Preventing the Spread of Mumps
Oral health professionals have an important role to play in reducing the prevalence of this virus.
This course was published in the June 2020 issue and expires June 2023. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define mumps.
- Identify reasons for the resurgence of mumps.
- Discuss prevention, diagnosis, and treatment of mumps.
The United States mumps (Rubulavirus) vaccination program began in 1967.1 Prior to its start, 186,000 cases were reported in the US each year.2 Since the program began, the reported number of mumps cases has decreased significantly.1 However, without immunization, the incidence of mumps is 100 to 1,000 cases per every 100,000 people, with epidemic outbreaks every 2 years to 5 years.3
Current recommendations for vaccination against mumps include two doses of measles, mumps, and rubella (MMR) beginning at age 1 year to 15 months. The initial dose provides individuals with a 78% immunity.1 A second dose of MMR is given between the ages of 4 and 6. With the second dose of MMR, immunity increases to 88%.1 However, mumps has not been eradicated from the US.4
The US is again experiencing a resurgence in the incidence of mumps. The US Centers for Disease Control and Prevention stated that from January 1 through December 6, 2019, more than 3,000 cases of mumps were reported in the US.2 Mumps tends to occur in populations in which close contact occurs such as in college settings. As the MMR vaccine is not completely effective in eliminating this disease, high vaccination coverage is necessary.2
As there are periods when mumps outbreaks are low, oral health professionals may not recognize the signs and symptoms of the disease. Further, mumps tends to occur more often in winter and spring. As such, the purpose of this article is to provide an update on the pathology of mumps and review oral health considerations for this disease.
PATHOLOGIC CONSIDERATIONS
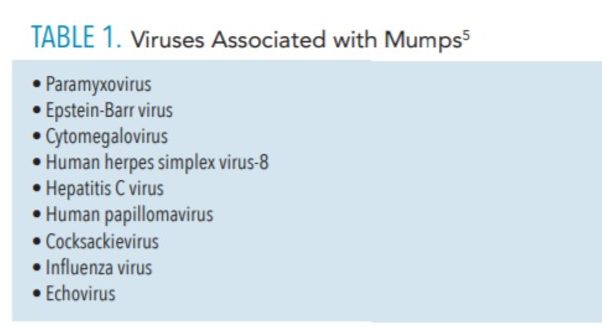
Mumps, also known as infectious parotitis or epidemic parotitis, is generally caused by the rubulavirus, which is within the genus paramyxovirus. Mumps can also be caused by other viruses in rare instances (Table 1). The virus is contained in a single stranded, negative strand of ribonucleic acid (RNA) consisting of 15,385 nucleotides encoding six structural proteins and at least two nonstructural proteins.5–7 This virus has two surface glycoproteins, one with hemagglutinin and neuraminidase activities and the other with cell fusion and cytolytic activities. These surface glycoproteins are responsible for fusion to the lipid membrane of the host cell membrane, which appears to be associated with neurovirulence.8,9 The mumps virus is susceptible to chemical disinfectants, such as ether, formalin, and alcohol, as well as heat, and ultraviolet light, all of which inactivate it.6,7
Mumps is a highly contagious infection known only to humans. Transmission of the virus occurs by direct contact, droplet spread, or via fomites (inanimate objects that can carry infection). The incubation period is approximately 16 days to 18 days and infected patients become most contagious 1 day to 2 days before the onset of clinical symptoms. The virus can be isolated from saliva as early as 7 days before and until 9 days after the onset of clinical symptoms.6,7,10
The virus enters the upper respiratory tract through inhalation of droplets, spreads to regional lymph nodes, replicates, and spreads through the blood to salivary and other glands. As the mumps virus infects salivary glands, edema and inflammation occur, leading to the classic presentation of pain and swelling. Although the parotid glands are often the most affected organs, parotitis is not a necessary component for mumps infection. Mumps virus can spread to other sites including the central nervous system (CNS), testes, ovaries, pancreas, and urinary tract system.6,8,11,12
Risk factors for mumps include lack of immunization, travel outside of the United States, and immune deficiencies. Most cases of mumps occur in school-aged children. Males and females are equally affected with parotitis, although males have a higher predilection for CNS involvement with a 3:1 ratio.6
CLINICAL PRESENTATION
Infections with mumps may be asymptomatic in 20% to 30% of individuals. Those suspected of having mumps tend to present with prodromal symptoms such as low-grade fever, malaise, headache, anorexia, and myalgia. These symptoms can last for 3 days to 5 days.6,7,11 After this prodromal period, the clinical course depends on the path of the virus and which organs are affected. The most common is a painful parotitis or swelling of the parotid gland, which occurs in 30% to 40% of all patients. The patient is considered to be infectious from approximately 3 days before the onset of active parotitis and up to 4 days after facial swelling is apparent.6
Pain, swelling, and fever are clinical characteristics of parotitis. Tenderness of the parotid gland, trismus, edema of Stensen’s ducts, parotid enlargement obscuring the mandibular angle, and superolateral lifting of the ear may be observed; these findings are best viewed from behind the patient. In addition, patients may complain of increased pain with chewing or when the salivary glands are stimulated by food and liquids. After several days, the swelling affects the contralateral gland in 70% to 75% of cases.5,12 Involvement of the submental and submandibular glands occurs in approximately 10% of cases. Serum amylase concentrations are elevated with parotitis inflammation.5–7 Parotid symptoms resolve within 7 days to 10 days.
Because mumps is a systemic infection, other sites of viral infection may be apparent. CNS involvement is the next most common extrasalivary complication of mumps manifesting as mumps meningitis or aseptic meningitis and, more rarely, encephalitis. Mumps meningitis occurs three times more frequently in males than females, and usually presents within 1 week to 2 weeks of parotid swelling. Symptoms include high fever, headache, vomiting, neck stiffness, and lethargy. The mumps virus can be isolated from cerebrospinal fluid early in the illness. Prognosis for either mumps meningitis or encephalitis is good, and complete recovery is expected.6,7
Another neurological complication of mumps is neuritis of the auditory nerve, which may lead to sensorineural deafness. Permanent hearing loss is preceded by symptoms including tinnitus, ataxia, vertigo, and vomiting. Although deafness may be considered a rare complication of mumps infection, a study by Hashimoto et al13 found that the incidence of hearing loss in children due to mumps was higher than previously reported.
Mumps infection can also affect the gastrointestinal system, causing acute pancreatitis. Symptoms include midabdominal pain, distention, low-grade fever, nausea, and vomiting. An elevated serum lipase value will be found in these cases.6
The genitourinary system is also notably impacted by the mumps virus. Approximately 20% to 30% of post-pubertal males develop unilateral orchitis or swelling of the testicles associated as a complication of mumps infection.5 This condition may occur before, during, or after parotitis. Symptoms include fever, chills, headache, vomiting, swelling, and testicular pain, erythema of the scrotum, and tenderness that can persist for weeks after other symptoms resolve.5–7 Bilateral orchitis occurs less frequently. Gonadal atrophy may occur, however sterility is rare.14 A study of patients with bilateral mumps orchitis treated with subcutaneous interferon alfa-2b for 1 week showed patients experienced resolution of their symptoms during that time and normospermia by the 6-month follow-up.15 Correspondingly, for women, oophoritis, or inflammation of the ovary, occurs in approximately 7% of post-pubertal females with mumps. Presenting symptoms include lower abdominal pain, fever, and vomiting; infertility is rare.5–7
Other less common complications of mumps include mastitis, myocarditis, arthritis, mild renal impairment, and thyroiditis.5,6,16 Hepatitis, acalculous cholecystitis, and thrombocytopenia are rare manifestations of mumps.7
DIFFERENTIAL DIAGNOSIS
The diagnosis of mumps is usually made based on clinical presentation and history of exposure to the virus.8,11 However, in many cases salivary gland swelling is not readily apparent and there may be widely varying constitutional mumps symptoms. A study investigating the clinical acumen of physicians’ abilities to diagnose mumps revealed that their diagnostic accuracy was poor based solely on clinical presentation. Findings showed that only 14% of 2,082 cases could be confirmed by laboratory analysis during a mumps outbreak.17 Therefore, laboratory testing is recommended for definitive diagnosis.7,8
Mumps virus is generally measured by serology, viral culture, or polymerase chain reaction assays generally measuring immunoglobulin M antibody concentrations. The virus can be readily isolated from saliva, cerebrospinal fluid, urine or seminal fluid within the first week of symptom presentation.7 Detection of antibody levels can provide information about when an individual was infected while detection of IgG indicates prior exposure to mumps, but not necessarily immunity.18,19
There are other causes of parotid gland swelling, including occlusion of salivary flow by a sialolith, bacterial infection referred to as bacterial sialadenitis, and viral infections (Table 1, page 33). Juvenile recurrent parotitis is a recurrent idiopathic, inflammatory condition that may occur three times to four times per year presenting with pain, fever, malaise, and parotid swelling in children. Symptoms may be unilateral or bilateral and are self-limiting.7 Other considerations for parotitis include: mastoiditis, drug reactions (thiazide diuretics), allergic reactions, tumors and cysts, metabolic disorders (diabetes, cirrhosis, uremia), Sjögren syndrome, and Mikulicz syndrome.
TREATMENT AND PROGNOSIS
Individuals diagnosed with mumps should be isolated from others for 5 days from the onset of symptoms to minimize the risk of spreading infection.5,6 Mumps is self-limiting and treatment is primarily supportive and conservative. Oral fluid intake to maintain adequate hydration; eating soft foods to prevent pain with chewing; avoiding acidic foods and liquids that increase salivation, cause swallowing difficulty and gastric irritation; taking ibuprofen or acetaminophen to relieve headaches and discomfort due to parotitis; and applying cold packs to swollen glands are recommended.6,16 Steroids are not recommended for the treatment of orchitis as this medication may facilitate, rather than alleviate, testicular atrophy.20
Most cases of mumps are uncomplicated and resolve without incident. Patients with specific complications, such as meningitis, encephalitis, myocarditis, nephritis, or severe pancreatitis, require a higher level of supportive care including inpatient hospitalization with intravenous fluid stabilization, pain management, and continuous close observation.6 In most cases, recovery is expected within 2 weeks to 3 weeks, and the prognosis is generally favorable. Death due to mumps is rare.
PREVENTION STRATEGIES
Like several communicable diseases, mumps prevention relies heavily on herd immunity, which is achieved through vaccination. Herd immunity occurs when a large proportion of the community is immune to the communicable disease. The threshold for mumps herd immunity varies between 75% and 86%.21 This broad window may leave room for spikes in the disease activity. However, even when herd threshold is at the optimal range, outbreaks still occur, particularly in settings where people are in close contact with one another for extended periods such as in elementary, middle, and college and university settings.2,22,23 These continued outbreaks suggest that there is a lack of understanding of when primary vaccine failure occurs.23
VACCINE CONSIDERATIONS
Today, parents may refuse or delay having their child vaccinated against preventable communicable disease. Omer et al24 found that this phenomenon is due to a perceived association between vaccines and autism, even though this association is refuted by scientific evidence.25 In addition, as the incidence for disease outbreaks decline, parents may feel the disease is no longer severe or that their child is not susceptible, which may lead to vaccine refusal.24,26
Each state is responsible for determining the immunization requirements as well as the reasons for exemption from vaccination. Omer et al24 found that between 1991 and 2004, only 1% of states allowed religious exemptions. However, when states accepted exemption from vaccination for philosophical or personal beliefs exemption rates increased from 0.99% to 2.54%. When nonmedical exemptions (NME) increase, herd immunity may be affected, which could increase the risk for medically exempt children to contract these communicable diseases.24
SECONDARY VACCINE FAILURE
Several studies have suggested that mumps immunity wanes over time. Cardemi et al27 studied an outbreak of mumps at the University of Iowa in 2015. In 2012, the University of Iowa instituted a vaccination requirement for students. Students were required to submit vaccine records showing two doses of the MMR vaccine or provide a medical or religious exemption form. When the mumps outbreak occurred, researchers found that students who had received the second dose of the MMR vaccine within 12 years had a lower attack rate than those who had received the second dose13 years or more before the outbreak.27 When the second dose of MMR was given 13 years to 15 years previous to the outbreak occurring, 11.3 cases per 1,000 were diagnosed with mumps as compared to 17.6 cases for those who had received the second dose 16 years to 23 years prior. These students were 9.1 times and 14.3 times more likely to contract mumps respectively. In cases such as this, at-risk individuals should receive a third dose of the vaccine.1 This added measure led to a 78% reduction in risk for contracting mumps. However, at 1-year post vaccination, titers for these students had returned to pre-vaccination level, which indicates that the third dose, is at best, a temporary fix to control the outbreak.23
PREVENTION AND POST-EXPOSURE PRECAUTIONS
Oral health professionals need to thoroughly assess their patients’ medical histories to prevent the potential spread of communicable diseases. Full medical histories, with immunization records,28,29 should be taken at the beginning of the dental appointment and reviewed thereafter for accuracy. This information provides essential details needed for the safe treatment. Healthcare providers, including oral health professionals, may play an important role in vaccination education.24 Therefore, it is important to include vaccine records in the patients’ health history evaluation.28,29
As previously discussed, parotitis is one of the first clinical symptoms of mumps. Additionally, some patients will experience pain when chewing, which may lead the patient to seek dental treatment. When patients enter the office displaying these symptoms, good infection control practices must be in place. These practices should include masks in the waiting room as well as hand sanitizer to prevent disease spread.
If mumps is suspected, the patient should be advised that dental treatment must be postponed until he or she is no longer infectious.30 The patient should be advised to isolate at home for 5 days and seek medical advice from his or her primary care physician. The potential case must be reported to the state or local health department, as mumps is a notifiable disease.5,31
All healthcare providers, including oral health professionals, must be immunized when possible against this communicable disease. Dental offices should have an accurate immunization record for all employees. In cases where the employee has previously been exposed to mumps, there should be documentation in the employee file, demonstrating evidence of immunity.32
CONCLUSION
Mumps is a highly contagious, yet poorly understood infection that is re-emerging in the US. To prevent the spread of mumps, oral health professionals need to be familiar with the systemic symptoms of this disease. The dental team must be aware of the appropriate prevention and post-exposure precautions. Furthermore, as a healthcare provider, it is the responsibility of the clinician to support and advocate for patient vaccination in order to reduce the prevalence of mumps in the US.
REFERENCES
- United States Centers for Disease Control and Prevention. Mumps Vaccination. Available at: cdc.gov/mumps/vaccination.html. Accessed May 26, 2020.
- US Centers for Disease Control and Prevention. Mumps Cases and Outbreaks. Available at: cdc.gov/mumps/outbreaks.html. Accessed May 26, 2020.
- World Health Organization. Weekly Epidemiologic Record. Available at: who.int/immunization/wer8207mumps_Feb07_position_paper.pdf?ua=1. Accessed May 26, 2020.
- The College of Physicians of Philadelphia. Mumps. Available at: historyofvaccines.org/content/articles/mumps. Accessed May 26, 2020.
- Lau RK, Turner MD. Viral mumps: increasing occurrences in the vaccinated population. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128:386–392.
- Defendi GL. Mumps. Available at: medscape.com/article/966678-print. Accessed May 26, 2020
- Hviid A, Rubin S, Mühlemann K. Mumps. Lancet. 2008;15:932–944.
- McAdam AJ, Milner DA, Sharpe AH. Infectious diseases. In: Kumar V, Abbas AK, Aster JC, eds. Robbins and Cotran Pathologic Basis of Disease. 9th ed. Philadelphia: 2015;355–356.
- Tecle T, Johannsson B, Yun Z., et al. Antigenic and genetic characterization of the fusion (F) protein of mumps virus strains. Archives of Virology. 2000;145:1199–1210.
- Ennis FA, Jackson D. Isolation of virus during the incubation period of mumps infection. J Pediatr. 1968;72:536–537.
- Delong L, Burkhart N. General and Oral Pathology for the Dental Hygienist. 3rd ed. Philadelphia: 2019;404-405.
- Regezi JA, Sciubba JJ, Jordan RCK. Oral Pathology: Clinical Pathologic Considerations. 7th ed. St. Louis: 2017;191.
- Hashimoto H, Fujioka M, Kinumaki H. An office-based prospective study of deafness in mumps. Pediatr Infect Dis J. 2009;28:173–175.
- Dejucq N, Jégou B. Viruses in the mammalian male genital tract and their effects on the reproductive system. Microbiol Mol Biol Rev. 2001;65:208–231.
- Jin L, Orvell C, Myers R, et al. Genomic diversity of mumps virus and global distribution of the 12 genotypes. Rev Med Virol. 2015;25:85–101.
- Grennan D. Mumps. JAMA. 2019;322:1022.
- Hatchette RF, Mahony JB, Chong S, et al. Difficulty with mumps diagnosis:what is the contribution of mumps mimickers? J Clin Virol. 2009;46:381–383.
- World Health Organization. Weekly Epidemiology Record. Available at: who.int/wer/2012/wer8709/en/. Accessed May 26, 2020.
- Rota JS, Rosen JB, Doll MK, et al. Comparison of the sensitivity of laboratory diagnostic methods from a well-characterized outbreak of mumps in New York city in 2009. Clin Vaccine Immunol. 2003;20:391–396.
- Lane TM, Hines J. The management of mumps orchitis. BJU Int. 2006;97:1–2.
- Livingston KA, Rosen JB, Zucker JR, Zimmerman CM. Mumps vaccine effectiveness and risk factors for disease in households during an outbreak in New York City. Vaccine. 2014;32:369–374.
- Pike J, Marin M, Guo A, Haselow D, Safi H, Zhou F. 2016-2017 Arkansas mumps outbreak in a close-knit community: Assessment of the economic impact and response strategies. Vaccine. 2020;38:1481–1485.
- Ramanathan R, Voigt EA, Kennedy RB, Poland GA. Knowledge gaps persist and hinder progress in eliminating mumps. Vaccine. 2018;36:3721–3726.
- Omer SB, Salmon DA, Orenstein WA, DeHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable disease. NE J Med. 2009;360:1981–1996.
- DeStefano F. Vaccine and autism: evidence does not support a causal association. Clin Pharmacol Ther. 2007;82:756–759.
- Smith PJ, Humiston SG, Marcuse EK, et al. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the health belief model. Public Health Rep. 2011;2:135–146.
- Cardemil CV, Dahl RM, James L, et al. Effectiveness of a third dose of MMR vaccine for mumps outbreak control. NE J Med. 2017;377:947–956.
- Record keeping. Reference Manual of Pediatric Dentistry. Chicago: American Academy of Pediatric Dentists; 2019-2020:431–438.
- Hicks J, Flaitz CM. Role of the pediatric dentist in optimization of childhood immunization. Ped Dent. 1996;18:395–398.
- Ogle OE. Salivary gland diseases. Dent Clin North Am. 2020;64:87–104.
- US Centers for Disease Control and Prevention. For Healthcare Providers. Available at: cdc.gov/mumps/hcp.html. Accessed May 26, 2020.
- US Centers for Disease Control and Prevention. Manual for the Surveillance of Vaccine-Preventable Diseases. Available at: cdc.gov/vaccines/pubs/surv-manual/chpt09-mumps.html#hcp-settings. Accessed May 26, 2020.
From Dimensions of Dental Hygiene. June 2020;18(6):32-35.



