Alternative Avenues for Pain Management
These complementary therapies can help reduce the recurring musculoskeletal pain often experienced by clinical dental hygienists.
This course was published in the November 2013 issue and expires November 2016. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define musculoskeletal disorders.
- Identify the etiology of musculoskeletal disorders.
- Discuss how complementary therapies, such as chiropractic care, acupuncture, massage, and physical therapy, can help clinicians manage musculoskeletal pain.
After a long day at work, it’s not uncommon for dental hygienists to experience recurring pain in the hands, wrists, neck, shoulders, and back. These aches, however, may signal a greater problem, as many of these symptoms are caused by musculoskeletal disorders (MSDs). Defined as injuries to muscles, ligaments, tendons, nerves, blood vessels, bones, and joints, these problems may be related to one incident or multiple, repetitive, and cumulative injuries.1 MSDs may lead to pain in the neck, shoulders, arms, wrist, hands, and upper and lower back, in addition to the lower extremities.2 A systematic review of 23 studies revealed that MSDs are common among dentists and dental hygienists.1 The review found that carpal tunnel syndrome was the most common MSD experienced by dental hygienists, with as many as 69.5% experiencing pain in the hand and wrist.1 Dental hygienists in the United States also suffer from low-back pain (56.8%), upper-back discomfort (67.4%), neck pain (68.5%), and discomfort in the lower extremities (less than 20%).1
MSDs have many possible etiologies, including poor posture; static posture, or staying in one position for a prolonged period of time; repetitive motions; mental stress; low fitness level; genetic inclination; and lack of rest.2 Multiple treatment options exist, though interventions intended to minimize or prevent musculoskeletal pain must be prescribed by a physician or specialist, and should be preceded by a thorough physical examination and assessment. Therapies that may be recommended for prevention and/or treatment of MSDs include chiropractic manipulation, acupuncture, massage therapy, and physical therapy.
CHIROPRACTIC CARE
Working in the same position for an extended time is likely to cause injury to the musculoskeletal system.2 The spine is composed of four natural curves that are interdependent of each other. If one curve flattens, the other curves are affected. When the spine is unbalanced (exaggerated or flattened), the bony structures of the vertebrae rest on top of each other, and the curves rely on muscles, ligaments, and soft tissue for support.3 When practicing dental hygiene, clinicians often avoid using the lumbar support of their stool, and flatten the lower back curve. This can lead to ischemia (lack of oxygen to the muscles), lower back pain, trigger points (tight muscles), and possible disk herniation (central portion of an intervertebral disk bulges out).3

FIGURE 2. This chiropractor uses manual therapy to adjust a patient’s neck.

FIGURE 2. This chiropractor uses manual therapy to adjust a patient’s neck.

FIGURE 3. Elbow pain is common among dental hygienists, and chiropractic treatment may help reduce it.
Chiropractors are primary health care professionals that practice a drug-free, hands-on approach to diagnosing and treating disorders of the musculoskeletal and nervous systems.4 Chiropractors address complaints of pain related to the back, neck, joints of the arms and legs, and headaches. The form of manual therapy used by chiropractors involves manipulating a joint, which is often accompanied by a cracking or popping sound.5 Patients are typically prescribed one or more adjustments per week, and each session addresses multiple areas of concern (Figure 1 through Figure 3). Besides manipulating or aligning the spine, some chiropractors also recommend rehabilitative exercises and provide diet and nutritional counseling.4 Spinal manipulation is generally safe with rare adverse events.5
Research on the effectiveness of chiropractic care is limited. Studies suggest chiropractic manipulation reduces pain and improves general health status.4,6,7 Additionally, patient satisfaction with chiropractic care is generally high.5,7 When compared to other forms of chronic pain treatment, however, a meta-analysis on the efficacy of chiropractic manipulation found no evidence that it was superior to other treatments, such as physical therapy, exercise, massage, or analgesics.8
ACUPUNCTURE
Based on the principles of traditional Chinese medicine, acupuncture has been practiced for more than 2,000 years. The philosophy of Chinese medicine asserts that the body is controlled by Qi, an energy that flows to major organs in the body through channels called meridians.9 More specifically, the theory of acupuncture is predicated on the belief that 12 main meridians correspond to the 12 major organs in the body. To maintain health, Qi must flow with precise strength and quality throughout the body.9 Each school of acupuncture therapy (eg, Western, traditional) employs its own methodology.
Acupuncture is the art of palpating the body to identify pressure points that cause either localized or referred pain or tenderness. The practitioner then inserts fine, sterile needles into acupuncture points located along the meridians. A treatment may involve the placement of a few or dozens of needles (Figure 4 and Figure 5).9 The needles may be stimulated manually or by the use of an electric current, remaining in place for up to 30 minutes. Patients frequently report feeling sedated or sleepy following acupuncture treatment. Some acupuncturists may offer other therapies, such as: moxibustion (burning herb above the skin surface); massage; cupping (placing cups on the skin to create suction); and exercise and diet recommendations.9 Typically, a patient receives six to 12 acupuncture treatments over a 3-month period, followed by a reevaluation every 2 months to 6 months.
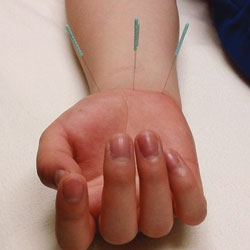
FIGURE 4. Acupuncture can be used to treat carpal tunnel syndrome.

FIGURE 5. Acupuncture needles are inserted into the pressure points that cause pain and tenderness. Special heat lamps, called Teding Diancibo Pu lamps, are used to reduce inflammation, improve circulation, and balance metabolism.
The World Health Organization and the US National Institutes of Health recognize the effectiveness of acupuncture therapy for the treatment of chronic pain, including pain in the back and neck.10,11 Studies on acupuncture treatment identify it as generally safe, if performed properly and by a well-trained practitioner, with minimal adverse reactions.9,10 Individuals with valvular heart defects and those with bleeding disorders or on anticoagulant therapy, however, should avoid acupuncture treatments.9
There is some evidence that acupuncture is more effective than placebo, with chronic pain relief in 55% to 85% of cases.10,11 A study investigating individuals with mild to moderate carpal tunnel syndrome found that acupuncture therapy was just as effective as prednisolone (a glucocorticoid used to treat inflammatory conditions).12 More longitudinal studies involving similar designs and treatment protocols are necessary to further support the effectiveness of acupuncture in relieving chronic musculoskeletal pain.
MASSAGE THERAPY
Keeping the arms and shoulders elevated for long periods of time impairs blood flow to muscles and tendons, and may lead to chronic pain and trigger points in the upper trapezius muscle.2 Trigger points, also known as knots, are caused by muscles that tighten and remain contracted for a prolonged period of time.3 Left untreated, flexibility in the localized area decreases, as does blood flow, while compression of nerves may lead to conditions, such as thoracic outlet syndrome and pronator syndrome.13 Thoracic outlet syndrome involves the compression of brachial nerve plexus and vessels between the neck and shoulder.14 It can cause numbness, tingling, and/or pain in the fingers, hand, or wrists.14 Pronator syndrome involves compression of the median nerve at the elbow. Symptoms are similar to carpal tunnel syndrome, and include numbness, pain, and tingling in the thumb, index, and middle finger.14

FIGURE 6. The application of firm pressure to a trigger point via massage therapy may relax the muscle.

FIGURE 7. For clinicians experiencing carpal tunnel syndrome, stretching of the wrist through massage therapy may provide some pain relief.
Therapeutic massage involves manipulating the soft tissue of the body to produce relaxation and relief of muscular aches and pains.15 Treatment is delivered in a quiet room with dimmed lights and soft music. Massage therapists may use a variety of techniques, including gentle stroking, pressure applied to a muscle, deep massage applied by circular motion, kneading of a muscle, and hacking or light karate chops.15
When treating patients with musculoskeletal disorders, therapists may incorporate physiotherapy, osteopathy, and chiropractic techniques. Sometimes massage therapy is combined with aromatherapy, which involves the use of diluted essential oils. Therapists trained in deep muscle therapy can ease trigger points through the application of firm pressure (Figure 6). The pressure may result, however, in pain that radiates to another area.3 Stretching can also be helpful in reducing pain (Figure 7). Dental hygienists can address trigger points by placing a tennis ball on a wall, then leaning against the ball and applying pressure toward the wall (Figure 8).3

A systematic review identified massage therapy as moderately superior to other therapies—such as joint mobilization, physical therapy, and acupuncture—in the treatment of MSDs. The review also concluded that massage therapy, in combination with exercise and self-care education, can be beneficial for chronic nonspecific low-back pain.16 Another study concluded that pain and disability were decreased after 10 sessions of massage therapy; however, the effects were limited at a 12-month followup.16 According to the literature, massage therapy is effective in the short-term management of musculoskeletal pain, as well as a preventive measure against MSDs. Receiving one massage per month may aid in maintaining overall health and reduce the likelihood of developing a MSD.
PHYSICAL THERAPY
Dental professionals can suffer from muscle imbalances due to repetitive bending in one direction.3 Physical therapists are health care professionals who work with patients to improve motion and manage pain effectively without the need for long-term use of medication.17 They examine, evaluate, and treat patients presenting with back pain, neck pain, carpal tunnel syndrome, headaches, injuries, MSDs, and numerous other health conditions.18 In addition, physical therapists also help individuals prevent injuries and promote a healthy lifestyle by suggesting methods to improve strength, flexibility, balance, and coordination.18
They can provide numerous rehabilitative, preventive, therapeutic, and educational services, including massage therapy, spinal manipulation, education about ergonomics, strength and flexibility training, stress management, and information on preventing problems from reoccurring.18 Physical therapists can test for muscle imbalances and also teach patients how to identify imbalances on their own. For example, to test for muscle imbalance in the neck, clinicians can bend the neck toward the right side and rotate the head toward the left. The opposite movement should be performed and then compared to the initial movement to determine which side has reduced range of motion. Right-handed clinicians usually have less range of motion when bending the neck to the left while rotating the head to the right side, and vice versa for left-handed clinicians.13
Static posture, even in the neutral sitting position, can lead to increased intramuscular pressure due to prolonged muscle contraction. Consequently, blood vessels within the muscle become compressed, leading to obstruction of blood flow. Pain and fatigue result as lactic acid builds in the muscle.13 To reduce the effects of muscle ischemia, trigger points, muscle imbalances, joint hypomobility (decrease in range of motion), disk degeneration, and nerve compression, dental hygienists may benefit from seeing a physical therapist who can prescribe specific recommendations, such as stretching exercises.3

FIGURE 9. Maintaining an incorrect sitting posture can cause low-back pain.

FIGURE 10. To strengthen the low back and prevent pain, dental hygienists should maintain a proper sitting posture at all times.
Stretching can significantly benefit the body by increasing blood flow to muscle groups, increasing joint synovial fluid, promoting joint range of motion, minimizing trigger points, providing nutrients to the vertebral disks, and relaxing the central nervous system.3 Imbalance between the abdomen and low back, as a result of constantly leaning toward a patient while seated, is usually the primary cause of low-back pain in dental professionals.13
To improve the lower back curve, dental hygienists should regularly activate the transversus abdominis muscles.13 The following exercise can be performed throughout the day:
- Sit tall, allowing a slight curve in the low back
- Pull the navel in toward the spine (as if preparing to take a hit in the stomach) while maintaining the low curve
- Hold the contraction for 1 minute while breathing normally
- Repeat five times
Contracting the lower abdomen toward the spine supports its natural curvature. When performed throughout the day, this exercise can help stabilize the transversus abdominis muscles and decrease low-back pain.2,13 Figure 9 through Figure 12 illustrate activation of transversus abdominis muscles, and lack thereof, while sitting and standing.

FIGURE 11. Poor standing posture can weaken the low back curve, causing musculoskeletal problems.

FIGURE 12. Proper standing posture engages the transversus abdominis muscles, helping to prevent low back injury.
CONCLUSION
Dental hygienists educate patients with periodontitis about the risk of complete tooth loss if the disease is left untreated. This concept is similar to MSDs. If musculoskeletal pain and discomfort are ignored, the damage to the musculoskeletal system may lead to serious injury or career-ending disability.2 When pain is experienced, dental hygienists should seek a comprehensive assessment and diagnoses by a physician or specialist before beginning any therapy. A multidisciplinary approach may be most beneficial. While some of these complementary approaches to addressing pain and injury do not have irrefutable bodies of evidence to support their efficacy, anecdotal experience should also be considered. Dental hygienists may benefit greatly from the treatment provided by chiropractors, massage therapists, acupuncturists, or physical therapists.
- Hayes M, Cockrell D, Smith DR. A systematicreview of musculoskeletal disorders amongdental professionals. Int J Dent Hyg.2009;7:159–165.
- Valachi B, Valachi K. Mechanisms leading tomusculoskeletal disorders in dentistry. J Am DentAssoc. 2003;134:1344–1350.
- Valachi B, Valachi K. Preventingmusculoskeletal disorders in clinical dentistry:strategies to address the mechanisms leading tomusculoskeletal disorders. J Am Dent Assoc.2003;134:1604–1612.
- American Chiropractic Association. AboutChiropractic. Available at: www.acatoday.org/level1_css.cfm?T1ID=42. Accessed October18, 2013.
- UpToDate. Spinal manipulation in thetreatment of musculoskeletal pain. Available at:www.uptodate.com/contents/spinalmanipulation-in-the-treatment-ofmusculoskeletalpain?detectedLanguage=en&source=search_result&search=Spinal+Manipulation+in+the+treatment+of+musculoskeletal+pain&selectedTitle=1~150&provider=noProvider. Accessed October 18, 2013.
- Chou R, Huffman LH. Nonpharmacologictherapies for acute and chronic low back pain: areview of the evidence for an American PainSociety/American College of Physicians clinicalpractice guideline. Ann Intern Med. 2007;147:492–504.
- Garner MJ, Aker P, Balon J, et al. Chiropracticcare of musculoskeletal disorders in a uniquepopulation within Canadian community healthcenters. J Manipulative Physiol Ther.2007;30:165–170.
- Assendelft WJ, Morton SC, Yu El, Suttorp MJ,Shekelle PG. Spinal manipulative therapy for lowback pain. A meta-analysis of effectiveness relativeto other therapies. Ann Intern Med.2003;138:871–881.
- Vickers A, Zollman C. ABC of complementarymedicine. Acupuncture. BMJ. 1999;319:973–976.
- National Center for Complementary andAlternative Medicine. Acupuncture May Be Helpfulfor Chronic Pain: a Meta-Analysis. Available at:nccam.nih.gov/research/results/spotlight/091012.Accessed October 18, 2013.
- World Health Organization. Acupuncture:Review and Analysis of Reports on ControlledClinical Trials. Available at: http://apps.who.int/medicinedocs/en/d/Js4926e/5.html. AccessedOctober 18, 2013.
- Yang CP, Hsieh CL, Wang NH, et al.Acupuncture in patients with carpal tunnelsyndrome: A randomized controlled trial. Clin JPain. 2009;25:327–333.
- Valachi B. Practice Dentistry Pain-Free:Evidence-Based Strategies to Prevent Pain andExtend Your Career.Portland, Ore: Posturedontics Press; 2008.
- Nield-Gehrig JS. Fundamentals ofPeriodontal Instrumentation and AdvancedRoot Instrumentation. 7th ed. Philadelphia:Lippincott Williams and Wilkins; 2012.
- Vickers A, Zollman C. ABC of complementarymedicine. Massage therapies. BMJ. 1999;319:1254–1257.
- UpToDate. Subacute and chronic low backpain: Pharmacologic and noninterventionaltreatment. Available at: www.uptodate.com/contents/subacute-and-chronic-low-backpain-pharmacologic-and-noninterventionaltreatment. Accessed October 18, 2013.
- American Physical Therapy Association.Benefits of a physical therapist. Available at:www.moveforwardpt.com/forhealthcareprofessionals/ detail.aspx?cid=84dd875a-7789-4c82-b466-d858b966b128. Accessed October 18, 2013.
- SpineUniverse: Vertical Health. What canphysical therapy do for me? Available at:www.spineuniverse.com/treatments/physicaltherapy/what-can-physical-therapy-do-me-0.Accessed October 18, 2013.
From Dimensions of Dental Hygiene. November 2013;11(11):67–71.



