 DENIZA/ISTOCK/GETTY IMAGES PLUS
DENIZA/ISTOCK/GETTY IMAGES PLUS
Impact of Loupes and Lights on Visual Acuity and Ergonomics
Using loupes and lights may help clinicians compensate for visual deficiencies and improve ergonomics, possibly increasing career longevity.
Visual acuity is imperative to performing precise movements during clinical care and sustaining proper ergonomics. According to the American Optometric Association, visual acuity refers to the clarity or the sharpness of vision.1 Dental hygienists perform clinical care in the oral cavity with a restricted field of vision due to limited space and lighting.2,3 As part of clinical practice, dental hygienists use visual motor integration to control eye and hand coordination to perform precise movements.2–4 When visual acuity is deficient, it impacts a dental hygienist’s ability to accurately assess disease of the hard and soft tissues, read the periodontal probe, and evaluate radiographs, among other challenges.2,5,6 Furthermore, visual acuity declines with age, and dental hygienists may compensate their ergonomics to enhance their field of vision.7
Impact of Visual Acuity on Ergonomic Practice and Health
Ergonomic health and visual acuity are topics of concern for dental hygienists.8,9 Dental hygienists are practicing longer and relying on the overall strength of their bodies to increase their work longevity. Visual deficiencies may impact postural positioning, compromising ergonomic health and increasing the risk for musculoskeletal disorders (MSDs).3,4 The risk for MSDs is increased by prolonged static positions, repetitive instrumentation, and limited field of vision.2–4 MSD-related pain and injury are associated with the number of hours practiced weekly, and often affect the spine, shoulders, and neck.3,8 Because dental hygienists are remaining in clinical practice longer, the clarity and sharpness of vision are of even greater importance as poor vision affects postural positioning and, ultimately, compromises balance.2
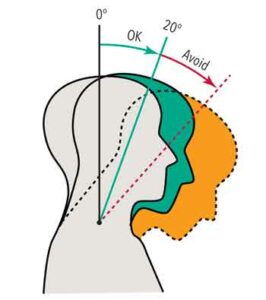
Visual deficiencies may result in the head tilted forward, over-exerted neck flexion, and lack of balance. A neutral neck position should be maintained during clinical care, which encompasses a head tilt range of 0° to 15° and a neck flexion of 0° to 20°. Dental hygienists’ neck flexion is often beyond 20°, causing neck pain (Figure 1).3,10,11 In addition, for every inch the head is tilted forward and the neck is flexed, the weight of the head also increases.12 This adds additional stress and strain to the cervical muscles of the neck and initiates a domino effect of abnormal forces to the spine, compromising ergonomic health.13
Maintaining a neutral neck position can be challenging as visual acuity declines with age. The risk of visual deficiencies—such as presbyopia, or farsightedness—increases especially among clinicians older than 40. Presbyopia is caused by the loss of elasticity in the lens of the eye, which makes it challenging to focus on objects in close range.7,14
Dental hygienists maintain a short working distance from the oral cavity (27 cm to 50 cm), which requires clarity and sharpness of vision.1,15 Clarity and sharpness are not only required for clinical patient care, but for other tasks as well, such as viewing radiographs or computer monitors farther away. In addition, the expansion of electronic displays in dental settings, as well as prolonged personal electronic use, enhances eye strain, discomfort, and ocular surface changes.16 Visual deficiencies caused by age and blurred vision from presbyopia impact the ability to focus on objects in various ranges during patient care.
Loupes and Lights for Improved Visual Acuity and Ergonomic Practice
The use of loupes is an evidence-based strategy to improve clinical performance and ergonomics.17–19 In dentistry, both Galilean and Keplarian telescope systems are used. The Keplarian prismatic loupes have a higher magnification compared to the Galilean. Because of their 3.5x up to 8.0x magnification, Keplarian loupes have longer barrels and are heavier than Galilean loupes. Galilean loupes, which are the most commonly used for dental hygiene procedures, offer a magnification range from 2.0x to 3.5x. With a concave lens and a convex lens, Galilean loupes produce a more distinct image than a single lens.20
Dental hygienists are relying on the overall strength of their bodies to increase their work longevity.
Panoramic loupes with a 3.5x magnification are also available. The panoramic lens is rectangular, allowing for increased peripheral vision, doubling the Keplarian prismatic viewable area. This type of loupe may be ideal to see more teeth at one time.
The use of loupes improves ergonomics and reduces the risk of MSDs.6,9,21,22 Additionally, the greatest advantage of loupes are enhanced indirect vision, improved vision for instrumentation, and reduction of visual deficiencies among clinicians older than 40.2,6,7 Other advantages include improved ability to read the periodontal probe, assess soft tissues, and detect calculus. The combination of loupes and lights enhances dental hygiene assessments and improves quality of care by illuminating the oral cavity.23,24 The literature, however, is limited on the impact of loupes on treatment outcomes.9
Loupes, when properly fitted, should be considered a foundational component to musculoskeletal health. Dental hygienists have reported less pain in their shoulders, arms, and hands after using loupes for only 6 months.8 Thus, introducing loupes early into dental hygiene education may reduce visual deficiencies, thus decreasing the risk of MSDs. Enhancing magnification with improved illumination from a head light improves visual acuity and supports balance.
Disadvantages of Loupes and Lights on Ergonomic Practice and Musculoskeletal Health
The use of loupes and lights is not without disadvantages. While wearing loupes, a dental hygienist’s sensorimotor may be altered due to the eyes shifting from magnified to nonmagnified fields, making it challenging to maintain balance and a neutral neck position. The early changes in magnification fields may cause vertigo and eye soreness. Dental hygienists should know that the adjustment period for wearing loupes is usually 2 weeks to 3 weeks.25–27
Illumination from a head light improves visual acuity and supports balance.
Both the Galilean and Keplarian loupe lenses can be mounted onto the front of the frame as a “flip up” or entrenched into the spectacle lens itself, which is known as a through-the-lens (TTL) loupe. For dental hygienists with prescription glasses, the flip-up loupe is best because the prescription lenses can easily be placed in and out as needed. The flip-up loupe, however, is heavier than the TTL loupe. Although the fixed TTL loupe is lighter, it is also more expensive, and dental hygienists do not have the ability to easily switch between magnified and direct vision.
The weight and cost of loupes and lights are also potential barriers. Loupes cost between $600 and $1,200 and lights range between $300 and $600.6 In regards to ergonomic health, the additional weight poses risks as well. Keplarian telescope systems provide a higher magnification, but are heavier and more expensive than Galilean loupes. In addition, LED headlamps add weight. Most LED headlamps require an attached battery pack that powers the light, which may cause cross-contamination risks. At certain intensities, the LED illumination may also harm the retina. It is important to verify that a headlight’s LED beam has white or colorless beams.28
The type of loupe and light purchased depends on the user’s individual needs. Loupes must be properly adjusted to conform to the dental hygienist’s facial features. Even the smallest fitting error can cause eyestrain.29 In addition, headlight systems greatly vary between manufacturers. Most loupe manufacturers make both cordless and corded batteries. Lights with corded batteries are often lighter on the frame.
As light intensities can vary, dental hygienists need to inquire about illumination products that will be both safe and comfortable. Dental hygienists should educate themselves on loupe and light brands and seek professional assistance for customized fitting before making a purchase. Other factors to consider when purchasing loupes are cost of accessories and replacement parts, as well as ease of maintenance and after-sales care.
Summary
Dental hygienists wishing to extend their careers will need to maintain ergonomic health. Visual acuity is necessary to perform clinical care and sustain proper ergonomics. Dental hygienists need to be aware of visual deficiencies and the natural process of declining vision with age. Considering the effect of visual acuity on clinical care and ergonomics, practicing dental hygienists should have their near vision evaluated regularly. The addition of loupes and lights may compensate for visual deficiencies and improve ergonomics, allowing dental hygienists to enhance patient care and maintain the longevity of a clinical career.
References
- American Optometric Association. Visual Acuity: What is /0/20 vision? Available at: aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/visual-acuity. Accessed July 12, 2021.
- Hoerler SB, Branson BG, High AM, Mitchell TV. Effects of dental magnification lenses on indirect vision: a pilot studyJ J Dent Hyg. 2012;86:323–330.
- Hayes MJ, Taylor JA, Smith DR. Predictors of work- related musculoskeletal disorders among dental hygienists. Int J Dent Hyg. 2012;10:265–269.
- Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders in a 3 year longitudinal cohort of dental hygiene students. J Dent Hyg. 2014;88:36–41.
- Bly J. Ergonomics and visual acuity. Dimensions of Dental Hygiene. 2018;16(10):26–28.
- Arnett MC, Gwozdek AE, Ahmed S, Beaubien HD, Yaw KB, Eagle IT. Assessing the use of loupes and lights in dental hygiene educational programs. J Dent Hyg. 2017;91:15–20.
- Perrin P, Ramseyer ST, Eichenberger M, Lussi A. Visual acuity of dentists in their respective clinical conditions. Clin Oral Investig. 2014;18:2055–2058.
- Hayes MJ, Osmotherly PG, Taylor JA, Smith DR, Ho A. The effect of wearing loupes on upper extremity musculoskeletal disorders among dental hygienists. Int J Dent Hyg. 2014;12:174–179.
- Eichenberger M, Perrin P, Sieber KR, Lussi A. Near visual acuity of dental hygienists with and without magnification. Int J Dent Hyg. 2018;16:357–361.
- Branson BG, Black MA, Simmer-Beck M. Changes in posture: a case study of a dental hygienist’s use of magnification loupes. Work. 2010;35:467–476.
- 11. Gehrig JS, Sroda R, Saccuzzo D. Ergonomics and periodontal instrumentation. In: Fundamentals of Periodontal Instrumentation and Advance Root Instrumentation. 8th ed. Philadelphia: Wolters Kluwer; 2017:1–38.
- Kapandji AI. The Physiology of the Joints: the Spinal Column, Pelvic Girdle and Head. 7th ed. Pencaitland, Scotland: Handspring Publishing Ltd; 2019:1–359.
- 13. Dylla JM, Forrest JL. Practice in motion: Part 1. Available at: dentalcare.com/en-us/professional-education/ce-courses/ce553. Accessed July 12, 2021.
- Eichenberger M, Biner N, Amato M, Lussi A, Perrin P. Effect of magnification on the precision of tooth preparation in dentistry. Oper Dent. 2018;43:501–507.
- Kellogg Eye Center. Refractive Errors. Available at: umkelloggeye.org/conditions-treatments/refractive-errors. Accessed July 12, 2021.
- Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic Physiol Opt. 2011;31:502–515.
- Hart RG, Hall J. The value of loupe magnification:an underused tool in emergency medicine. Am J Emerg Med. 2007;25:704–707.
- Buller AJ, Ramchndani M, Fenerty C. Better optic disc examination: wearing loupes enhances the indirect opthalmoscope image. J Pediatr Opthalmol Strabmisus. 2006;43:102–103.
- Maggio MP, Villegas H, Blatz MB. The effect of magnification loupes on the performance of preclinical dental students. Quintessence Int. 2011;42:45–55.
- Turcotte C. How do I know when it’s time to upgrade my loupes? Dimensions of Dental Hygiene. 2021;19(4):46.
- Congdon LM, Tolle SL, Darby M. Magnification loupes in US entry-level dental hygiene programs occupational health and safety. J Dent Hyg. 2012;86:215–222.
- Khan SA, Chew KY. Effect of working characteristics and taught ergonomics on the prevalence of musculoskeletal disorders amongst dental students. BMC Musculoskelet Disord. 2013;14:118.
- Holt ER, Hoebeke R. Shine a light. Dimensions of Dental Hygiene. 2012;10(9):25–27.
- Brame JL. Seating, positioning, and lighting keep your body injury-free with these cornerstones of ergonomics. Dimensions of Dental Hygiene. 2008;6(9):36–37.
- Hayes MJ, Osmotherly PG, Taylor JA, Smith DR, Ho A. The effect of loupes on neck pain and disability among dental hygienists. Work. 2016;53:755–762.
- Sunell S, Rucker L. Surgical magnification in dental hygiene practice. Int J Dent Hyg. 2004;2:26–35.
- Branson BG, Bray KK, Gadbury-Amyot C, et al. Effect of magnification lenses on student operator posture. J Dent Educ. 2004;68:384–389.
- Stamatacos C, Harrison JL. The possible ocular hazards of LED dental illumination applications. J Tenn Dent Assoc. 2013;93:25–29.
- Shanelec DA. Optical principles of loupes. J Calif Dent Assoc. 1992;20:25–32.
From Dimensions of Dental Hygiene. August 2021;19(8):21-23.

