 INGRAM PUBLISHING/GETTY IMAGES PLUS
INGRAM PUBLISHING/GETTY IMAGES PLUS
The Importance of Effective Scaling and Root Planing
High-quality instrumentation in addition to good self-care, appropriate re-evaluations, and additional treatment are key components of a successful periodontal treatment regimen.
This course was published in the August 2021 issue and expires August 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain the roles of subgingival calculus and biofilm in persistent periodontal inflammation.
- Discuss the limits to traditional, blind scaling and root planing (SRP).
- Identify determination criteria and approaches to therapy for sites that fail to respond adequately to traditional, blind SRP.
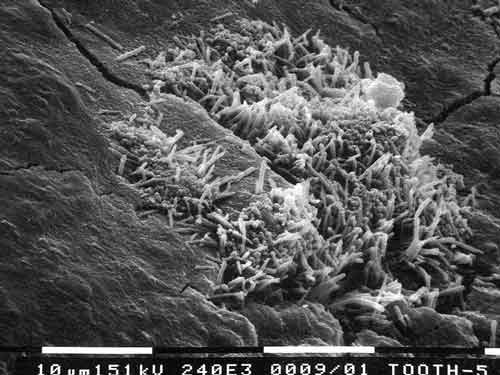
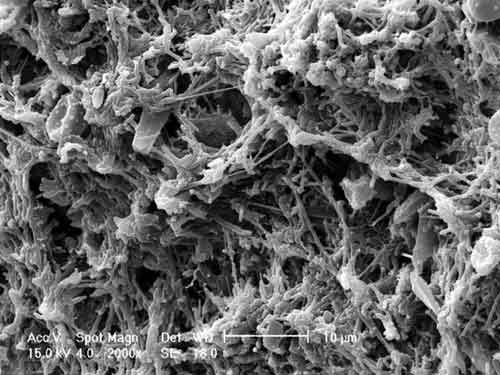
Periodontal diseases are a worldwide public health burden.1 Undiagnosed, untreated, or inappropriately treated periodontitis can have devastating effects on oral health, quality of life, and overall health. The destructive effects and systemic impacts of periodontitis are the result of inflammation. Oral inflammation can cause tooth loss and has been linked to numerous systemic health problems. Inflammation results from the interaction of a host’s immune system and dysbiotic subgingival biofilms. Dysbioses are problematic disruptions of normal flora. Figure 1 and Figure 2 are scanning electron micrographs depicting a typical subgingival biofilm. Dysbioses seem initiated by the interactions of certain microbes, such as Porphyromonas gingivalis and Filifactor alocis.2,3 Alternately Bartold and Van Dyke proposed that inflammation itself is responsible for controlling the composition of biofilms.4 Hajishengallis also discussed the concept that inflammation supports the growth of dysbiotic microbial communities.5 Regardless of which hypothesis is correct, dysbiotic microbial communities coupled with hosts’ inflammatory responses can result in degradation of the periodontium.
The traditional first step in periodontal therapy involves eliminating subgingival biofilm and calculus to resolve periodontal inflammation. Success requires effective self-care and thorough subgingival debridement, including scaling and root planing (SRP), that may need to be repeated over time.
Scaling and Root Planing and Subgingival Biofilms
The goal of SRP is to remove subgingival calculus and biofilm.6 Numerous studies have confirmed the significant reduction of subgingival bacteria following SRP.7 Smooth or burnished calculus, circuitous periodontal pockets, irregular roots, and a lack of visibility make SRP a demanding procedure for even accomplished clinicians.
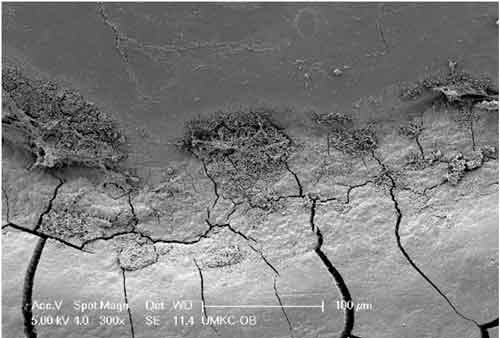
When performed effectively, SRP can reduce subgingival biofilm, clinical inflammation, and probing depths. However, studies evaluating SRP effectiveness indicate that many teeth exhibit residual subgingival biofilm and calculus.8 Deeper probing depths, root concavities, grooves, restorative contours, and furcation involvements reduce efficacy. As seen in Figure 3, the cementoenamel junction (CEJ) is a common site for residual calculus. No specific type of instrumentation has demonstrated consistent superiority, be it manual, ultrasonic/sonic, or lasers.9 The most important factors affecting SRP efficacy are operator experience, skill, and training.
No treatments can completely eradicate all bacteria. Limited visibility, restricted access, tissue invasion of certain microbes, and inaccessible biofilm retained in surface irregularities all impact the effectiveness of treatment.10 Previously treated sites may also be re-infected by bacteria from untreated sites, saliva, epithelium of the periodontal pocket wall and/or oral and pharyngeal mucosa, and even from other individuals.11,12
Bacterial recolonization begins almost immediately following subgingival instrumentation.13,14 Post-treatment bacterial counts may reach pretreatment levels within a week.15 Initially, nonpathogenic microbes may replace periodontal pathogens.15–17 The intervals necessary for sites to return to pretreatment levels of subgingival microflora depend on disease severity, thoroughness of debridement, and supportive care.17 Thus, preventing the rebound of pathogenic bacteria requires meticulous self-care and repeated removal of subgingival biofilms at appropriate intervals.
Subgingival Dental Calculus
Dental calculus is considered mineralized oral biofilm.18,19 Calculus is porous, allowing bacteria to thrive on and inside it.19–21 The presence of subgingival calculus is strongly associated with inflammation in the soft tissue pocket wall and is an important factor in the development and progression of periodontitis.18,22,23 Subgingival calculus provides surfaces that are, in turn, conducive to adherence and growth of biofilms.24 Calculus is a reservoir for endotoxins and microbial antigens.21,25 Incomplete removal of subgingival calculus leaves a residuum that contributes to reinfection of the periodontal pocket and the recurrence of periodontitis.25
Characteristics of Diseased Root Surfaces
A root no longer protected by the periodontal ligament or junctional epithelium is readily colonized by bacteria that may, over time, result in mature biofilm and subgingival calculus. Exposed root surfaces are uneven and hypermineralized. Lacunae, resorptive defects, and mounds are common.
Bacterial lipopolysaccharide (endotoxin) penetrates and adsorbs to the roots of periodontally diseased teeth.26 Attachment loss also exposes cementum into which biologically active products can diffuse. Although weakly bound, endotoxin can wreak havoc on healing following inadequate periodontal therapy.27 Bench studies have demonstrated that the removal of surface endotoxin via manual or ultrasonic instrumentation or by rinsing are all effective. Unfortunately, SRP alone does not fully eliminate endotoxins. Retoxification of treated surfaces may occur quickly, reinforcing the need for brief intervals between periodontal maintenance appointments.
Removal of Subgingival Calculus: Instrumentation
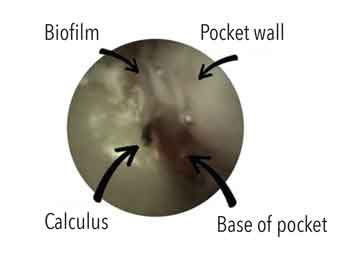
Ease of calculus removal is related to location, hardness, composition, mode of attachment, and instrument sharpness. These factors are mediated by biofilm and surface irregularities. Given the difficulties of removing subgingival calculus during SRP, debates regarding optimal instrumentation focus on manual vs ultrasonic and/or sonic instrumentation vs fine-grained tapered finishing burs.28 A related debate centers on removal of residual cementum and underlying dentin by overly aggressive instrumentation of the root surface. Thus, clinicians often face a conundrum, namely trying to blindly remove as much subgingival biofilm and calculus as possible seeking to achieve a biocompatible smooth root surface without removing excessive amounts of tooth material. Such challenges led to the development of advanced instruments, such as periodontal endoscopes and a videoscope.22,23,29,30 The use of periodontal endoscopes or videoscopes by a skilled clinician can reduce the need for traditional periodontal surgeries.31,32 Figure 4 depicts a view of retained calculus through a periodontal endoscope.
Studies comparing manual to ultrasonic instrumentation with or without surgical flap reflection report no significant differences between the two.28,33 Studies also reveal that neither method removes all subgingival biofilm.28,34 The combined use of curets and an ultrasonic scaler appears more effective than either method alone. Studies show that regardless of the type of instruments employed, experienced clinicians are more effective at removing subgingival calculus. Furcations, CEJ, interproximal root flutings, deeper pockets, and multirooted teeth are most likely to exhibit residual calculus following SRP. Better results are more likely when manual and ultrasonic instrumentation are combined or when either is followed by subgingival powder air-polishing.34,35 Although ineffective against calculus, air-powder polishing using glycine or erythritol powders appears as effective as other approaches for removal of subgingival biofilms.35,36
Lasers are among the most recent additions to the armamentarium. Lasers, either as a monotherapies or as adjuncts, have been used to mitigate SRP’s traditional inadequacies in the hope of increasing desired clinical outcomes.37 There is an absence of strong evidence supporting the effectiveness of lasers as adjuncts to SRP.7,38,39 More high-quality research is needed in this area.
Re-evaluation and Periodontal Maintenance Therapy
Periodontal maintenance must meet or exceed the norm. Repeated re-assessment is necessary to determine if different approaches are warranted. Assessment of nonsurgical therapy is complicated by three variables. First, removing all subgingival biofilm and calculus is demanding and may be impossible. Second, detecting subgingival calculus is difficult. Third, the quality of self-care is inconsistent. Absent good self-care, it’s difficult to determine whether persistent signs of inflammation are caused by supra- or subgingival etiologies.
Sherman et al40 looked at the detection of subgingival calculus via tactile perception. They reported a high false negative response (77.4%) when comparing clinical reports of calculus-free root surfaces vs low-magnification microscopic evaluation of those same surfaces. Tactile perceptions of the subgingival environment lack sensitivity, specificity, and reproducibility. Put simply, if root calculus can’t be seen, it can’t be reliably detected. And even if detected, the inability to see the tooth surface offers no assurance that the calculus has been removed. This often results in residual calculus and over-instrumentation (excessive removal of cementum or dentin), or both.
The interval between completion of nonsurgical periodontal therapy (ie, SRP) and the first re-evaluation appointment should be long enough to allow near-complete healing of treated sites. The connective tissues of an inflamed gingival lamina propria may require as many as 12 weeks of healing following SRP. Re-evaluation is not an endpoint but a waypoint. Re-evaluation of any periodontal treatment, including SRP, requires a reassessment of the same clinical parameters used to diagnose disease and to construct the original treatment plan.41 Two important aspects of re-assessment can be viewed in the context of studies that revealed that bleeding on probing is not a completely reliable prognostic indicator for subsequent attachment loss, and sites consistently free of bleeding on probing (the desired results of adequate SRP combined with good self-care) will not incur subsequent attachment loss.42 These studies provide an important clinical goal; however, they were of limited duration, which further suggests that the presence of persistent bleeding on probing bodes poorly for a site. Along the same lines, special attention must be focused on furcation involvements, particularly those with bleeding on probing. This is because such sites may experience rapid attachment loss. Long-term data revealed that furcation involvement approximately doubles the risk of tooth loss for molars over 10 years to 15 years. In spite of this observation, most molars with a furcation involvement will respond favorably to periodontal therapy if adequately instrumented and in the presence of good self-care, resulting in the consistent elimination of bleeding on probing.
Results of reassessment determine the next steps in treatment. This is likely to be periodontal maintenance or a second SRP at nonresponding, still-diseased sites. A second SRP is often more successful if performed using advanced instrumentation designed to improve operator visibility. The second SRP should be followed by another re-evaluation appointment. If diseased sites persist (generally assessed by the presence of bleeding on probing) at this appointment, the next step may be surgical intervention.
Surgical treatment typically seeks improved access for removal of subgingival calculus and biofilm. Figure 5 depicts the limits to blind SRP, despite radiographs that show subgingival calculus. Here, the dental hygienist did a good job of blind SRP but the teeth continued to display signs of inflammation at re-evaluation. Access surgery was performed. Note the discoloration at CEJ sites suggesting retained calculus as well as sheets of thin, brownish calculus on root surfaces apical to those debrided via blind SRP. Figure 6 depicts a similar situation in a different patient.
Some surgeries may also employ regenerative technologies or tissue sculpting aimed at providing better support or tissue anatomy that is more easily maintained. Other surgical procedures may improve appearance and mitigate chronic pain. In recent years, minimally invasive surgeries have facilitated improved SRP and regenerative opportunities at some sites, but they necessitate use of advanced instrumentation that improves visualization and instrumentation.
Like other chronic diseases, the ongoing nature of periodontitis requires meticulous re-evaluations and modulations of subsequent care, including maintenance. The initial interval between maintenance appointments should be based on a patient’s risk for disease recurrence. Factors such as residual probing depths, persistent bleeding on probing, erratic or inadequate self-care, and failure to appear at periodontal maintenance appointments are signals of greater risk.43

Unfortunately, many practices still adhere to a “soft-tissue management protocol” consisting of SRP, a 4-week to 6-week re-evaluation, and near-automatic assignment to a periodontal maintenance program with 6-month intervals. Although this may succeed for a few patients and insurance companies, it will not work for most. Dockter et al44 reported that treatment of periodontitis in general dental practices varied little regardless of disease severity or risk of subsequent disease. They also reported that the average number of periodontal maintenance appointments was fewer than what research considers appropriate for patients with moderate to advanced periodontitis. Unfortunately, periodontal diseases are often not managed properly or in a timely manner.44,45 If clinical procedures, such as SRP, do not produce desired results, other therapies should be considered as well as referral to a specialist.
The effectiveness of SRP and patient-centered maintenance is supported by a 2015 American Dental Association-commissioned systematic review and clinical practice guidelines that addressed the nonsurgical treatment of chronic periodontitis with and without adjunctive therapies.7,46 On average, SRP is a remarkably effective treatment if executed with precision by skilled clinicians.

Conclusions
Based on published evidence, the following conclusions are reasonable:
- Subgingival calculus and root surface irregularities are replete with biofilm composed of metabolically active bacteria.
- Removing subgingival bacterial and calculus helps create biologically compatible root surfaces. Thorough and judicious root planing can eliminate such deposits. Endotoxin adsorbs to tooth surfaces but is easily removed once deposits are eliminated. Numerous clinical studies have documented the beneficial effects of complete removal of subgingival calculus on the resolution of inflammation.34
- Periodontal destruction appears related to the presence of calculus.19,20,22,23,25
- SRP is a difficult task, especially in sites with deeper probing depths. It can often be performed well only by highly skilled clinicians who may need advanced instrumentation to ensure appropriate visualization of subgingival tooth surfaces.30,32,47 Effective SRP demands thorough calculus removal. Complete removal of subgingival cementum should not be a goal of periodontal therapy but is often inevitable.33
- Inflammation associated with periodontitis adversely affects not only the oral environment, but also systemic health. This observation reinforces the importance of effective SRP, high-quality self-care, appropriate re-evaluations, and further treatment if indicated. The need for periodontal maintenance remains as long as patients have teeth (or implants). Initial maintenance intervals should trend toward too-often rather than too-seldom with an eye toward increasing maintenance intervals when clinical needs permit.
- Goals of SRP include complete removal of calculus and biofilm, smoothing root surfaces, eliminating bleeding on probing (necessitating effective self-care), reducing probing depths, increasing clinical attachment levels, and eliminating inflammation thereby reducing systemic inflammatory burden.
- An astute clinician will treat periodontitis using appropriate instrumentation, monitor results of treatment via periodic re-evaluations, and perform appropriate and timely treatments and retreatments of recurrent disease as needed.48
- Finally, SRP is one of numerous approaches available to arrest periodontitis and restore health. If a single session or multiple sessions of SRP do not achieve waypoints indicative of health and stability, other effective therapies must be provided or referral to a specialist is indicated.
References
- Eke PI, Thornton-Evans GO, Wei L, Borgnakke WS, Dye BA, Genco RJ. Periodontitis in US adults. National Health and Nutrition Examination Survey 2009-2014. J Am Dent Assoc. 2018;147:576–588.
- Lamont RJ, Hajishengallis G. Polymicrobial synergy and dysbiosis in inflammatory disease. Trends Molec Med. 2015;21:172–183.
- Aruni AW, Mishra A, Dou Y, Chioma O, Hamilton BN, Fletcher HM. Filifactor alocis—a new emerging periodontal pathogen. Microbes Infect. 2015;17:517–530.
- Bartold PM, Van Dyke TE. An appraisal of the role of specific bacteria in the initial pathogenesis of periodontitis. J Clin Periodontol. 2019;46:6–11.
- Hajishengallis G. The inflammophilic character of the periodontitis associated microbiota. Mol Oral Microbiol. 2014;29:248–257.
- Ishikawa I, Baehni P. Nonsurgical periodontal therapy—where do we stand now? Periodontol 2000. 2004;36:9–13.
- Smiley CJ, Tracy SL, Abt E, et al. Systematic review and meta-analysis on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J Am Dent Assoc. 2015;146:508–524.
- Heitz-Mayfield LJ, Trombelli L, Heitz F, Needleman I, Moles D. A systematic review of the effect of surgical debridement vs. non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol. 2002;29(Suppl 3):92–102.
- Cobb CM. Lasers and the treatment of periodontitis: the essence and the noise. Periodontol 2000. 2017;75:205–295.
- Adriaens PA, Adriaens LM. Effects of nonsurgical periodontal therapy on hard and soft tissues. Periodontol 2000. 2004;36:121–145.
- Quirynen M, De Soete M, Dierickx K, van Steenberghe D. The intra-oral translocation of periodontopathogens jeopardizes the outcome of periodontal therapy. A review of the literature. J Clin Periodontol. 2001;28:499–507.
- Greenstein G, Lamster I. Bacterial transmission in periodontal diseases: A critical review. J Periodontol. 1997;68:421-431.
- Magnusson I, Lindhe J, Yoneyama T, Liljemberg B. Recolonization of a subgingival microbiota following scaling in deep pockets. J Clin Periodontol. 1984;11:193–207.
- Cugini MA, Haffajee AD, Smith C, Kent RL, Socransky SS. The effect of scaling and rootplaning on the clinical and microbiological parameters of periodontal diseases: 12 month results. J Clin Periodontol. 2000:27:30–36.
- Petersilka GJ, Ehmke B, Flemmig TF. Antimicrobial effects of mechanical debridement. Periodontol 2000. 2002;28:56–71.
- Harper DS, Robinson PJ. Correlation of histometric, microbial, and clinical indicators of periodontal disease status before and after root planing. J Clin Periodontol. 1987;14:190–196.
- Shiloah J, Patters MR. Repopulation of periodontal pockets by microbial pathogens in the absence of supportive therapy. J Periodontol. 1996;67:130–139.
- Akcali A, Lang NP. Dental calculus: The calcified biofilm and its role in disease development. Periodontol 2000. 2018;76:109–115.
- Tan BTK, Mordan NJ, Embleton J, Pratten J, Galgut PN. Study of bacterial viability within human supragingival dental calculus. J Periodontol. 2004;75:23–29.
- Moolya NN, Thakur S, Ravindra S, Setty SB, Kulkarni R, Hallikeri K. Viability of bacteria in dental calculus—a microbiological study. J Indian Soc Periodontol. 2010;14:222–226.
- Galgut PN, Mordan N, Newman HN. A transmission electron microscopy study of supragingival calculus. J Int Acad Perio. 2001;3:31–37.
- Wilson TG, Harrel SK, Nunn ME, Francis B, Webb K. The relationship between the presence of tooth-borne subgingival deposits and inflammation found with a dental endoscope. J Periodontol. 2008;79:2029–2035.
- Wilson TG, Carnio J, Schenk R, Myers G. Absence of histologic signs of chronic inflammation following closed subgingival scaling and root planing using the dental endoscope: human biopsies—a pilot study. J Periodontol. 2008;79:2036–2041.
- Nyman S, Westfelt E, Sarhed G, Karring T. Role of diseased root cementum in healing following treatment of periodontal disease. A clinical study. J Clin Periodontol. 1988;15:464–468.
- Mandel ID. Calculus update: prevalence, pathogenicity and prevention. J Am Dent Assoc. 1995;126:573–580.
- Hughes FJ, Smales FC. The distribution and quantitation of cementum-bound lipopolysaccharide on periodontally diseased root surfaces of human teeth. Arch Oral Biol. 1990;35:295–299.
- Pitaru S, Soldinger M, Madgar D, Metzger Z. Bacterial endotoxin inhibits migration, attachment, and orientation of human gingival fibroblasts in vitro and delays collagen gel contraction. J Dent Res. 1987;66:1449–1455.
- Oda S, Nitta H, Setoguchi T, Izumi Y, Ishikawa I. Current concepts and advances in manual and power-driven instrumentation. Periodontol 2000. 2004;36:45–58.
- Michaud RM, Schoolfield J, Mellonig JT, Mealey BL. The efficacy of subgingival calculusremoval with endoscopy-aided scaling and root planing: a study on multirooted teeth. J Periodontol. 2007;78:2238–2245.
- Kuang Y, Hu B, Chen J, Feng G, Song J. Effects of periodontal endoscopy on the treatment of periodontitis: A systematic review and meta-analysis. J Am Dent Assoc. 2017;148:750–759.
- Harrel SK, Wilson TG Jr, Rivera-Hidalgo F. A videoscope for use in minimally invasive periodontal surgery. J Clin Periodontol. 2013;40:868–874.
- Harrel SK, Nunn ME, Abraham CM, Rivera-Hidalgo F, Shulman JD, Tunnell JC. Videoscope assisted minimally invasive surgery (VMIS): 36-month results. J Periodontol. 2017;88:528–535.
- Drisko CL, Cochran DL, Blieden T, et al. Position paper: sonic and ultrasonic scalers in periodontics. Research, Science and Therapy committee of the American Academy of Periodontology. J Periodontol. 2000;71:1792–1801.
- Cobb CM. Non-surgical pocket therapy: mechanical. Ann Periodontol. 1996;1:443–490.
- Wennstrom JL, Dahlen G, Ramberg P. Subgingival debridement of periodontal pockets by air-polishing in comparison with ultrasonic instrumentation during maintenance therapy. J Clin Periodontol. 2011;38:820–827.
- Flemmig TF, Arushanov D, Daubert D, Rothen M, Mueller G, Leroux BG. Randomized controlled trial assessing efficacy and safety of glycine powder air polishing in moderate-to-deep periodontal pockets. J Periodontol. 2012;83:444–452.
- Ishikawa I, Aoki A, Takasaki AA, Mizutani K, Sasaki KM, Izumi Y. Application of lasers in periodontics: true innovation or myth? Periodontol 2000. 2009:50:90–126.
- Chambrone L, Ramos UD, Reynolds MA. AAP best-evidence consensus on infrared laser wavelengths for the treatment of moderate to severe periodontitis. A systematic review and meta-analysis. J Periodontol. 2018;89:743–765.
- Mills MP, Rosen PS, Chambrone L, et al. The efficacy of laser therapy used alone or as an adjunct to non-surgical and surgical treatment of periodontitis and peri-implant diseases: an AAP best-evidence consensus report. J Periodontol. 2018;89:737–742.
- Sherman PR, Hutchens LH Jr, Jewson LG, Moriarty JM, Greco GW, McFall WT Jr. The effectiveness of subgingival scaling and root planing. I. Clinical detection of residual calculus. J Periodontol. 1990;61:3–8.
- Claffey N. Decision making in periodontal therapy. The re-evaluation. J Clin Periodontol. 1991;18:384–389.
- Lang NP, Adler R, Joss A, Nyman S. Absence of bleeding on probing. An indicator of periodontal stability. J Clin Periodontol. 1990;17:714–721.
- Ramseier CA, Nydegger M, Walter C, et al. Time between recall visits and residual probing depths predict long‐term stability in patients enrolled in supportive periodontal therapy. J Clin Periodontol. 2019;46:218–230.
- Dockter KM, Williams KB, Bray KS, Cobb CM. Relationship between pre-referral periodontal care and periodontal status at time of referral. J Periodontol. 2006;77:1708–1716.
- Cobb CM, El-Annan E, Carrara A, et al. Periodontal referral patterns, 1980 vs 2000: a preliminary study. J Periodontol. 2003;74:1470–1474.
- Smiley CJ, Tracy SL, Abt E, et al. Evidence-based clinical practice guideline on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J Am Dent Assoc. 2015;146:525–535.
- Drisko CL, Killoy WJ. Scaling and root planing: Removal of calculus and subgingival organisms. Curr Opin Dent. 1991;1:74-80.
- Rethman M. Open forum digest. AAP Connect. October 3, 2019.
From Dimensions of Dental Hygiene. August 2021;19(8):40-44.



