
Minimally Invasive Periodontal Surgery Revisited
The addition of a videoscope to this technique provides benefits for both clinicians and patients.
This course was published in the October 2013 issue and expires 10/31/16. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the incidence and etiology of child abuse and
neglect. - Define minimally invasive periodontal surgery (MIS).
- Explain the purpose of the videoscope in MIS.
- Discuss the effects of MIS with the videoscope on treatment outcomes.
While modern regenerative surgery has greatly reduced the level of discomfort and negative esthetic changes that may occur following periodontal surgery, it is still viewed with trepidation by some patients. This same concern influences the referral of patients for regenerative surgery. When isolated deep pockets remain following nonsurgical periodontal therapy, oral health professionals are often apprehensive about referring patients to a periodontist for surgical treatment of localized areas. The concern is that the treatment of the deeper sites will cause post-surgical pain, cold sensitivity, and recession around teeth that have been previously rendered stable through nonsurgical therapy.
MINIMALLY INVASIVE PERIODONTAL SURGERY
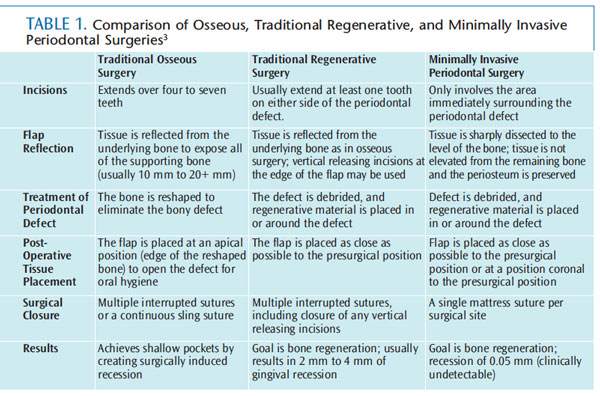
Minimally invasive periodontal surgery (MIS) is a surgical technique designed to reduce the negative effects of periodontal surgery.1,2 Table 1 provides a comparison of osseous surgery, traditional regenerative surgery, and MIS.3
The essence of MIS is to promote the regeneration of lost bone, periodontal ligament, and connective tissue utilizing very small incisions, minimal reflection of tissue, maintenance of blood supply, and restricting the surgery only to areas of localized, deeper pockets. Short incisions (3 mm to 4 mm in length) are employed, and the incisions are not extended into the adjacent healthy tissue. Rather, incisions might be confined to the palatal or lingual aspect of the surgical site, allowing for the maintenance of the facial tissues—thus limiting or eliminating recession following surgery.
MIS is usually well tolerated by patients, as there is minimal morbidity following the procedure. Patients often report little or no pain. This is reflected in minor changes in patient activity following surgery. In most cases, there is no need for prescription pain medication (acetaminophen or ibuprofen is recommended), and no need to alter chewing habits.4 Patients may resume most typical activities of daily living 1 day post-surgery. Food that is moderately firm can be consumed in the surgical area within 1 day to 2 days, while the chewing of hard foods may resume within 1 week to 2 weeks. A common side effect of traditional periodontal surgery—cold sensitivity—is rare with MIS, and the use of desensitizing agents is not usually needed.4 In fact, many patients attest that it feels as if nothing was done. This may be due to MIS typically being performed from the lingual or palatal aspect, making it more difficult for patients to see the surgical site without the use of a dental mirror.

The results following MIS are, in most cases, better than those reported for traditional regenerative surgery. In a study of 142 sites that were originally 6 mm to 12 mm deep after root planing, all pockets had a mean depth of 3.09 mm immediately following MIS.5,6 At 1-year post-surgery, all pockets maintained the 3.09 mm mean depth, with all pockets less than 4 mm. When these sites were re-evaluated 6 years post-operatively, the mean pocket depth was 3.06 mm, with all pockets remaining less than 4 mm. The 6-year data actually showed slight improvement over the 1-year data. There was no indication of deepening pockets or a return of active periodontal diseases over time. At both 1-year and 6-year postoperative reevaluations, there was no clinically detectable recession in the surgical areas (mean recession of 0.01 mm).5,6
A subset of data from a large university based clinical study of MIS using a videoscope for visualization has recently been published.7 This study, at 6 months post-treatment, showed a mean pocket depth of 2.5 mm with an increase in gingival height. This demonstrates that the post-surgical pocket depth was ideal after MIS. Rather than recession of the gingival tissue with negative esthetic implications, improvement was gained in tissue height where presurgical recession had existed.
VISUALIZATION
MIS yields favorable post-surgical results, induces little or no gingival recession, and causes minimal post-surgical discomfort.4–6 Despite these excellent results, traditional, large-incision periodontal regenerative surgery remains a routine method for delivering regenerative periodontal treatment. One of the major reasons for this is the difficulty in visualizing the periodontal defect when small-incision surgery is used. Traditionally, MIS has been performed with either highpower surgical telescopes (loupes) or a surgical microscope, neither of which is ideal.
Recently, a videoscope has been developed for use in MIS. A videoscope is a surgical instrument that has a camera at the end of the scope that transmits a digital image to an external video monitor (Figure 1). This is different from an endoscope, which has optical fibers in the body of the scope that transmits a picture to an external camera. The videoscope provides higher quality images and is significantly more flexible than a traditional endoscope.
The instrument for directing the videoscope into the small surgical opening of MIS incorporates a carbon fiber retractor, as well as a device that prevents the camera from becoming obscured by blood or debris from the surgical site. This device also allows for the elimination of water flow to the operating site. A previously developed endoscope designed for nonsurgical dental use required a constant flow of water to maintain visualization. The water flow was problematic because it clouded the image projected on the monitor. This new technology allows visualization in an air- or gas-filled surgical field during the MIS procedure. An air-filled field is safe,8 improves visualization, and makes patient management easier than when a liquid-filled field is used.

CASE STUDIES
This patient is a 45-year-old man with a long history of periodontal disease and treatment. Periodontal therapy consisting of nonsurigical root planing followed by traditional periodontal surgery had been performed approximately 8 years prior. The patient had been compliant with the recommended periodontal maintenance therapy on a 4-month basis. His only systemic factor was well-controlled hypertension.
His periodontal health was good, with the exception of two refractory molar sites. He had generalized pockets that were 3 mm to 4 mm with minimum inflammation. The two refractory interproximal molar sites had pockets of 7 mm to 8 mm, exhibiting moderate inflammation and bleeding on probing. The two sites had been treated with localized root planing several times since the initial periodontal treatment was performed. The patient stated that root planing “helped for a little while, but the pockets always came back.”
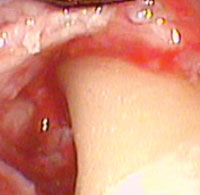
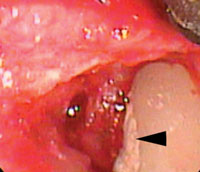
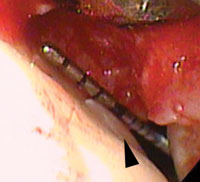
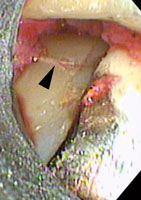
Small MIS access incisions were made on the lingual aspect of each site. Figure 2 shows the initial view of the pocketed areas. A layer of smooth, and apparently burnished, calculus covered the root surface. The calculus was undetectable with a periodontal probe. The root surface had the smooth feel of a calculus-free surface. The calculus was removed with a combination of curets and ultrasonic instrumentation under direct observation with the videoscope. Figure 3 shows the root surface following mechanical debridement. At this point, the root surface felt smooth and no calculus was visible using surgical telescopes (loupes). The videoscope view, however (Figure 3), revealed multiple tiny islands of apparent calculus (small white spots). Figure 4 shows the root surface after the use of ethylenediaminetetraacetic acid (EDTA) to biomodify the root surface. It appears that EDTA dissolved the near microscopic islands of calculus from the root surface. The other refractory site revealed an apparent cementoma on the root surface (Figure 5). This cementum abnormality was smooth when palpated with a periodontal probe. The excess cementum was easily removed with a diamond-coated ultrasonic tip under direct vision with the videoscope.
The second patient is a 50-year-old man in good health. He had multiple localized pockets greater than 6 mm. Moderate inflammation and localized bleeding on probing were associated with the deeper pockets. He had received nonsurgical periodontal therapy many times in the past, which consisted of multiple sessions of root planing with local anesthetic. Traditional periodontal surgical treatment had been recommended for the deeper sites, but the patient refused due to concerns about pain and esthetics. The patient had requested MIS.
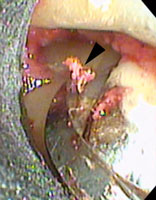
Small MIS access incisions were made between the maxillary molars. Multiple small islands of calculus were noted. The entire root surface was smooth when palpated with a periodontal probe. A vertical line of calculus was noted when the root was viewed with the videoscope. This line of calculus was not visible with surgical telescopes because of its position. This line of calculus had the clinical appearance of a root fracture (Figure 6). When the area was scaled with a curet, the calculus was removed, revealing a groove in the root surface (Figure 7). As further root planing was performed and the groove was removed, a healthy, smooth root surface was revealed (Figure 8). This type of groove in root surfaces associated with the deepest portion of the periodontal defect is often observed when the videoscope is utilized. It is not known if these grooves are developmental in nature or possibly caused by occlusal stress, but their association with areas of bone loss suggests that they may be an important part of the development of periodontal degeneration.
MINIMALLY INVASIVE SURGERY CHANGES ROUTINE PERIODONTAL THERAPY
Periodontal diseases are multifactorial, chronic, and inflammatory. In the day-to-day treatment of periodontal diseases, this means that the disease is never “cured.” At best, it is controlled by minimizing inflammation, which amounts to decreasing the risk factors that contribute to periodontal degeneration. Many risk factors are genetic or systemic in nature and are beyond the clinician’s or the patient’s ability to control. An example of this is the presence of a genetic risk factor inherent in the presence of a positive test for IL1ß.9 Some systemic risk factors, such as diabetes, can be partially controlled by diet and medication, but there is evidence that even patients with well-controlled diabetes are at greater risk for complications related to diabetes. This likely includes a greater risk for periodontal degeneration. Other risk factors related to lifestyle, such as smoking and level of oral hygiene, are, in theory, controllable or even reversible, but are often beyond the ability of the clinician to control. This leaves oral health professionals in the compromised and frustrating position of not being able to control all of the risk factors that influence patients’ periodontal diseases.
The risk factors that clinicians can influence are some of the local factors associated with periodontal diseases. Most periodontal treatment involves some method of reducing local factors that influence inflammation of the periodontium. The removal of plaque and calculus, and the reduction of pockets that harbor periodontal pathogens are at the heart of successful periodontal outcomes.
CONCLUSION

Dental hygienists are often the first oral health professionals to recognize periodontal diseases in a patient, and may even have the primary responsibility for the initial treatment. Nonsurgical treatment consisting of root planing, oral hygiene instruction, and placing the patient in a long-term maintenance program will frequently control periodontal diseases. There are often isolated sites, however, that do not completely respond to nonsurgical therapy. These isolated sites contain bacterial species that are associated with active periodontal diseases.10,11 Studies have shown that pockets of 5 mm or greater are more likely to worsen over time, and may lead to tooth loss.10,11 While it is sometimes possible to maintain these deeper pockets with repeated root planing and other nonsurgical therapy, the recreation of lost periodontal support with surgery that repairs the connective tissue attachment and regenerates lost bone gives a more desirable and long-lasting end result.12
Sites that cannot be controlled or maintained with nonsurgical treatment should be treated by regenerative surgery. If it is possible to regenerate periodontal supporting tissue and eliminate the pocket, this is the logical next step in treatment after root planing and a period of maintenance care. As discussed, however, the perception of periodontal surgery as being painful and disfiguring is a strong deterrent to taking the next steps necessary to achieve control over the risk factors for periodontal diseases.
The introduction of minimally invasive medical procedures has revolutionized the use of surgery for medical conditions. An example is the common procedure of gall bladder removal. Before the introduction of minimally invasive procedures, the surgical removal of a gall bladder was a major undertaking and included a week of hospitalization, 2 weeks in bed, and a minimum of 6 weeks away from work. A great deal of pain and discomfort was also associated with this procedure. Today, using minimally invasive approaches, the removal of a gall bladder can be performed as an outpatient procedure, with less than a week away from work, and minimal post-surgical pain. The use of MIS for regenerative periodontal procedures has similar advantages to minimally invasive medical procedures.
Oral health professionals have long been apprehensive about referring patients for periodontal surgery due to fears of patient discomfort and esthetically unacceptable recession. MIS, assisted by the videoscope, allows for surgery to be performed only in the area of the remaining isolated defect. This means that surgery will not be extended into the periodontally healthy areas, and generalized recession can be avoided. By using MIS, periodontal health does not need to be compromised by trying to maintain pockets deeper than considered healthy with the associated subgingival inflammation.
MIS represents a major step forward in the treatment of periodontal diseases and the regeneration of lost periodontal tissue. With greater accessibility to MIS treatment, it is now possible to bring patients to a state of full periodontal health without the negative sequela that has been associated with traditional periodontal surgery in the past.
References
- Harrel SK. A minimally invasive surgical approach for bone grafting. Int J Periodontics Restorative Dent. 1998;18:161–169.
- Harrel SK. A minimally invasive surgical approach for periodontal regeneration: surgical technique and observations. J Periodontol. 1999;70:1547–1557.
- Harrel K. Treating periodontal defects. Dimensions of Dental Hygiene. 2007;5(10):30–34.
- Cortellini P, Tonetti MS. Minimally invasive surgical technique and enamel matrix derivative in intrabony defects . I: Clinical outcomes and morbidity. J Clin Periodontol. 2007;34:1082–1088.
- Harrel SK, Wilson TG , Nunn ME. Prospective assessment of the use of enamel matrix derivative with minimally invasive surgery. J Periodontol. 2005;76:380–384.
- Harrel SK, Wilson TG , Nunn ME. Prospective assessment of the use of enamel matrix proteins with minimally invasive surgery: 6-year results. J Periodontol. 2010;81,435–441.
- Harrel SK, Wilson TG Jr, Rivera-Hidalgo F. A videoscope for use in minimally invasive periodontal surgery. J Clin Periodontol. 2013;40:868–874.
- Harrel, SK, Hidalgo-Rivera, F, Abraham C. Tissue resistance to soft tissue emphysema during minimally invasive surgery. J Contemp Dent Pract. 2012;13:886–891.
- Giannobile WV, Braun TM, Caplis AK, Doucette-Stamm L, Duff GW, Kornmann KS. Patient stratification for preventive care in dentistry. J Dent Res. 2013;92:694–701.
- Greenstein G . Contemporary interpretation of probing depth assessments: diagnostic and therapeutic implications. A literature review. J Periodontol. 1997;68:1194–1205.
- Greenstein G. Periodontal response to mechanical non-surgical therapy. J Periodontol. 1992;63:118–130.
- Grbic J, Lamster IB, Celenti RS, Fine JB. Risk indicators for further clinical attachment loss in adult periodontitis. Patient variables. J Periodontol. 1991;62:322–329.
From Dimensions of Dental Hygiene. October 2013;11(10):71–75.



