
Innovation in Tooth Whitening
The continuous advances in whitening materials and techniques reflect the efforts of oral health professionals and industry toward preserving tooth structure, minimizing dentinal hypersensitivity, and enhancing esthetics.
The demand for whiter teeth has spurred the development of many innovations in professional oral health care technologies, as well as in over-the-counter (OTC) products. Discoloration can present in various ways, and, depending on the nature of the discoloration, the treatment approach and outcome can vary significantly. When discussing tooth whitening, it is important to acknowledge the work of many pioneers who enabled the profession to offer tooth whitening as a conservative, alternative treatment to whiten and lighten discolored teeth that otherwise would have to be treated with veneers or crowns—with concomitant removal of sound tooth structure. Historically, professional whitening procedures were performed in the dental office, typically using concentrated hydrogen peroxide (H2O2) and by isolating surrounding soft tissue to avoid contact with the whitening agent. Although this proved effective, drawbacks included lengthy chairtime, cost, and the risk of dentinal hypersensitivity. These downsides were addressed by Haywood and Heymann in 1989, with the introduction of nightguard vital bleaching using 10% carbamide peroxide in a custom tray worn at night.1This technique offered the possibility of whiter vital teeth at a reduced cost, and with fewer side effects. It also marked an evolutionary step in tooth whitening, as the patient took on the responsibility of performing the procedure at home.
Advances in whitening materials and delivery methods appeared as the oral health care industry realized it could address consumers directly by introducing OTC whitening products. Among these offerings, technology was introduced in 2000 that used hydrogen peroxide on a clear strip of tape that was applied to the teeth.2 Then, as now, a drawback of OTC tooth whitening products used without professional supervision is the potential lack of a proper diagnosis for the cause of tooth discoloration, which would allow clinicians to suggest appropriate therapy, and monitor the efficacy and safety of treatment.
In response to consumers’ desires for improved perception of tooth color, dental manufacturers often promote the whitening component in dentifrices. While ordinary whitening toothpastes relied mainly on their efficacy in removing extrinsic tooth stains, the newer generation or “advanced whitening” dentifrices also claim to be effective in removing intrinsic stains.3
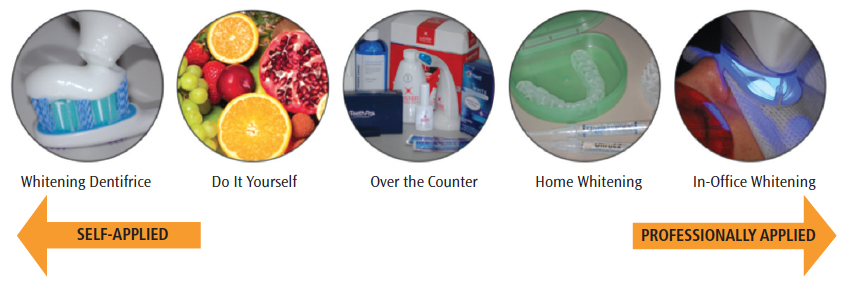
The diversity of whitening methods (Figure 1) has created confusion among patients in terms of expectations that can be realized with each treatment modality. The purpose of this article is to define extrinsic and intrinsic discoloration, help clinicians understand the active ingredients and chemistry behind each whitening technique, and strategies for addressing hypersensitivity. This will facilitate appropriate decision-making, based on the nature of tooth discoloration.
TOOTH COLOR AND TYPES OF DISCOLORATION
Tooth color is primarily determined by the reflectance of the dentin, modified by the absorption, scattering, and thickness of the enamel.4 Tooth color varies among individuals, among teeth in the same individual, and even within the same tooth.5 Furthermore, tooth color is not constant over a lifetime, and can change for various reasons.4
The etiology of tooth discoloration is broadly classified as extrinsic or intrinsic, depending on the origin of the stain. It has also been reported that long-standing extrinsic stains can become internalized, making removal more challenging.6 Extrinsic stains of various color—such as those caused by coffee, tea, red wine, tobacco, and colored food—are caused by superficial accumulation of residue on the enamel surface. These can be accentuated by pitting or irregularities of the enamel, salivary composition, salivary flow rates, and poor oral hygiene.7 Stains remain on the tooth surface due to attractive forces, including long-range interactions (such as electrostatic and van der Waals forces), and short-range interactions (such as hydration forces, hydrophobic interactions, dipole-dipole forces, and hydrogen bonds).8
Intrinsic discolorations are incorporated during tooth formation or after eruption, and are attributable to the presence of stain molecules within the enamel and dentin.9 Preeruptive stains arise due to dental fluorosis, tetracycline staining, hematologic disorders, and inherited developmental defects of enamel or dentin without systemic features.7 Post-eruptive intrinsic stains can result in local discoloration. The severity varies according to the etiology, and may range from mild yellow/orange to dark brown and black. These are commonly associated with caries, restorative materials, and pulpal hemorrhage.
Despite the fact that enamel is inert and does not have any remodeling capacity, it still undergoes continuous, dynamic ion exchange with the oral biofilm—with calcium phosphate apatite crystals moving in both directions to maintain proper mineral balance.10 In fact, enamel and dentin act as a semipermeable membrane that allows small molecules to pass into the tooth structure. This may account for reports of tooth discoloration from extrinsic sources becoming internalized. The key properties that cause enamel and dentin to bind to and retain staining molecules internally, however, are still not well understood.
TOOTH WHITENING CHEMISTRIES
Traditionally, stains of extrinsic origin were removed by toothbrushing or dental prophylaxis, which relies on abrasive action. Stains of intrinsic origin, by comparison, could be removed only by oral health professionals using oxidizing agents, such as hydrogen or carbamide peroxide. There has been a paradigm shift, however, with two major events taking place. The first is the incorporation of oxidizing agents into OTC whitening products, as well as dentifrices. The second development is emerging evidence that extrinsic stains can become internalized, which makes a strict distinction between extrinsic and intrinsic discoloration more difficult to establish. One might argue, therefore, whether every type of discoloration eventually can be treated with self-applied methods on a daily basis.
WHITENING DENTIFRICES
Whitening dentifrices basically contain the same functional ingredients of ordinary toothpaste formulations. These include:
- Solid cleansing abrasive materials that aid in physically removing the stains with the use of hydrated silica, calcium carbonate, dicalcium phosphate dihydrate, calcium pyrophosphate, alumina, perlite, and sodium bicarbonate11
- Humectants
- Thickening agents
- Surfactants
- Active agents, such as fluoride, to impart anticariogenic health benefits
- Flavoring
- Sweeteners
- Opacifying agents
- Coloring agents
- Buffering and preserving agents to maintain stability12
In addition to these basic ingredients, whitening dentifrices may contain peroxide, enzymes, citrate, pyrophosphates, and hexametaphosphates to augment the cleaning and/or prevention of stains.12 Although incorporating additional chemicals seems easily accomplished, it is not a simple process because potential interactions with new chemicals may adversely affect preexisting characteristics, such as stability, efficacy, and consistency.
Extensive research has been conducted in optimizing the stain removal potential of dentifrice abrasives, while minimizing any deleterious wear effects to the tooth surface.13 The relative safety of abrasives is established by standard methods referred to as relative dentin abrasivity.13 A study comparing dentifrices showed that, with few exceptions, dentifrices marketed as whitening products were generally more abrasive to dentin, especially those containing silicas.14 The stain-removal potential of dentifrices in clinical trials are usually evaluated with common indexes, including the Lobene Stain Index or Macpherson-modified Lobene Stain Index, which are related to the area and intensity of the stain.15,16
Another attribute of dentifrice is its polishing ability that can increase luster and improve esthetics, while also rendering the tooth surface less susceptible to further staining.14 Because toothbrushing is performed on a daily basis, further advances in technology would likely benefit public health. With continuous innovations, dentifrices may enable effective stain prevention and also include components that can penetrate deep into the enamel and dentin to interact with intrinsic stains.
DO-IT-YOURSELF (DIY) WHITENING
Do-it-yourself (DIY) whitening is promoted on myriad news outlets that provide information about at-home whitening remedies, including rubbing crushed strawberries, apples, or activated charcoal on teeth. The advocated use of these fruits is based on anecdotal perception, with the rationale being that they contain malic acid. The argument for using charcoal is based on its abrasiveness in removing stains.
The use of DIY whitening with strawberries has been investigated in vitro and compared with conventional whitening modalities, including the use of an OTC product, professionally dispensed, patient-applied home whitening, and professionally applied in-office whitening. At three months post-whitening, the DIY group showed an overall tooth color change similar to the negative control, with values of less than the 50:50 perceptibility threshold of the human eye.17 The greatest overall color change was observed for the professionally applied in-office whitening group, with no significant differences noted between the OTC and patient-applied home whitening groups.18
Another in vitro study evaluated the effect of various tooth whitening modalities on microhardness, surface roughness, and surface morphology of the enamel. While this study found that DIY whitening with strawberries did not affect surface roughness or surface morphology, it noted a significant reduction in microhardness.19
OVER-THE-COUNTER WHITENING
OTC whitening products provide consumers with a variety of materials and delivery methods, typically at less cost than in-office or professionally dispensed, at-home whitening therapies. Among the systems available, strip technology generally contains H2O2 as the active ingredient. In concentrations not exceeding 10%, it has been reported to be safe and effective.20 Earlier concerns of not attaching to the tooth properly, and inability to cover a wide arch, are being addressed with new seal technology.20 In vitro studies have shown that when applied on the outer enamel surface, the H2O2 in strips was able to reach the pulp cavity, demonstrating that the active agent diffuses into the enamel and dentin to interact with stain molecules deep within the tooth structure.21,22
DENTIST-DISPENSED, PATIENT-APPLIED HOME WHITENING
Dentist-dispensed, patient-applied home whitening is a well-established whitening procedure. It allows proper diagnosis, treatment planning, and professional supervision. It is relatively easy to perform, and may be less expensive than in-office whitening. Initially, it was used with 10% carbamide peroxide during nighttime bleaching sessions. A study of the kinetics of carbamide peroxide showed that it remains active for up to 10 hours, with about half of the active agent used up in the first 2 hours.23 Concentrations indicated for at-home whitening range between 10% to 35%. A 10% carbamide peroxide solution breaks down into 3.35% hydrogen peroxide and 6.65% urea. Urea further breaks down into ammonia and water, and may provide beneficial side effects—including slowing the caries process by increasing the pH value of the solution.6
Carbamide peroxide products usually contain either a carbopol or glycerine base. The carbopol base slows the release of hydrogen peroxide, making it more effective over a longer period.6 More recently, however, H2O2 products have been introduced for individuals who cannot tolerate wearing trays at night. The H2O2 concentration generally ranges from 7.5% to 9.5%, and the active time ranges from 30 minutes to 60 minutes; in addition, it can be applied during daytime.6
IN-OFFICE WHITENING
In-office whitening is the initial form of tooth whitening, and is performed with H2O2-based materials at concentrations of up to 40%. It is an alternative for patients who cannot tolerate trays, or who desire an instant whitening outcome and prefer to have the procedure performed in the office.
A study that evaluated the time required to achieve a six-tab difference on a Vita Classical shade guide found that in-office whitening produced the fastest results, followed by professionally supervised at-home whitening. The researchers noted that OTC whitening required the most time.24 That said, the use of high-concentration H2O2 materials associated with in-office whitening also resulted in generally higher incidence of dentinal hypersensitivity. Recently, manufacturers have attempted to address this issue by reducing concentration levels and changing the delivery method from gels to varnish systems.25
DENTINAL HYPERSENSITIVITY
Whitening procedures, whether over-the-counter or professional, can cause dentinal hypersensitivity and demineralization. Carbamide peroxide and H2O2 are able to penetrate through enamel and dentin. The majority of studies show that H2O2– and carbamide peroxide-containing products had no clinically significant adverse effects on enamel. However, two clinical cases did show significant enamel damage associated with the use of OTC whitening products.26–28 Eventually, upcoming in situ and in vivo studies will provide more evidence on this topic.29
In order to address the possible concerns of demineralization associated with whitening, several remineralization strategies using fluoride and calcium phosphate technologies have been suggested. Remineralization is the process whereby calcium and phosphate ions are supplied from a source externally to the tooth to promote ion deposition into the crystal voids in demineralized enamel to produce mineral gain.30 Calcium and phosphate ions are available in human saliva but the net remineralization may be too small and slow.29
Agents to promote remineralization, as well as reduce tooth sensitivity after whitening include fluoride, potassium nitrate, amorphous calcium phosphate (ACP), casein phosphopeptide-ACP, calcium sodium phosphosilicate, arginine calcium carbonate, and tri-calcium phosphate. Whether these active components truly assist in remineralization after whitening has yet to be determined. However, the application of topical fluoride post-whitening has been demonstrated to be effective in restoring the mineral content and microhardness values back to the baseline level.31,32
CONCLUSION
Tooth whitening is a dynamic process initiated by the movement of the active ingredient through the tooth structure, where it interacts with stain molecules and induces micromorphologic alterations on the tooth surface—and within the tooth—to affect the dentition’s optical properties.26 The development of, and continuous advances in, whitening materials and techniques reflect the efforts of the dental profession and industry toward preserving tooth structure and enhancing esthetics.
Clinicians and patients who initiate professional whitening treatment, as well as consumers who elect OTC therapy, will benefit from future innovations in whitening technology that are based on an improved understanding of the chemistry behind the tooth whitening process.
REFERENCES
- Haywood VB, Heymann HO. Nightguard vital bleaching. Quintessence Int. 1989;20:173–176.
- Gerlach RW. Shifting paradigms in whitening: introduction of a novel system for vital tooth bleaching. Compend Contin Educ Dent Suppl. 2000;29:S4–S9.
- Hoic D, Dixit N, Prencipe M, et al. The technology behind Colgate Simply White Toothpaste. J Clin Dent. 2004;15:37–40.
- Paravina RD, Powers JM. Esthetic Color Training in Dentistry. St. Louis, MO: Mosby; 2004.
- Goodkind RJ, Schwabacher WB. Use of a fiber-optic colorimeter for in vivo color measurements of 2830 anterior teeth. J Prosthet Dent. 1987;58:535–542.
- Hilton TJ, Ferracane JL, Broome JC. Summitt’s Fundamentals of Operative Dentistry. 4th ed. Hanover Park, IL: Quintessence; 2013:417,429,430.
- Hattab FN, Qudeimat MA, Al-Rimawi HS. Dental discoloration: An overview. J Esthet Dent. 1999;11:291–310.
- Nathoo SA. The chemistry and mechanisms of extrinsic and intrinsic discoloration. J Am Dent Assoc. 1997;128 Suppl:6S–10S.
- Dahl JE, Pallesen U. Tooth bleaching—a critical review of the biological aspects. Crit Rev Oral Biol Med. 2003;14:292–304.
- Peters MC. Strategies for noninvasive demineralized tissue repair. Dent Clin North Am. 2010;54:507–525.
- Hefferren JJ. Historical view of dentifrice functionality methods. J Clin Dent. 1998;9:53–56.
- Joiner A. Whitening toothpastes: A review of the literature. J Dent. 2010;38s:e17–e24.
- Hefferren JJ. A laboratory method for assessment of dentifrice abrasivity. J Dent Res. 1976;55:563–573.
- Schemehorn BR, Moore MH, Putt MS. Abrasion, polishing, and stain removal characteristics of various commercial dentifrices in vitro. J Clin Dent. 2011;22:11–18.
- Lobene RR. Effect of dentifrices on tooth stains with controlled brushing. J Am Dent Assoc. 1968;77:849–855.
- Macpherson LMD, Stephen KW, Joiner A, et al. Comparison of a conventional and modified tooth stain index. J Clin Periodontol. 2000;27:854–859.
- Douglas RD, Steinhauer TJ, Wee AG. Intraoral determination of the tolerance of dentists for perceptibility and acceptability of shade match. J Prosthet Dent. 2007;97:200–208.
- Kwon SR, Meharry M, Oyoyo U, Li Y. Efficacy of do-it-yourself whitening as compared to conventional tooth whitening modalities; an in vitro study. Oper Dent. 2015;40:E21–E27.
- Kwon SR, Kurti SR, Oyoyo U, Li Y. Effect of various tooth whitening modalities on microhardness, surface roughness and surface morphology of the enamel. Odontology. 2015;103:274–279.
- Oliveira GM, Miguez PA, Oliveira GB, et al. Safety and efficacy of a high-adhesion whitening strip under extended wear regimen. J Dent. 2013;41s:e46–e52.
- Gökay O, Müjdeci A, Algn E. Peroxide penetration into the pulp from whitening strips. J Endod. 2004;30:887–889.
- Bharti R, Wadhwani K. Spectrophotometric evaluation of peroxide penetration into the pulp chamber from whitening strips and gel: An in vitro study. J Conserv Dent. 2013;16:131–134.
- Matis BA. Degradation of gel in tray whitening. Compend Contin Educ Dent Suppl. 2000;S28,S31–S35.
- Auschill TM, Hellwig E, Schmidale S, Sculean A, Arweiler NB. Efficacy, side-effects and patients’ acceptance of different bleaching techniques (OTC, in-office, at-home). Oper Dent. 2005;30:156–163.
- Park S, Kwon SR, Qian F, Wertz PW. Evaluation of various in-office tooth whitening systems on hydrogen peroxide penetration. J Dent Res. 2016;(Spec Issue A):0635.
- Kwon SR, Wertz PW. Review on the mechanism of tooth whitening. J Esthet Restor Dent. 2015;27:240–257.
- Cubbon T, Ore D. Hard tissue and home tooth whiteners. CDS Rev. 1991;84:32–35.
- Hammel S. Do-it-yourself tooth whitening is risky. US News and World Report. 1998;66.
- Kwon SR, Li Y.Tooth whitening safety. Dimensions of Dental Hygiene. 2012;10(5):30–39.
- Cochrane NJ, Cai F, Huq NL, Burrow MF, Reynolds EC. New approaches to enhanced remineralization of tooth enamel. J Dent Res. 2010;89:1187–1197.
- Bizhang M, Seemann R, Duve G, et al. Demineralization effects of 2 bleaching procedures on enamel surfaces with and without post-treatment fluoride application. Oper Dent. 2006;31:705–709.
- da Costa JB, Mazur RF. Effects of new formulas of bleaching gel and fluoride application on enamel microhardness: an in vitro study. Oper Dent. 2007;32:589–594.
From Dimensions of Dental Hygiene. January 2018;16(01):18,21-23.

