
Improve Your Ultrasonic Technique
Many factors contribute to a clinician’s ability to effectively remove calculus and help patients achieve optimal oral health.
The ability of ultrasonic instrumentation to remove calculus has been well documented. However, ultrasonic instrumentation is a technique-sensitive modality that is neither simple nor easy. Recognizing some of the common misconceptions regarding the use of ultrasonic scalers for calculus removal will help clinicians to optimize their ultrasonic technique to ensure effective patient care.
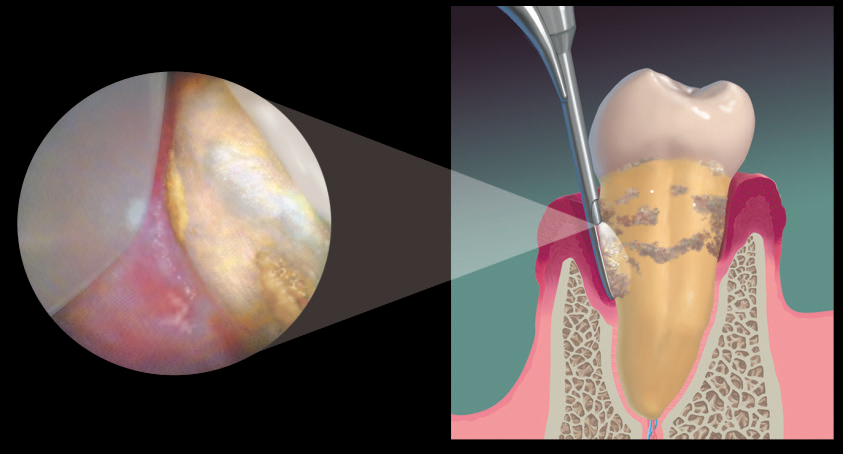
Many clinicians erroneously believe that ultrasonic scalers are much faster at removing deposits than hand instruments. The length of time required for effective deposit removal depends on many variables, such as location, quality, and quantity of the biofilm and calculus, and the extent of the disease. As demonstrated by the dental endoscope (Figure 1, page 38), successful root coverage by ultrasonic or hand instrumentation requires a methodical, comprehensive approach.1–3 Periodontal endoscopy has also confirmed that limitations exist with both hand scaling and ultrasonic instrumentation when calculus is detected solely by the use of an explorer.4
DEPOSIT TRAITS
Deposit traits play a role in the clinician’s ability to remove biofilm and calculus. Supragingival calculus differs from subgingival calculus in several aspects.5 Subgingival deposits are denser, harder, and tend to be more tenacious than supragingival calculus. The amount and variety of the calcium composition contribute to the ease of removal.6,7 Newly formed dental calculus tends to flake and crumble without difficulty during mechanical debridement. Veneered or burnished calculus requires more mindful and physical effort to remove.
The quantity of hard and soft deposits is related to the patient’s personal oral hygiene care, diet, and individual traits of his or her calculus.8 A high volume of deposits and increased difficulty in accessing them equate to longer treatment times.
STROKE WIDTH
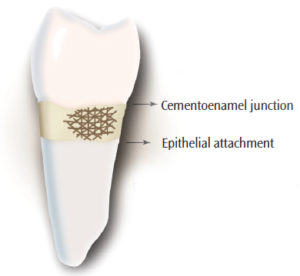
Regardless of the type of ultrasonic inserts/tips (UITs) used, the stroke width is only 1 mm to 2 mm.2,9 The stroke created by a UIT is comparable to the stroke created by a hand instrument.9 When the working end of an instrument is adapted to a tooth surface, it touches at the height of the contour and contacts at a tangent because the curvature of the tooth is either concave or convex.2,9Many overlapping, channeling strokes are equally necessary with ultrasonic instrumentation as with hand instrumentation to remove calculus. Both require a slow speed and a combination of overlapping vertical, oblique, and horizontal strokes (Figure 2).9 Slowing down the stroke allows the clinician to implement precise adaptation of the UIT and exercise better control of calculus removal. Therefore, strokes should be maintained within 1 mm sections for thorough coverage of the tooth surface.1,2,9,10
It is quite difficult to correctly adapt a precise stroke width when removing deposits that can’t be seen, and completing calculus removal without the aid of the dental endoscope (Figure 1) is virtually impossible. Periodontal endoscopy enables clinicians to improve their abilities to remove deposits, retain root structure, and slow periodontal disease progression.1,2
Although biofilm is a soft material, it still requires proper UIT adaptation, low to medium power, and proper technique for removal.8Longer and faster strokes are sufficient to displace loose biofilm supra- and subgingivally adjacent to the UIT. In order to disrupt adherent biofilm, the UIT must be in contact with the tooth surface using a slow, short, and vigilant stroke technique. The physical disruption and removal of adherent biofilm are only achieved with repeated strokes of a UIT in direct contact with every aspect of the tooth surface.1,2,9
GRASP AND ACTIVATION PRESSURE
Proper use of ultrasonic instrumentation involves using suitable grasp pressure and applied pressure against the deposit being removed. Clinicians mistakenly use ultrasonics with a very relaxed pen grasp and light to moderate pressure to maximize the vibration activation of the UIT, regardless of the type and volume of deposits. A gentle, exploratory pressure increases tactile sensitivity and is sufficient for nontenacious, light to moderate spicule deposits. Moderate to heavy, tenacious, or burnished calculus requires more of a modified pen grasp to apply pressure against the peripheral edge toward the calculus deposit. Some calculus pieces cannot be eradicated without the application of moderate to firm pressure and an adequate amount of time. A firm grasp will impede stroke activation and strong pressure may dampen the UIT displacement, reducing the stroke pattern and decreasing efficacy.11,12 Therefore, applying the appropriate amount of pressure in accordance to the size and tenacity of the calculus is necessary to achieve appropriate outcomes.
INSERT/TIP AND POWER SELECTION
Choosing the proper UIT for the task at hand is integral to deposit removal. Many clinicians prefer slim or thin UITs, but most are not designed to withstand the high power necessary for removing moderate to heavy or tenacious calculus deposits. Using more than one type of UIT (standard and thin straight or curved UIT combination) is the best option, as the clinician moves supragingivally to subgingivally, or from heavier to lighter deposits.13 Thin UITs are available that may be used with higher power.
Along with proper UIT selection, power settings must be at levels suitable to remove the amount and type of calculus present. The lowest power level that will efficiently remove soft and hard deposits should be used. When higher power levels are needed, anesthesia should be administered. Some clinicians tend to use low power to prevent discomfort, but UITs used consistently on low power frequently burnish calculus, instead of removing it.8 The rapid oscillation of the UIT, even at low power settings, can give the false impression that biofilm and calculus are easily removed. Lavage and flushing of unattached remnants do occur; however, underlying attached biofilm and calculus deposits remain on the root surface until they are physically disrupted.1Low to medium power settings are sufficient for light to moderate calculus and high power is indicated for tenacious or burnished calculus.12
In conjunction with a high power setting, proper tip adaptation is fundamental to calculus removal.9 The tip of the UIT should be held slowly and directly on the outer ledges of tenacious calculus in order to fracture the deposit.11 Using the tip of the UIT directly on the calculus deposit is the only way to remove tenacious and burnished calculus. However, continuing to use the UIT once the deposit has been removed may damage the root surface.
Checking UIT wear length regularly is imperative to deposit removal, as using worn UITs may lead to burnished or residual calculus. Although the UIT may oscillate, the amount of movement generated by a worn UIT is difficult to ascertain. Most UITs with a 1 mm reduction in length are decreased in effectiveness by 25%, and a 2 mm reduction decreases efficacy by 50%.10 A shortened UIT can affect the vibration displacement, amplitude, and oscillation, thereby diminishing ultrasonic scaling performance.13
CONCLUSION
Clinicians with an in-depth understanding of ultrasonic instrumentation are well prepared to help their patients achieve optimal oral health. Thorough removal of calculus deposits is crucial to the management of periodontal diseases. UITs are constantly evolving to allow clinicians to refine their technique for better results. Adding the advanced technology of a dental endoscope be a necessary adjunct to future clinical care.
REFERENCES
- Kiehl N. The keys to successful power instrumentation. Dimensions of Dental Hygiene. 2012;10(7):42–48.
- Pattison AM, Matsuda SA, Kiehl N. Ultrasonic therapy in the 21st century. Dimensions of Dental Hygiene. 2014;12(7):40–44.
- Kiehl N. 5 Myths about periodontal instrumentation. Dimensions of Dental Hygiene. 2011;9(11):68–70.
- McConaughy F. Advances in visual acuity. Dimensions of Dental Hygiene. 2017;15(6):28–30.
- Boyd LD, Wilkins EM. Nonsurgical periodontal therapy and adjunctive therapy. In: Clinical Practice of the Dental Hygienist. 12th ed. Philadelphia: Wolters Kluwer; 2016.
- White DJ. Dental calculus: recent insights into occurrence, formation, prevention, removal and oral health effects of supragingival and subgingival deposits. Eur J Oral Sci. 1997;105:508–522.
- LeGeros RZ, Rohanizadeh R, Lin SJ, et al. Dental calculus composition following use of essential-oil/ZnCl2 mouthrinse. Am J Dent. 2003;16:155-60.
- Eastabrooks D. Oral hygiene assessment: soft and hard deposits. In: Dental Hygiene: Theory and Practice. 4th ed. St. Louis: Saunders/Elsevier; 2015.
- Hand and Utrasonic Scaling Stroke Comparison (Online Streaming Videos). Los Angeles: Pattison Institute LLC; 2014.
- Stach D. The five most common errors when using ultrasonic inserts. Dimensions of Dental Hygiene. 2010;8(7):46–50.
- Hodges KO. Ultrasonic instrumentation. In: Dental Hygiene: Theory and Practice. 4th ed. St. Louis: Saunders/Elsevier; 2015.
- Jahn CA. Sonic and ultrasonic instrumentation and irrigation. In: Carranza’s Clinical Periodontology. 12th ed. St. Louis: Elsevier Saunders; 2015.
- Lea SC, Landini G, Walmsley AD. The effect of wear on ultrasonic scaler tip displacement amplitude. J Clin Periodontol. 2006;33:37–41.
Featured image by KIRILL4MULA/ISTOCK/GETTY IMAGES PLUS
From Dimensions of Dental Hygiene. October 2017;15(10):36,38.

