Injury Prevention with Physical Therapy
An individually designed program provided by a physical therapist can help oral health professionals improve strength, flexibility, endurance, and patterns of posture and movement.
Ergonomics is the study of human performance (positioning and movement) and workplace design, such as equipment, ambience, and placement. The purpose of ergonomics is to maximize productivity by increasing safety, improving work quality, reducing operator fatigue and discomfort, and decreasing the risk of work-related musculoskeletal disorders (MSDs).1–3
Dental ergonomics focuses on dental workplace design—such as lighting, chairs, and dental equipment weights, sizes, and shapes—and also encompasses clinicians’ work postures and movements.4 Clinicians must make a concerted effort to adopt work postures that will provide optimal functioning.5,6 Body positioning, however, is also a psychomotor skill—meaning that muscular effort and activity must be learned in relation to the task.7 For a movement behavior to become automatic, the body must learn the skill beyond the cognitive level so that it can be performed without much thought.7
Clinicians perform skills as they have become accustomed, such as tightening muscles that should be loose while moving and using muscles that are poorly suited for such tasks. For example, keeping the head forward and shoulders rounded is common poor positioning in dentistry. The ideal posture is to keep the ear in line with the shoulder, which relaxes the shoulders and allows the arms to remain close to the body—enabling the operator to attend to what the hands are doing. In the poor posture, the trapezius muscle (in the neck and upper back) is working overtime to hold the head against gravity. The rounded shoulders make the arms move away from the body, increasing motion at the elbow to bring the hands toward and away from the body. A forward head and rounded shoulders force the trapezius muscle and shoulder abductor muscle to perform sustained holding, which can lead to muscular fatigue and pain. This position also hinders the effectiveness of the anterior muscles of the chest (pectorals), which should be moving the shoulders to bring the hands closer to the body. The ideal posture is arms at the sides, elbows flexed, and wrists and hands positioned to move and perform tasks.
MUSCULOSKELETAL PROBLEMS
MSDs are common among those providing oral health care services.5–9 Body positions are held for extended periods during the clinical practice of dental hygiene. For example, neck flexion—at least 30° of a head-down position—is maintained approximately 88% of the working day, while trunk flexion—at least 30° of bending forward—is held approximately 52% of the working day.4 These positions are maintained against gravity and demand more muscle effort. This increased effort can lead to muscle overload, decreased blood flow, and strain on the muscle tissue.
Muscle movement helps blood flow, while static postures reduce blood flow to the tissues. Blood flow delivers oxygen and nutrients to muscles and joints, ridding lactic acid buildup in the muscle tissue. It is the accumulation of lactic acid that can result in muscle soreness and tissue damage.10 Prolonged static posture, without movement into the other planes of motion, also causes muscles to become shortened, tight, and weak.
Highly repetitive movements with little or no muscle rest can also lead to fatigue, tissue damage, discomfort, and injury. Muscles and tendons become especially stressed with repetitive motion, which is damaging partially due to the force needed to perform the tasks—including precision control of instruments and equipment that may also vibrate. Fewer muscle units, which may also be carrying this load, are doing the task because of the precision control. The end results are changes to the muscle tissue itself, as well as disruption in blood flow, which causes fatigue and pain. Discomfort most often limits movement, leading to a continuous cycle of pain and a possible loss of motor functions and skills.10,11
Several studies4,6,9 have documented the prevalence of general MSD pain among oral health professionals. The reports of pain range from 64% to 93% of clinicians—which is an astounding two out of every three dental hygienists. MSD is most common among dental hygienists in the hand and wrist regions (60% to 69.5%).4,6 Shoulders, elbows, hips, knees, and ankles are also sites of MSD pain.9 Impairments to sensation and circulation can also cause functional losses, such as the ability to correctly grasp instruments.3
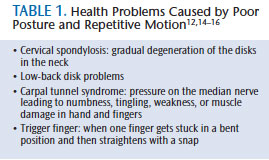
The likely cause of these physical problems centers on three factors: posture, repetitive motion, and force or pressure.2 Problems developing from awkward or poor posture include cervical spondylosis12 and lower-back disk problems, which are often coupled with sciatica.13 Carpal tunnel syndrome14 and trigger finger15 can develop from sustained forceful grips and repetitive wrist motion (Table 1).16
After a demanding workday, oral health professionals may experience fatigue in their muscles that requires proper rest. Consistent fatigue or discomfort is a sign that injury is likely or has already occurred.2 The first symptoms of MSDs are pain along with numbness and tingling.2 These symptoms frequently begin at the start of dental hygienists’ careers.4
ROLE OF PHYSICAL THERAPISTS

Applying ergonomic principles is one of the many tools used by physical therapists to help address and prevent musculoskeletal pain. Other health care professionals who use ergonomics include exercise physiologists, occupational therapists, and specially trained ergonomists who work with individuals and businesses on work-related injury and pain.2 Physical therapists, however, are uniquely positioned to assist individuals in the prevention and treatment of MSDs.
Physical therapists provide a comprehensive assessment and individualized treatment plan for each patient.17 This assessment often contains an analysis of postures and motion used in daily work activities. It can also include an assessment about and within the workplace (Figure 1). In the dental setting, physical therapists observe the dental patient position to ensure it is at the correct height for clinicians to keep their heads slightly flexed, which is aided by wearing loupes. Clinicians’ low backs should be straight. The lighting is also observed. Overhead lighting should be placed slightly left of the patient for best visibility. The workstation should include the placement of dental instruments within clinician reach to prevent overstretching. Along with the environment, physical therapists document dental professionals’ length of time in posture, dexterity, coordination with the dental instruments, and endurance for the task. Behaviors that signal muscular fatigue, stress, or pain—such as the repeated stretching of the neck, back, or shoulders—are also noted. By analyzing postural and movement patterns, the physical therapist assesses the quality and factors limiting the smooth execution and performance of movements. As necessary, further measures of strength, range of motion, sensation, muscular endurance, nerve integrity, and pain may be completed. The collection of this data enables the physical therapist to create an individualized program that may include training to preserve, enhance, or restore movement and physical function impaired or threatened by pain, injury, or disease.
Physical therapists focus their individualized programs on therapeutic exercise, including strengthening, stretching, patient education, and functional training.17 Evidence supports exercise for strengthening and endurance in the prevention and treatment of neck, back, and shoulder pain.18–21, While exercise is an effective method in prevention,3 it can also aggravate the problem. As such, oral health professionals should consult a medical provider before starting any exercise program.16
Functional training integrates motor learning (relatively permanent change in behaviors due to practice) and motor control (activation and coordination of muscular activity, such as how to move more efficiently) to help clinicians reduce pain and improve or restore appropriate posture and motion in their daily movements.22 Physical therapists can develop an individualized exercise program that is easily performed in the workplace and at home to prevent work-related disorders.2,3 They work to reduce the risk of expensive surgery and the need for long-term use of prescription medications. In addition, educating clinicians on how to prevent or manage an injury provides long-term health benefits.17 In most states, clinicians can seek out the care of a physical therapist directly, without a referral from a physician.23
FINAL RECOMMENDATIONS
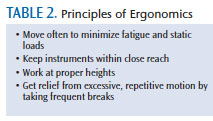
Prevention is the best defense against MSDs. Following the principles of ergonomics (Table 2) will decrease the risk of MSDs. Clinicians who experience MSD pain that is not relieved by rest should seek consultation from a licensed physical therapist. This consultation should include an individually designed program to help relieve pain while improving strength, flexibility, endurance, and patterns of posture and movement through exercise. The program will include actions that can be done at work or home. The physical therapist should also include suggestions for workplace redesign. Adhering to the principles of ergonomics is an ongoing practice that clinicians need to follow throughout their careers in order to keep MSDs at bay.
REFERENCES
- Gupta S. Ergonomic applications to dental practice. Indian J Dent Res. 2011;22:816–822.
- Thompson CR. Prevention Practice: A Physical Therapist’s Guide to Health, Fitness, and Wellness. Thorofare, NJ: Slack Inc; 2007.
- Noh H, Roh H. Approach of industrial physical therapy to assessment of the musculoskeletal system and ergonomic risk factors of the dental hygienist. J Phys Ther Sci. 2013;25:821–826.
- Hayes M, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hygiene. 2009;7:159–165.
- Valachi B. Dentistry shouldn’t be a pain in the neck: ergonomic and wellness strategies to prevent pain and extend your career. Available at: ineedce.com/courses/1742/PDF/DentistryShouldntbe_ergo.pdf Accessed March 20, 2014.
- ASL-Musculoskeletal Diseases. Prevalence of musculoskeletal disorder among dental practitioners. Available at: msd.ancientscienceoflife.org/ article.asp?issn=2231072X;year=2013;volume=1;issue=1;spage=22;epage=25;aulast=Dayakar. Accessed March 20, 2014.
- Wulf G, Shea C, Lewthwaite R. Motor skill learning and performance a review of influential factors. Med Educ. 2010;44:75–84.
- United States Department of Labor. Bureau of Labor Statistics. Nonfatal occupational injuries and illnesses requiring days away from work, 2012. Available at: bls.gov/news.release/pdf/osh2.pdf. Accessed March 20, 2014.
- Morse T, Bruneau H, Dussetscgleger J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work. 2010;35:419–429.
- Valachi B, Valachi K. Mechanisms leading to musculoskeletal disorders in dentistry. J Am Dent Assoc. 2003;134:1344–1350
- Valachi B, Valachi K. Preventing musculoskeletal disorders in clinical dentistry: strategies to address the mechanisms leading to musculoskeletal disorders. J Am Dent Assoc. 2003;134:1604–1612.
- American Academy of Orthopaedic Surgeons. Cervical Spondylosis (Arthritis of the Neck). Available at: orthoinfo.aaos.org/ topic.cfm?topic=A00369. Accessed March 20, 2014.
- MedlinePlus. Sciatica. Available at: nlm.nih.gov/medlineplus/ency/article/000686.htm. Accessed March 20, 2014.
- PubMed Health. Carpal tunnel syndrome. Available at: ncbi.nlm.nih.gov/pubmedhealth/ PMH0001469. Accessed March 20, 2014.
- Mayo Clinic. Diseases and Conditions: Trigger finger. Available at: mayoclinic.org/diseases-conditions/trigger-finger/basics/definition/CON-20043819. Accessed March 20, 2014.
- RGP Inc. An Introduction to Ergonomics: Risk Factors, MSDs, Approaches and Interventions. Available at: rgpdental.com/pdfs/topics_ ergonomics_paper(2).pdf. Accessed March 20, 2014.
- American Physical Therapy Association. Guide to Physical Therapists Practice. Available at: apta.org/search.aspx?q=Guide%20to%20practice. Accessed March 20, 2014.
- Kay TM, Gross A, Goldsmith CH, et al. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2013;8:CD004250.
- Choi BKL, Verbeek JH, Tam WW, Jiang JY. Exercises for prevention of recurrences of low-back pain. Cochrane Database Syst Rev. 2010:1;CD006555.
- Sihawong R, Janwantanakul P, Sitthipornvorakul E, Pensri P. Exercise therapy for office workers with nonspecific neck pain: a systematic review. J Manipulative Physiol Ther. 2011;34:62–71.
- Linton SJ, van Tulder MW. Preventive interventions for back and neck pain problems: what is the evidence? Spine. 2001;26:778–787.
- Schmidt R, Lee T. Motor Control and Learning: A Behavioral Approach. 5th ed. Champaign, Ill: Human Kinetics; 2011.
- American Physical Therapy Association. A summary of direct access language in state physical therapy practice acts. Available at: apta.org/uploadedFiles/APTAorg/Advocacy/State/Issues/Direct_Access/DirectAccessbyState.pdf. Accessed March 20, 2014.
From Dimensions of Dental Hygiene. April 2014;12(4):26,28–29.

