Medication Use and Xerostomia
By keeping up to date on the most commonly used medications that cause dry mouth, dental hygienists can help patients maintain their oral health.
Today, many people manage their ailmentsvia prescription and over–the–counter (OTC) medications, and oftentimes these medications cause oral manifestations including xerostomia, gingival inflammation, oral candidiasis, ulcerations, and mucositis. Xerostomia is the most common oral side effect caused by medication use.1 The subjective feeling of dry mouth related to a reduction in salivary production and/or alteration of saliva’s chemical composition, xerostomia symptoms include burning mouth, thirst, altered speech, dry lips, and ulcerated mucosa.2,3
Saliva is essential for the comfort and function of the oral cavity as it lubricates and protects hard and soft tissues and aids in chewing, swallowing, and digestion. It also decreases infection risk and prevents dental caries.4,5 Saliva is produced by three major glands: the parotid, submandibular, and sublingual (Figure 1).4 Salivary gland dysfunction is often associated with hyposalivation, an unstimulated salivary flow (USF) below 0.1 ml/min and a stimulated salivary flow (SSF) below 0.5 ml/min, that results in a 40% to 50% reduction of typical salivary gland secretion.3 This leads to the formation of a thin layer of residual saliva on the hard palate, which triggers the sensation of dry mouth.3

MEDICATIONS THAT CAUSE XEROSTOMIA
According to the United States Surgeon General’s Report on Oral Health in America, dry mouth is a side effect of more than 400 prescription and OTC medications.4 The Academy of General Dentistry reports that xerostomia affects approximately one in four Americans, which means that about 25% of the US population is at an increased risk of oral complications due to dry mouth. Older adults are at the greatest risk of xerostomia because of their increased use of medications. As such, dental hygienists need to be familiar with the most frequently prescribed medications that cause xerostomia. The most common groups of medications that cause oral dryness are: cholesterol-lowering drugs; antihypertensives; antihistamines; antidepressants; antianxiety drugs; analgesics; drugs used to treat respiratory, gastrointestinal, and hormonal conditions; and chemotherapeutics.6,7 Table 1 provides a list of commonly used medications that cause xerostomia.
More than 97 million Americans have high cholesterol.8 Commonly known as statins, HMG-CoA reductase inhibitors are used to lower cholesterol levels. Zocor and Lipitor are two commonly prescribed statins. Side effects include increased enzymes, myopathy (muscle weakness), and xerostomia. Hypertension affects approximately 50 million Americans—causing 40,000 deaths per year and contributing to another 200,000. Diuretics were the first drugs used to treat hypertension in the 1950s.8
Today, angiotensin-converting enzyme (ACE) inhibitors are commonly prescribed to treat hypertension. Xerostomia is a frequent side effect of both ACE inhibitors and diuretics.8 Antihistamines are a group of drugs used to treat allergies.9 Diphenhydramine is a sedating antihistamine with anticholinergic effects that increases the risk of xerostomia. Loratadine, on the other hand, is a nonsedating antihistamine that creates less of an anticholinergic effect, which decreases the risk of xerostomia.9
Analgesics provide varying levels of pain management depending on their strength.9 There are two types of analgesics: nonnarcotic and narcotic. Salicylates, acetaminophen, and nonsteroidal anti-inflammatory drugs are examples of nonnarcotic analgesics.10 An opioid analgesic (eg, hydrocodone) is a natural or synthetic morphine-like substance used for reducing moderate to severe pain.9
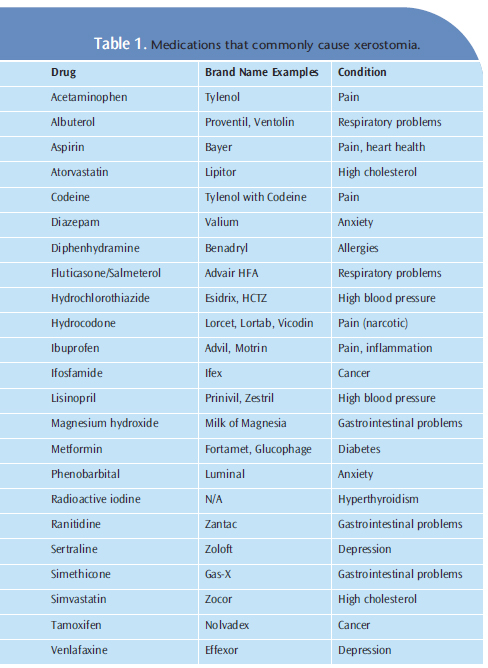
Depression affects approximately 5% to 10% of the population.10 There are three major drug groups used to treat depression: monamine oxidase inhibitors, tricyclic antidepressants, and selective serotonin reuptake inhibitors.10 Anxiety disorders are the most common type of psychiatric illness in the US, but less than 30% of people seek treatment. 8 There are several medications used to treat anxiety disorders; and prescription drugs, such as benzodiazepines and barbiturates, are recommended based on the severity of the condition.9
Respiratory diseases commonly treated with medication include asthma, chronic obstructive pulmonary disease, and upper respiratory tract infections.9 Respiratory drugs come from a wide range of medication types ranging from adrenergic drugs for bronchodilation to corticosteroids.9 Gastrointestinal drugs are available OTC or are prescribed based on the severity of the condition. Gastroesophageal reflux disease or heartburn is the most prevalent gastrointestinal disease in the US.9 Several groups of drugs are used to treat hormonal conditions such as diabetes, thyroid disorders, adrenal gland dysfunction, and contraceptives, including insulin (oral and injectable), antithyroids, estrogens, and steroids.10
Used in conjunction with surgery and radiation therapy, chemotherapeutic drugs treat various types of cancers or abnormally growing cells. These include alkylating agents, antimetabolites, hormones, antitumor antibiotics, immunomodulators, and plant extracts. These drugs exert varying types of oral side effects, but all can cause xerostomia. Dental hygienists should educate their patients about xerostomia management by actively engaging them during the comprehensive examination and oral hygiene instruction.
RECOMMENDATIONS FOR DENTAL HYGIENISTS
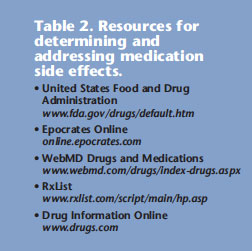
The clinical signs and symptoms of xerostomia are subjective and depend on patient perception.5 However, early detection and prompt intervention decrease the effects of xerostomia and improve quality of life. Oral health professionals should encourage patients to investigate the possible side effects of medications by providing easy–to–use resources. Websites are available that discuss the side effects created by various medications and offer strategies to mitigate them (Table 2).
In addition, prescription medications always include an information sheet that lists any possible side effects. The American Dental Hygienists’ Association offers a “Hyposalivation with Xerostomia” screening tool for oral health professionals to use as a guide when identifying a patient’s xerostomia risk level (here).11 The tool is designed for use during the assessment process and is composed of three major categories: source, symptoms, and signs. From the interview questions, clinicians can establish whether a patient’s risk of xerostomia is low, moderate, or high.11
ALLEVIATE SYMPTOMS
Patients diagnosed with xerostomia are at increased risk of dental caries, fungal infections, periodontal diseases, and other oral problems. 6,8 The US Food and Drug Administration has approved several prescription drugs to relieve dry mouth caused by medical treatments or conditions. For example, pilocarpine HCL (Salagen) and cevimeline (Evoxac) are cholinergic drugs that increase salivary secretions.8 Saliva substitutes may help patients manage their symptoms and they come in a variety of formats, such as mouthrinses, sprays, swabs, gels, and tablets that dissolve in the mouth.4 To improve salivary flow, patients should drink plenty of water or sugarless/neutral acid drinks, chew sugar–free chewing gum containing xylitol, and use a fluoride mouthrinse.4 Patients should also avoid alcohol–containing products, caffeine, and all forms of tobacco.4,6
CONCLUSION
Xerostomia is a condition experienced by many patients, and treating it requires a collaborative approach. Xerostomia can occur at any age, but patients who take multiple medications are at increased risk, which means it disproportionately affects older adults. As the American population ages, dental professionals will see more patients with xerostomia. Practitioners need to stay current on common xerostomia–inducing medications, ask descriptive questions, use screening tools during assessments, and provide patients with eas–to–access resources to help mitigate the consequences of this condition.
REFERENCES
- Kalmar J, James WD. Oral manifestations of drug reactions. Xerostomia.Medscape Reference. Available at: www.emedicine.medscape.com/article/1080772–overview. Accessed October 19, 2012.
- Leal SC, Bittar J, Portugal A, Falcão DP, Faber J, Zanotta P. Medication inelderly people: its influence on salivary pattern, signs and symptoms of drymouth. Gerodontology. 2010;27:129—133.
- Gueiros LA, Soares MS, Leão JC. Impact of aging and drug consumption onoral health. Gerodontology. 2009;26:297—301.
- United States Department of Health and Human Services. Dry mouth? Don’tdelay treatment. Available at: www.fda.gov/forconsumers/consumerupdates/ucm254273.htm. Accessed October 19, 2012.
- Cho MA, Ko JY, Kim YK, Kho HS. Salivary flow rate and clinical characteristicsof patients with xerostomia according to its aetiology. J Oral Rehabil.2010;37:185—193.
- Guggenheimer J, Moore PA. Xerostomia: etiology, recognition andtreatment. J Am Dent Assoc. 2003;134:61—69.
- Medications that cause dry mouth. NeuroTalk. Available at: www.neurotalk.psychcentral.com/showthread.php?t=25830. Accessed October 19, 2012.
- Weinburg MA, Theile CM, Fine JB. In: Cohen M, ed. Oral Pharmacology forthe Dental Hygienist.2nd ed. Upper Saddle River, NJ: Pearson Education Inc;2012.
- Haveles BE. Applied Pharmacology for the Dental Hygienist. 6th ed. MarylandHeights, Mich: Mosby Elsevier; 2011.
- Weinburg MA, Westphal C, Fine JB. In: Cohen M, ed. Oral Pharmacology forthe Dental Hygienist.Upper Saddle River, NJ: Pearson Education Inc; 2008.
- Fehrenbach MJ. American Dental Hygienists’ Association hyposalivationwith xerostomia screening tool. Access. 2010;24:22—25.
From Dimensions of Dental Hygiene. November 2012; 10(11): 34, 36, 38.

