Treating Patients With Von Willebrand Disease
Maintaining oral health is paramount for individuals with this blood clotting disorder.
This course was published in the July 2015 issue and expires July 31, 2018. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define von Willebrand disease (VWD).
- Identify the signs and symptoms of this disease.
- Discuss the clinical implications of VWD on oral health.
- Explain the protocol for providing comprehensive oral health care to patients with this blood clotting disorder.
While VWD can be acquired, it is most commonly inherited. The genetic etiology is autosomal; thus, VWD is found in equal proportions among men and women.4 VWD is biochemically characterized by a reduction or abnormality in a glycoprotein known as von Willebrand factor. Defective or decreased concentrations of von Willebrand factor result in less vigorous adhesion of blood platelets to injured blood vessel walls, thereby increasing bleeding times.4 VWD affects approximately 1% to 2% of the population.
There are several types of VWD (Table 1), all of which are diagnosed by a hematologist. Type I VWD is the most common and accounts for approximately 80% of cases; it is also the mildest type.4,6 Individuals with type II (A, B) and type III do not have any von Willebrand factor, while individuals with type II (M and N) have normal levels of von Willebrand factor. Factor replacement products are used to treat those patients who do not have any von Willebrand factor.4 Type II and type III exhibit symptoms similar to moderate hemophilia.
Diagnostic testing for VWD is reliable in both high sensitivity and specificity, but the precise type and severity of VWD may not be well defined by diagnostic tests.7 Also, individuals with VWD may be asymptomatic and go undiagnosed.4 The inconclusive typing of the true severity of an individual’s disease status often compels dental professionals to rely on clinical manifestations and oral symptoms to determine an appropriate treatment plan.
SIGNS AND SYMPTOMS
Symptomatic individuals with VWD customarily present with mucosal bleeding, including epistaxis; generalized easy bruising; gastrointestinal tract or genitourinary bleeding; menorrhagia (heavy menstrual bleeding) in women; and anemia.4 Oral manifestations may include petechiae, ecchymoses, excessive gingival bleeding, and oral hematomas.8 Extraorally, multiple purpura of the epidermis, open or bleeding wounds, hematomas, and swollen joints may be present.8 Individuals with VWD are at increased risk of allergic reaction to the factor replacement products used to replenish the missing von Willebrand factor. Synovitis (joint inflammation) and systemic diseases due to factor replacement through blood transfusion can also occur.8 Table 2 presents additional VWD signs and symptoms.9,10
Women with VWD often experience menorrhagia and may be prescribed a combination of pharmacotherapies, including the combined oral contraceptive pill and intrauterine progestogen-only contraceptive.5 The thromboembolic properties of oral contraceptives can create an increased risk of myocardial infarction and hypertension.11 Oral complications caused by the combined oral contraceptive pill and intrauterine progestogen-only contraceptive pill include increased occurrence of localized osteitis, xerostomia, gingival inflammation, and hyperplasia, despite adequate self-care.11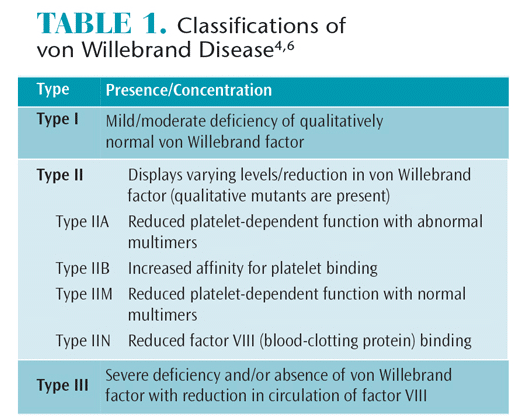
CLINICAL IMPLICATIONS
In order to prevent a medical emergency, patients should be screened for possible clotting disorders. Health history questions may include whether the patient has experienced unusual bleeding episodes after surgery or dental treatment, noticed spontaneous bleeding, or experienced easy/frequent bruising. A clinically significant bleeding episode is one that continues beyond 12 hours, causes the patient to return for further treatment, results in the development of a hematoma or ecchymosis, and/or requires blood product infusion.9
Dental care for individuals with VWD includes a comprehensive medical and dental health history review, including the documentation of vital signs; oral health screening; notation of current prescription therapies and allergies to any drugs used in dental care; assessment of the potential for substance abuse; and identification of other potential intrinsic diseases.8 The invasiveness of the planned procedure and the potential for prolonged bleeding post-operatively are important considerations when treatment planning.8 The assessment incorporates the type of VWD, symptoms manifested, proposed treatment, and collaboration with the patient’s hematologist to determine if a factor replacement blood transfusion is recommended pre- or post-treatment.4,8,9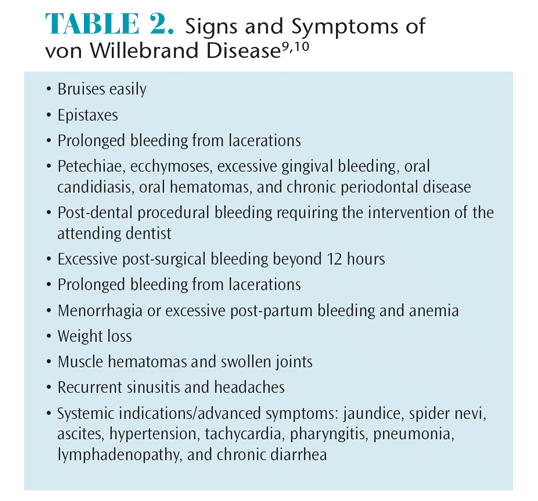
A full radiographic survey with routine follow-up bitewing and periapical X-rays can be performed on a case-by-case basis.12 Caries, oral cancer, and periodontal risk assessment should be conducted at the initial dental hygiene visit and a personalized treatment plan should be developed based on the findings.9,13
Definitive diagnosis of VWD, including an assessment of severity, is made by the patient’s hematologist.14 Dental hygienists, however, can assess for signs and symptoms that suggest VWD, including the patient’s personal and family health history and any indication of prolonged bleeding in the past.9 A referral for consultation and potential diagnostic testing can ensue based on these findings. Close collaboration with the hematologist remains the single most important element in management of patients with VWD.4,8
A treatment plan should be implemented immediately in patients with VWD (as well as other bleeding disorders) who elicit poor oral hygiene to prevent further damage to periodontal tissues.15 The use of topically applied antibacterial agents, such as chlorhexidine gluconate and/or antibiotics, prior to invasive dental procedures may reduce infection and inflammation.15 In addition to traditional caries and periodontal interventions, the treatment plan may include a referral to a registered dietitian for nutrition analysis and possible treatment—as anemia and vitamin deficiency also may be contributing factors for gingivitis and periodontitis.16
Pharmacotherapeutics prescribed to prevent prolonged bleeding episodes during invasive procedures include antihemophilic (encourage clot formation) and antifibrinolytic (prevent clot breakdown) agents. Depending on the severity and type of VWD, the hematologist may recommend these agents alone or in combination prior to and post-treatment.6 Antifibrinolytic agents can be used in conjunction with desmopressin for invasive dental work (Table 3).4,8 For the approximately 20% of patients who are unresponsive to desmopressin, a standard local therapy application of tranexamic acid and a fibrin glue (attaches tissue together) with the desmopressin therapy is recommended.6 The use of fibrin glue in conjunction with standard treatments was found to reduce the need for concentrates and prevent bleeding complications during oral surgery in the majority of study patients. Therefore, these post-operative recommendations may help prevent the need for a factor replacement blood transfusion post-treatment.6
The best strategy to prevent a prolonged bleeding episode is consistent, routine oral examination and prophylaxis so that biofilm and inflammatory levels are kept to a minimum.4,8 Most patients with VWD are at moderate to severe caries risk due to their medication use and tendency to bleed.9,13,15 As such, oral health professionals may recommend: consumption of fluoridated drinking water; application of topical fluoride varnish every 3 months to 6 months; use of xylitol chewing gum to increase salivary flow; and daily use of a fluoride dentifrice with a power toothbrush.13,17 Caries prevention is critical so as to avoid the need for invasive dental procedures that can put patients with VWD at elevated risk for a prolonged bleeding episode.9,15
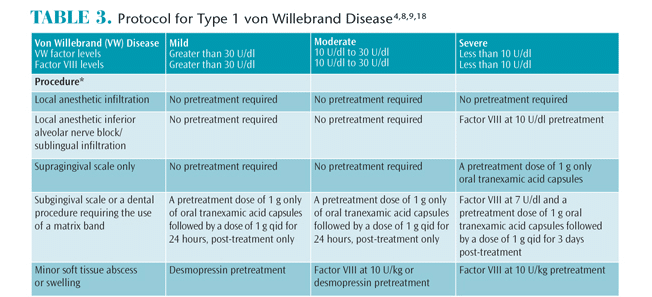
Patients with VWD also should maintain excellent periodontal health because gingival inflammation can lead to increased bleeding.9 The periodontal treatment plan should be individualized with the primary focus on the prevention of gingival inflammation.9,18 Antiseptic mouthrinses may help reduce biofilm and inflammation.9 Periodontal probing measurements, supragingival scaling, and coronal polishing generally can be accomplished with little to no risk of significant bleeding.9 Subgingival scaling and root planing and other invasive procedures can be performed based on a collaborative treatment plan involving the recommendation of the patient’s hematologist (Table 3).4,8,9,18 The use of ultrasonic instrumentation may reduce the risk of increased bleeding and tissue trauma.9 For periodontal tissues with severe inflammation, edema, and erythema, gross debridement prior to deep scaling or root planing is advised.9 Depending on the outcome of treatment, a referral for periodontal surgery may be needed. A high-dose regimen of cholecalciferol 50,000 IU daily for 10 days can be recommended, as well as a continuous low dose vitamin D regimen to support periodontium health.16
Although the risk is extremely low with modern single-use needles, submucosal infiltration during the administration of local anesthesia can cause hematomas in patients with VWD and should be used only after discussion with the patient’s hematologist.15 Specifically, the use of nerve blocks, especially those involving the inferior alveolar nerve and infiltration of the lingual/floor of the mouth, should be avoided due to the possibility of airway obstruction should hematoma occur in the retromolar or pterygoid space.8 To reduce this risk, intraligament and intrapapillary injections with the use of articaine and/or an anesthetic containing a vasoconstrictor can be used.3,15 Administering nitrous oxide sedation should also be considered as a noninvasive, low-risk pain control adjunct.15
Ongoing evaluation of the patient’s reaction to treatment procedures is vital to maintaining homeostasis. In addition, communication with the patient and family members on the perception of the treatment outcome is imperative to planning any future procedures. All information regarding the patient’s treatment outcomes should be communicated to his or her hematologist upon completion of treatment.
Accurate, consistent, and thorough interprofessional communication is necessary when treating patients with VWD. Proper documentation of health history, clotting disorder signs and symptoms, drug therapy, hematology consultation, and planned treatment is imperative. Without this detailed record, other health care providers will be hampered in their ability to treatment plan for the patient.
ADDITIONAL CONSIDERATIONS
The location and position of the third molars should be ascertained in the early teen years, so early extraction may be considered in order to avoid the need for more extensive procedures in the future.14 If wisdom tooth extraction is indicated, an infusion of factor replacements prior to and several days after, in addition to antifbrinolytic therapy is a recommended preventive measure.14 Natural exfoliation with pressure and ice is preferred for primary teeth. The extraction of primary teeth, however, may be indicated for patients with a history of prolonged bleeding. Hospitalization should be considered for extensive dental procedures such as surgical, impacted, and multiple extractions, periodontal surgery, and treatments requiring sutures.4
During dental treatment, measures should be taken to reduce mucosal trauma with careful use of the saliva ejector. Special care is recommended while taking radiographs and impressions and during the use of rubber dams to protect surrounding tissues.15 The use of cautery for invasive operative procedures is recommended. The utilization of a diode laser in both nonsurgical periodontal procedures and oral surgical procedures reduces patient discomfort, operative and post-operative bleeding, and scarring.19
Post-operative drugs that may interfere with platelet function, such as aspirin, must be avoided, and nonsteroidal anti-inflammatory agents should be used with caution.4 The World Federation of Hemophilia recommends the use of acetaminophen with or without codeine for pain control and cites the potential for drug interactions when multiple medications are prescribed.4 A custom mouthpiece may offer local compression in the area where post-operative bleeding is expected.7 Applying pressure with gauze, resting, administering ice to the treatment area, and compression and elevation can minimize post-operative bleeding.9
CONCLUSION
Dental and dental hygiene management of patients with VWD can be accomplished after careful collaboration with their hematologists. Prevention of a bleeding episode can be managed via thorough assessment of an accurate health history, patient’s medication use, pain management needs, and appropriate post-treatment measures. Implementation of this treatment plan will help prevent a potential medical emergency and limit the need for future extensive dental treatment, as well as improve oral and overall health and well-being for individuals with VWD.
REFERENCES
- Bucciarelli P, Siboni SM, Stufano F, et al. Predictors of von Willebrand disease diagnosis in individuals with borderline von Willebrand factor plasma levels. J Thromb Haemost. 2015;13:228–236.
- Von Willebrand EA. Hereditar pseudohemofili. Finska Lakarsallskapets Handl. 1926;67:7–112.
- Kalsi H, Nanayakkara L, Pasi KJ, Bowles L, Hart DP. Access to primary dental care for patients with inherited bleeding disorder. Clin Haematol. 2012;18:510–515.
- World Federation of Hemophilia. Protocols for the Treatment of Hemophilia and Von Willebrand Disease. Available at: 1.wfh.org/publication/files/pdf- 1137.pdf. Accessed June 9, 2015.
- Kujovich JL. Von Willebrand’s disease and menorrhagia: Prevalence, diagnosis, and management. Am J Hematol. 2005;79:220–228.
- Franchini M, Rossetti G, Tagliaferri A, et al. Efficacy and safety of factor VIII/von Willebrand factor concentrate (Haemate-P®) in preventing bleeding during surgery or invasive procedures in patients with von Willebrand’s disease. J Hematol. 2003;88:1279–1282.
- Costa-Pinto J, Perez-Rodriguez A, Gomez-del- Castillo MDC, et al. Diagnosis of inherited von Willebrand disease: Comparison of two methodologies and analysis of the discrepancies. Haemophil. 2014;20:559–567.
- Stubbs M, Lloyd J. A protocol for the dental management of the patient with von Willebrand’s disease, haemophilia A, and haemophilia B. Austr Dent J. 2001;46:37–44.
- Gupta A, Epstein JB, Cabay RJ. Bleeding disorders of importance in dental care and related patient management. J Can Dent Assoc. 2007;73:77–83.
- Lillicrap D, James P. Von Willebrand disease: An introduction for the primary care physician. Available at: 1.wfh.org/publication/files/pdf- 1204.pdf. Accessed June 9, 2015.
- Mayo Clinic. Von Willebrand disease. Available at: mayoclinic.org/diseases-conditions/von-willebranddisease/ basics/definition/con-20030195. Accessed June 9, 2015.
- American Dental Association and United States Department of Health and Human Services. Dental radiograph Examinations: Recommendations for Patient Selection and Limiting Radiation Exposure. Available at: ada.org/sections/professional Resources/pdfs/Dental_Radiographic_Examinations_ 2012.pdf. Accessed June 9, 2015.
- American Dental Association, & Council on Scientific Affairs. Non-Fluoride Caries Preventive Agents: Full Report of a Systematic Review and Evidence-Based Recommendations. Available at: ebd.ada.org/contentdocs/clinical_recommendations_ non_fluoride_caries_preventive_agents_full_report.pd f. Accessed June 9, 2015.
- Morimoto Y, Yoshioka A, Sugimoto M, Imai Y, Kiritia T. Haemostatic management of intraoral bleeding in patients with von Willebrand disease. Oral Dis. 2005;11:243–248.
- Australian Haemophilia Centre Directors’ Organization. A Consensus Statement on the Dental Treatment of Patients With Inherited Bleeding Disorders. Available at: ahcdo.org.au/sitebuilder/ publications/knowledge/asset/files/16/dentalguidelin esforwebsitedec10.pdf. Accessed June 9, 2015.
- Hacman KL, Gagnon C, Briscoe RK, Lam S, Anpalahan M, Ebeling PR. Efficacy and safety of oral continuous low-dose versus short-term high-dose vitamin D: A prospective randomized trial conducted in a clinical setting. Med J Austr. 2010;192:686–689.
- American Dental Association. Professionally applied topical fluoride: Evidence-based clinical recommendations. J Am Dent Assoc. 2006;137:1151–1159.
- Nickles K, Wohlfeil M, Alesci S, Miesbach W, Eickholz P. Comprehensive Treatment of Periodontitis in Patients With von Willebrand Disease. J Periodontol. 2010;81:1432–1440.
- Amid R, Kadkhodazadeh M, Ardakani MRT, et al. Using diode laser for soft tissue incision of oral cavity. Journal of Lasers in Medical Sciences. 2012;3(1):36–43.
From Dimensions of Dental Hygiene. July 2015;13(7):41–44.



