Habits for Healthy Practice
Positioning, grasp, fulcrums, and instrument design are integral to improving the ergonomics of instrumentation.
Dental hygiene practice is physically demanding. During instrumentation, dental hygienists use heavy muscle and pinch forces, employ repetitive motion, and hold their wrists and forearms in awkward positions for prolonged periods.1 To reduce the risk of these musculoskeletal challenges, appropriate instrument selection and correct use of fulcrums and grasp are crucial.
NEUTRAL POSITION
The correct positioning of both the patient and practitioner is critical to the clinician’s long–term comfort and effectiveness.2 Maintaining a neutral position can improve safety and efficacy of performance, provide endurance, and reduce the potential for overexertion or injury.3 A neutral wrist position is key to reducing the risk of injury.3 To achieve a neutral position, the clinician needs to maintain a straight back with thighs placed slightly downward and body weight evenly distributed, feet flat on the floor, shoulders relaxed, wrist and forearm in a straight line, and eyes directed downward to prevent neck and eye strain.2,3 Dental loupes are also helpful in achieving a neutral position.
GRASP
The dynamics of grasp are important because they affect tactile sensitivity and control of the instrument, decrease the patient’s risk of trauma, and prevent fatigue in a clinician’s fingers, hand, and arm.3
The most commonly used instrument grasp is the modified pen grasp—an efficient, stable grasp that works with most dental instruments and is a slight variation of the conventional or standard pen grasp.4 The modified pen grasp is a three–finger grasp using the thumb, index finger, and middle (second) finger, keeping all three fingers in contact with the instrument.
The three fingers create a tripod placing the pad of the thumb, pad of the first finger, and side of the second finger pad on the handle of the instrument (Figure 1). The instrument rests between the second and third joints of the first finger or in the crook of the hand, depending on the area being instrumented. The effectiveness and efficiency of the modified pen grasp is influenced by the positioning of the wrist, forearm, elbow, and shoulder. Neutral positioning of these specific body parts is essential to preventing cumulative trauma disorders, including carpal tunnel syndrome.3,5 To obtain neutral positioning, the wrist is straight and the forearm and hand are in the same horizontal plane, and the elbow is 90° or greater with the shoulders level and relaxed.3 Neutral wrist positioning may reduce grasp pressure, thus, decreasing the risk of musculoskeletal disorders.
FULCRUM / FINGER REST

One of the simplest ways to prevent injury is to use a fulcrum during instrumentation. A fulcrum is a finger rest implemented to stabilize the hand while performing clinical procedures and to reduce muscle stress.6 Fulcrums also improve precision of instrumentation and help prevent slippage and sudden movements that could cause trauma to the patient.7 Little research has been conducted on the use of fulcrums and pinch forces during dental hygiene instrumentation. In 2005, Dong et al7 compared the effects of three different positions—no finger rest, one finger rest, and two ringer rests—on muscle load and pinch force during simulated dental hygiene tasks. The results showed that the use of a two–finger rest always reduced thumb pinch force and muscle activity and that the one–finger rest reduced thumb pinch force and muscle activity most of the time. The authors concluded that the use of finger rests is important in decreasing the muscle load in the hands of clinicians and that providing dental and dental hygiene students with instruction on fulcruming early in their training may provide long–term musculoskeletal benefits.7
A 2008 study by Cosaboom–FitzSimons et al looked at five different finger rest positions, including opposite arch, standard intraoral, basic extraoral, cross arch, and finger–on–finger fulcrums. Results showed that regardless of the fulcrum used, similar amounts of muscle activity were produced.1 Dental hygienists should continue to use alternative fulcrums based on need, preference, and improved ergonomics.1
INSTRUMENT DESIGN
Handle design and finger force affect the risk of upper extremity musculoskeletal disorders. Dental instrument handle surfaces can change the pinch force required in dental tasks. One study looked at whether the static friction between an instrument and a wet gloved finger was influenced by the material used to manufacture the instrument, the instrument’s surface texture, or the glove material.8 The study found that static friction was important in reducing slippage of instruments under wet or contaminated conditions.8 Additionally, surface texture, such as cross–hatching and dimpling of dental instrument handles, can affect pinch forces during instrumentation activation. The texture can be scored, smooth, or a combination of both. Surface texture can enhance grip, increase control, and reduce hand fatigue.
Regarding shape, most dental hygiene instruments are either round or octagonal. A thin handle may be difficult to grasp, thus increasing the risk of muscle cramping. Lightweight (hollow) handles with larger diameters and balanced ends are recommended to increase tactile sensitivity and decrease clinician fatigue. Most companies offer instruments with a choice of varying diameters of handle thickness and surface texture.
Instrument sharpness is another consideration for dental instrument selection. Dull instruments require added force for effective calculus removal.9 Several companies now offer instruments made with new metals that require less frequent sharpening. An instrument with a sharp blade will be less fatiguing to the clinician and contribute to the efficacy of deposit removal.
VIBRATION
Slow–speed handpieces and ultrasonic scalers can enhance the effectiveness of instrumentation, but they can also be heavy with long and awkward cords, and their vibration may create negative ergonomic consequences. Prolonged exposure to slow motor handpiece vibrations and cord torque may contribute to work–related musculoskeletal disorders.9 When choosing a handpiece, a lightweight, comfortable ergonomic design with adequate balance and a larger diameter to reduce pinch force and allow ease of movement is optimal.10 Cord–free handpieces eliminate cord torque. The repetitive vibration caused by ultrasonic scalers is a consideration for dental hygienists. Long–term exposure to high–frequency vibrations may increase the risk of nerve damage, but this is still being investigated. Using the blended approach of combing hand and ultrasonic instrumentation may reduce this risk as well as help modify the pinch forces dental hygienists use throughout the day.
CONCLUSION
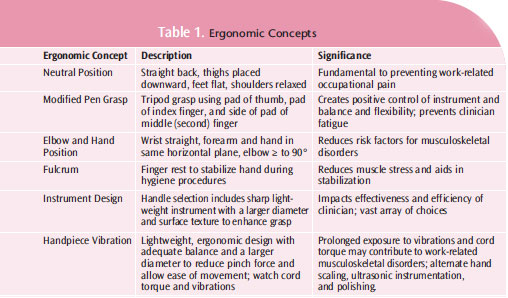
Correct grasp, appropriate use of fulcrums, and careful selection of instruments based on ergonomic design are important to the safe practice of dental hygiene. Table 1 provides an overview of key ergonomic concepts related to instrumentation. By improving the ergonomics of daily dental hygiene practice, clinicians can reduce their risk of musculoskeletal injury and enjoy a long and pain–free career in the field.
REFERENCES
- Cosaboom–FitzSimons ME, Tolle SL, Darby ML, Walker ML. Effects of 5 different finger rest positions on arm muscle activity during scaling by dental hygiene students. J Dent Hyg. 2008;82:34.
- Fehrenbach MJ, Weiner J. Saunders Review of Dental Hygiene. 2nd ed. St. Louis: Elsevier; 2009:398–399.
- Matsuda SA. Instruments and principles for instrumentation. In: Wilkins EM, ed. Clinical Practice of the Dental Hygienist. 10th ed. Baltimore: Lippincott, Williams, & Wilkins; 2009:619–622.
- Pattison AM, Pattison GL. Periodontal Instrumentation. 2nd ed. Upper Saddle River, NJ: Prentice Hall; 1991.
- Hodges KO. Concepts in Nonsurgical Periodontal Therapy. Albany, NY: Delmar Publisher; 1998:298.
- Franzblau A, Armstrong TJ, Werner RA, Ulin SS. A cross–sectional assessment of the ACGHI TLV for hand activity. J Occup Rehabil. 2005;15:57–67.
- Dong H, Barr A, Loomer P, Rempel D. The effects of finger rest positions on hand muscle load and pinch force in simulated dental hygiene work. J Dent Educ. 2005;69:453–460.
- Laroche C, Barr A, Dong H, Rempel D. Effect of dental tool surface texture and material on static friction with a wet gloved fingertip. J Biomech. 2007;40:697–701.
- Michalak–Turcotte C. Controlling dental hygiene work–related musculoskeletal disorders: the ergonomic process. J Dent Hyg. 2000;74:41–48.
- Smeltzer D. Branan S. Ergonomic considerations for low–speed handpieces. J Pract Hyg. 2007;16:15–16.
From Dimensions of Dental Hygiene. November 2012; 10(11): 42, 44.

