
Maximizing Protection
Personal protective equipment is a key component of effective infection control in the dental operatory.
Proper infection control is a crucial aspect of every dental hygiene practice setting. Without it the safety of the work environment is compromised, which results in a setting where a wide array of diseases may be transmitted to patients and practitioners. An important component of infection control protocol is the use of personal protective equipment (PPE), which includes any type of face mask, glove, or clothing that serves as a barrier between infectious materials and the skin, mouth, nose, or eyes (mucous membranes).
Surgical face masks and protective eyewear are integral components of PPE and help contribute to a safer work environment. Face mask fit along with filtration and protective eyewear protocols are important in reducing contamination of the mucous membranes and skin surrounding the eyes, nose, and mouth as well as injury and infections. Their proper use may be overlooked in the hectic day-to-day activities of practice—compromising the safety and health of both practitioners and patients.
Dental hygiene procedures involving air-water syringes, ultrasonic scaling devices, and polishing procedures generate aerosols, which produce potentially hazardous droplets and splatter that are contaminated with bacteria and blood.1 Mycobacterium tuberculosis, staphylococci, streptococci, herpes simplex virus, cytomegalovirus, and hepatitis B and C are examples of pathogenic microorganisms transmitted in the dental practice setting through the inhalation of airborne microbes and contact with the mucous membranes via droplets and splatter.1-3
FACE MASKS
Donning of face masks has long been advocated to protect oral care clinicians’ mucous membranes of the nose and mouth from exposure to aerosol and splatter generated during patient care. However, dental hygienists desiring the best protection from these hazards must choose a mask that fits properly, is fluid resistant, and effective in filtering debris and splatter. Also important is correct usage during and after patient care. Face masks vary widely in style, types, and sizes and selection should be based on fit and intended application.4 The “one size fits all” mask approach where all procedures are completed with the same type of mask by all office staff should be revisited. Mask selection based on both proper fit and given application or exposure risk of the activity is a more contemporary approach.
Composed of several layers of synthetic material, face masks are designed to filter and collect microscopic particles that come directly in contact with the mask.5 Recommended face masks for dentistry should have a bacterial filtration of 95% for a particle range of 3 µm to 5 µm in diameter.1 Bacterial filtration efficacy (BFE)—the effectiveness of medical face mask material to prevent passage of aerosolized bacteria—is expressed in the percentage of a known quantity that does not pass the medical face mask material at a given aerosol flow rate.6 A particle size of 1 µm to 6 µm provides acceptable BFE. Most of the particles created by dental procedures are large droplets and splatter and are not carried into the lungs.6,7 These particles can still enter the mucous membranes of the eyes, nose, or mouth and are capable of pathogen transmission.
BARRIER PROTECTION
  |
Low, moderate, or high barrier protection categories, as determined by the American Society for Testing Materials (ASTM) guidelines, aid in determining the best mask type for the procedure to be performed.8 In addition to BFE, particulate filtration efficiency (PFE) is also used to test the efficacy of a mask by evaluating its ability to filter particles spore size of 0.1 µm to 1.0 µm. Based on these ASTM guidelines, manufacturers divide masks into levels of protection. Dental hygienists need to understand that the greater the protection, the harder the mask is to breath through. A low level mask category, although meeting OSHA standards for all dental hygiene procedures, is optimal for oral examinations, hand instrumentation, fluoride treatments, and basic laboratory work, all of which are procedures that involve no spray or aerosols. The moderate performance mask provides PFE= 98.5% at 0.5 µm and provides excellent protection during dental procedures such as a dental prophylaxis, which involves a lower level of aerosol production. Maximum protection from higher aerosol-producing procedures, such as ultrasonic scaling for long periods of time, oral examinations for higher risk patients, air polishing, and air-water syringes, are best met with a high barrier protection mask that provides a PFE= 99.8% at 0.1 µm as compared to the PFE= 98% at 0.1 µm of a low level mask. The manufacturer’s labeling of these types of barrier protection assist dental hygienists in making informed decisions about mask selection. Anticipated aerosol production should be used as the criterion for mask selection as it is impossible to measure the exact amount of aerosol each dental hygiene procedure will produce. However, the choice should be a mask that covers the nose, mouth, facial hair, and fits snugly against the sides of the head with no gaps.
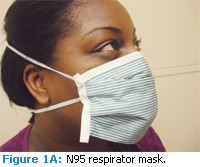
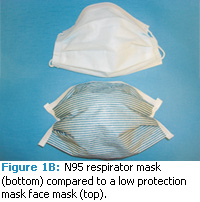
A concern of all health care professionals is the transmission of H1N1 (novel Influenza A). Dental face masks are not designed to filter very small particle aerosols containing viruses and hence do not provide protection against the H1N1 virus.9 High filtering face respirators designed to filter particles out of the air and protect the wearer from small particle aerosols containing viruses are the face protection of choice. The National Institute for Occupational Safety and Health (NIOSH) certifies three classes of filtration for masks: N-, R-, and P- series and three levels of filtration efficacy: 95%, 99%, and 99.97% in each class.10 Anything above N95 is considered a respirator type of device and can provide protection against viruses if the device is custom fit and used correctly (Figures 1A and 1B). When working with patients who have suspected or known cases of H1N1 influenza, the N95 fittested respirator should be donned prior to entering the treatment room as well as during all dental procedures.11
A NIOSH-certified particulate-filter respirator is also necessary with airborne infection isolation precautions that are required when treating patients who have highly communicable diseases such as tuberculosis. According to NIOSH, infectious droplet nuclei measure 1 µm to 5 µm, therefore the surgical mask worn should effectively filter the smallest particles in this range (1 µm).10 N95 refers to the filterability and, in the unloaded state, provides protection of 1 µm particles and a filter leakage of <5%, meeting the OSHA requirements of >95% filtration. The level of protection provided by a respirator is determined by the fit or seal of the face piece (face-seal leakage) and the filtration material effectiveness of incoming air. Although the surgical N95 respirator fulfills the OSHA filtration requirements and is NIOSHcertified, the majority of surgical masks do not and should not be used as airborne infection isolation precautions.10 Patients who have serious airborne diseases should be treated in a special facility where the proper precautions are taken. Therefore, respirators are not the standard for PPE in most dental offices. However, with the threat of new emerging diseases, such as H1N1, the demand for high particulate respirators masks may increase.
APPROPRIATE USAGE AND PROPER FIT

Worn correctly, masks should be donned prior to eyewear, they should cover the mouth, and secure firmly against the bridge of the nose and under the eyes to reduce fogging of eyewear. A proper fitting mask should create a seal for the nose and mouth and cover any facial hair but should not come in contact with with the lip or nostrils.5 Allowing a mask to slip below the nostrils is a common practice of some clinicians who complain about breathability problems or poor fit. This improper practice greatly compromises the afforded barrier protection allowing airborne contaminants to be inhaled.
A snug fit along the entire periphery of the mask is necessary because without a good seal, leaks occur on the sides of the mask. Unfiltered exhaled and inhaled air can pass through these openings.12 Mask contamination results from exposure to aerosols as well from handling the mask through the course of treatment. Masks can become damp from exhaled air or by touch from contaminated gloves as well as splashing and splattering of body fluids that contain microorganisms. Changing the mask every 20 minutes in a wet environment and every 60 minutes in a nonaerosol environment and between patients is recommended.7
The practice of changing masks with each patient may be better understood and more widely practiced than changing masks when they become wet.12 A wet mask does not filter efficiently and undermines the barrier protection for which it was intended. When masks become wet from both the clinician’s breathing and external aerosols and splatter, a wicking effect occurs. Wicking (moisture being drawn into the material) allows external contaminants to penetrate the mask and potentially come in contact with the clinician’s tissues.12,13
Often a mask is removed when the patient is dismissed and not replaced during clean up. This infection control error results in direct exposure of the clinician to airborne microorganisms. Aerosol contaminants linger in the treatment room long after the treatment is completed and can be directly inhaled into terminal lung alveoli.13
PROTECTIVE EYEWEAR
Masks provide the dental hygienist with partial protection from aerosols and injury. Proper eyewear is equally important and should be worn in conjunction with face masks. Knowledge and implementation of eye safety practices are critical to prevent injury to ocular tissues of both dental hygienists and patients. The Centers for Disease Control and Prevention (CDC) considers use of protective eyewear a key strategy for preventing occupationally acquired eye infections as well as work-related ocular injuries.1 While OSHA requires the provision of safety glasses by the employer, the responsibility to use this protection vigilantly and safely is up to each practitioner.14,15 For some, the risks of eye injury seem remote after years of accident-free treatment and this important safety procedure may not be taken seriously. Unfortunately after an accident or injury occurs, it is too late.
Bezen has identified four categories of common ocular injuries in the oral care environment: mechanical, microbial infection, chemical, and lasers/electromagnetic radiation.16 Use of appropriate safety eyewear minimizes risk from these types of injuries. Mechanical injuries often occur during instrumentation procedures as contaminated debris, calculus, biofilm, infected tooth material, and saliva are propelled toward the clinician. Often containing large concentrations of bacteria, ocular contact with these toxic substances increases risk for ocular infection. Viral and bacterial conjunctivitis, Staphylococcus aureus, hepatitis B, and ocular herpes (the second leading cause of blindness) are infection risks associated with aerosol-producing instruments used by dental hygienists.16,17 Ocular herpes is a risk even without signs of intraoral or extraoral herpetic lesions because the virus is often present in the saliva before clinical symptoms.
Good eye safety practices are mandated in the laboratory as well as in the direct treatment area. Mechanical injuries may occur during laboratory procedures when dental hygienists are performing model pouring, trimming, and grinding as flying debris and aerosols are produced. Additionally, a wide array of chemicals used in practice settings may present a hazard to ocular tissues. Accidental exposures via splashed chemicals or from glove transfer to the eye from disinfectants, cleaning agents, radiographic processing solutions, and various dental materials may cause serious ocular burns and injury to unprotected eye tissues.7
PATIENT PROTECTION
Equally important is patient eye protection, which is a vital safeguard against injury, infection, and potential lawsuits. With patients’ eyes less than 5 cm from the work area, left unprotected, the possibility of injury and infection is high. During treatment, instruments are frequently used and passed in very close proximity to the eyes, flipped from end to end, and picked up and released on the bracket table. A small slip, instrument drop, or a broken anesthetic cartridge can result in serious physical and or chemical injury to the patient’s unprotected ocular tissues. Moreover many agents used during a prophylaxis are not compatible with ocular tissue, such as fluoride, bentonite (ingredient in some polishing agents), and chemicals found in disinfectants. Patient eye infections are caused by contamination from particles containing saliva, plaque, and bacteria-laden calculus from scaling and can be heavily contaminated with microorganisms from aerosol-producing instruments. Corneal abrasions, conjunctiva foreign bodies, subconjunctivitis hemorrhage, recurrent erosion, punctures, and conjunctivitis have been reported in dental patients.18,19 Industrial strength polycarbonate glasses with side shields are ideal because they provide more resistance to debris, splatter, and projectiles.16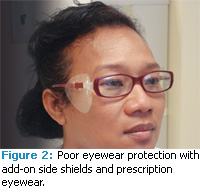
The CDC recommends that safety eyewear in the dental environment meet the American National Standard Institute Standards (ANSI) for impact resistance.1 Eyewear that meet these standards display symbols or markings either on the lens or arm of the protective eyewear. Markings include the manufacturer’s symbol and a symbol indicating it meets standard impact resistance (Z87. 1-1989) or the requirement for high-impact resistance Z87 (Z87.1plus 2003).20
THE CORRECT FIT
Three basic types of protective eyewear are available: glasses, goggles, and face shields. In addition to being impact resistant ideal characteristics of each type of eyewear include: light weight, scratch resistant, distortion free, and comfortable for the practitioner. Fit of the eyewear is of paramount importance. The closer the eyewear fits to the face, the better the quality of the seal provided and the less chance of an object penetrating the edge of the eyewear. A tighter seal also prevents chemical splashes, debris, and splatter from contacting ocular tissues.19
Protective eyewear must be large enough to adequately protect the front and sides of the clinician’s eyes from both macroscopic and microscopic injury.5 A common mistake made by oral health care practitioners who wear prescription eyeglasses is wearing them as safety eyewear. Contemporary prescription glasses often consist of small frames with small lens diameters. They are often not impact resistant, and provide minimal eye protection from flying debris and chemicals. Typically, prescription glasses should not be used as safety eyewear because they do not meet ANSI standards and are not large enough for adequate protection.
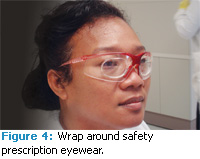
Wraparound glasses or glasses with solid side shields prevent microorganisms and debris from entering the sides of the eyewear. Disposable plastic add-on side shields are available for clinicians with prescription eyewear although many add-on shields do not adapt well to the sides of the face and minimize their effectiveness (Figure 2). If add-on side shields are used, they need to be solid and fit tightly against the sides of the glasses and the face. For prescription eyeglass wearers, ANSI-certified goggles or full face shields can be used over prescription eyewear. This combination, however, may prove cumbersome and uncomfortable for the clinician (Figure 3). Another option is to have the lens prescription placed into impact resistant safety glasses (Figure 4). During procedures where a large amount of splatter is produced, a clear face shield may be useful. In general, eyewear may be substituted with a clear face shield, however, a face shield does not substitute for a surgical mask.13
For maximum protection and comfort a combination of features is available among eyewear manufacturers that contribute to their wearability. In addition to solid impact resistant side shields, adjustable side arms, brow guards, anti-fog features, and mask hooks are available. Anti-fog features are available on masks as well as eyewear via anti-fog cloth wipes or anti-fog lenses. Mask hooks are available on certain protective eyewear and conveniently combine the mask and eyewear as a single unit by allowing the ear loops of the mask to hook on a clasp on the side of the protective eyewear and removal of PPE is performed with less risk of cross contamination. One disadvantage to this feature is the inability to prolong the use of the mask in high aerosolproducing procedures that may have airborne contaminants for several minutes after the dental hygiene procedure is complete.
CARE OF EYEWEAR
Soap and water are sufficient for decontaminating protective eyewear.1 Ideally the manufacturer of the eyewear should be consulted to determine appropriate cleaning and disinfecting agents. Alcohol-based sanitizers especially developed for eyewear are a good choice for disinfection. However, loupes require special care and the manufacturer’s directions should be closely followed. Since many chemical disinfectants can cause eyewear distortion over time as well as irritation to the eyes, they should be used with caution.
GLOVES
Gloves are the third component of PPEs and while they are not the focus of this article, they warrant a brief discussion. Protocols for gloves seem to be well understood with high adherence to standards. All gloves used during patient treatment should be Food and Drug Administration approved to ensure maximum protection. Gloves should be donned after the placement of eyewear and masks, and hands should be washed prior to and after gloving. After 1 hour of use gloves should be changed or sooner if a tacky, sticky surface develops. Gloves should never be washed with detergents for reuse because wicking may occur, compromising the afforded barrier protection. Ideally gloves should cover the cuffs of long sleeved clinic attire to ensure the covering of all skin.16
Changes in glove needs most often result from latex allergies affecting patients and clinicians. Nitrile gloves have improved over time in functionality and many dental hygienists will find these an excellent alternative to latex gloves. Also petroleum-based hand lotions and lip lubricants can also degrade latex, undermining their barrier protection.
During the provision of care appropriate usage is typically practiced because donning of gloves with each patient is routine. In the hectic aspects of day-to-day operations the biggest concern may be the lack of heavy duty utility gloves that should be worn during all clean up procedures as a safeguard from injury. Available in both sterile and nonsterile types, these puncture-resistant neoprene or polynitrile gloves should be donned when transporting contaminated instruments or when placing them in and out of ultrasonic cleaning devices to prevent injuries and during cleaning and disinfecting procedures.14
CONCLUSION
Dental face masks and eyewear are not created equal nor do all dental procedures involve equal risks of exposure. Dental professionals must make prudent decisions when selecting and donning PPE if they are to be effective in minimizing risks of exposure to infectious agents and accidents, which can threaten both their health and safety as well as their patients’.
REFERENCES
- Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003; 52:1-61.
- Harrel S, Molinari J. Aerosols and splatter in dentistry a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135:429-437.
- Bennett AM, Fulfors MR, Walker JT, et al. Microbial aerosols in general dental practice. Br Dent J. 2000: 189: 664-667.
- Oberg T, Brosseau LM. Surgical mask filter and fit performance. Am J Infect Control. 2008:36:276- 282.
- Molinari J, Harte J. Practical Infection Control in Dentistry. 3rd ed. Philadelphia: Wolters Kluwer/Lippincott, Williams, Wilkins; 2009.
- Miller C, Palenik C. Infection Control and Management of Hazardous Materials for the Dental Team. 3rd ed. St. Louis: Elsevier Mosby; 2005.
- Jorgenson, G, Palenik CJ. Selection and use of personal protective equipment. The Dental Assistant. 2004; 73:16-19.
- American Society for Testing and Materials. Stan dard specification for performance of materials used in medical face masks. Available at: www.astm.org/Standards/F2100.htm. Accessed February 2, 2010.
- Centers for Disease Control and Prevention. Interim Recommendation for facemask and respirator use to reduce novel influenza (H1N1) Virus transmission. Available at: www.cdc.gov/h1n1flu/masks.htm. Accessed February 2, 2010.
- TB Respiratory Protection Program in Health Care Facilities Administrators Guide. National Institute for Occupational Safety and Health. Available at: www.cdc.gov/niosh/99-143.html. Accessed Sept. 4, 2009.
- Centers for Disease Control and Prevention. Prevention of 2009 H1N1 Influenza Transmission in Dental Health Care Settings. Available at: www.cdc.gov/niosh/docs/99-143/. Accessed February 2, 2010.
- Organization for Safety & Asepsis Procedures. FAQs for personal protective equipment. Available at: www.osap.org/displaycommon.cfm?an=1&subarticlenbr=728. Accessed February 2, 2010.
- Runge P. Not all face masks are created equal—what is the best for you? The Dental Assistant. 2005; 74(4):4-8.
- Wilkins EM. Clinical Practice of the Dental Hygienist. 10th ed. Philidelphia: Lippincott Williams and Wilkins; 2009.
- Hill E. Eye Safety Practices in U.S. dental school restorative clinics. J Dent Educ. 2006;70:1294-1297.
- Bezan D, Bezan K. Prevention of eye injuries in the dental office. J Am Optom Assoc. 1988; 59: 929-934.
- Farrier SL, Farrier JN. Eye safety in operative dentistry—a study in general dental practice. Br Dent l. 2006; 200:218-223.
- Szymanska J. Work-related vision hazards in the dental office. Ann Agric Environ Med. 2000; 7:1-4.
- Khalid A, l Wazzan A, Almas K, et al. Prevalence of ocular injuries, conjunctivitis and use of eye protection among dental personnel in Riyadh, Saudi Arabia. Int Dent J. 2001;51:89-94.
- Occupational and Educational Personal Eye and Face Protective Devices. ANSI Z87.1-2003. New York: American National Standards Institute (ANSI); 2003.
From Dimensions of Dental Hygiene. March 2010; 8(3): 26, 28-31.


