
Human Papillomavirus-Induced Head and Neck Lesions
Oral health professionals should be well-versed in the mode of transmission, risk factors associated with infection, and treatment modalities.
This course was published in the April 2022 issue and expires April 2025. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe the clinical features of the human papillomavirus (HPV)-induced lesions that occur in the head and neck.
- Discuss the risks of transmission for HPV.
- Define the modes of transmission for HPV.
- Identify two preventive measures that can be used to drive down HPV infection rates.
The human papillomavirus (HPV) encompasses a large group of related viruses that can infect human skin and mucosa.1,2 The lesions that occur in mucosa can arise in the anogenital region and upper aerodigestive tract.1 According to the United States Centers for Disease Control and Prevention (CDC), more than140 types of HPV exist, with approximately 40 types affecting the oral cavity.3 Virus types are classified as low risk or high risk depending on their potential to develop into benign, premalignant, or malignant lesions.2 Low-risk types may cause no disease or benign growths such as squamous papilloma, verruca vulgaris, genital warts, or various sinonasal papillomas. High-risk types of HPV are more likely to increase an individual’s risk of developing a carcinoma.2 Infection with HPV is recognized as a causal factor in the development of carcinoma in the anogenital region, including the uterine cervix, anus, vagina, vulva, and penis.3 In the head and neck, HPV is associated with the high-risk variants responsible for oropharyngeal squamous cell carcinoma.4
Benign Lesions
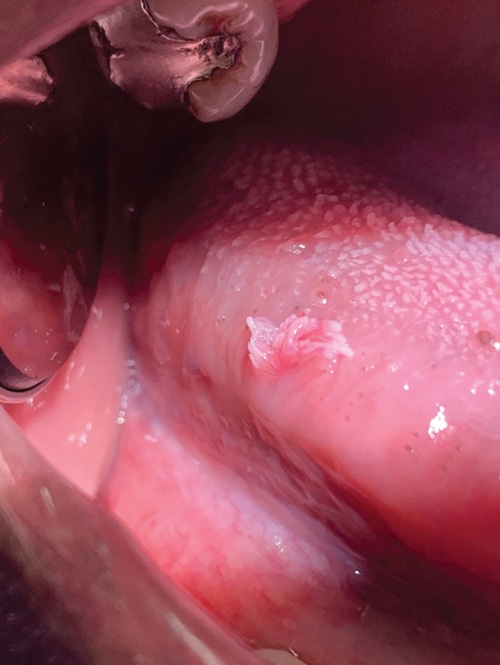
Squamous Papilloma. This benign, exophytic (growing outward from the surface) lesion presents with a papillary or fingerlike surface architecture and color ranging from pink to white (Figure 1). It can occur at any location in the oral cavity but is frequently found as a solitary lesion on the tongue, palate, or lips.1,5 The lesion is usually pedunculated (attached via a stalk) but can be sessile (attached directly by the base). It can occur at any age but the average age is between 30 and 50.6 Squamous papilloma is most often associated with low-risk HPV types 6 and 11 (Table 1).6,7 Diagnosis is made by biopsy and histologic examination. The treatment of choice for squamous papilloma is surgical excision using laser technology. Other treatments include electrocautery, cryosurgery, and intralesional injections of interferon.6 Recurrence is rare, except for lesions in patients infected with human immunodeficiency virus.8
Verruca Vulgaris. This common wart is primarily found on the skin of the hands. Its clinical presentation is similar to a papilloma with an exophytic papillary appearance (Figure 2). The lesions are sessile and can appear pink to white. While rarely found on the mucosa, it can be transferred to the vermillion border, gingiva, or anterior tongue through autoinoculation from the hands.1,5,9 The virus affects children and young adults with a peak incidence in teenagers ages 12 to 16.7 Verruca vulgaris is most frequently associated with HPV low-risk types 2 and 4 (Table 1).7 Diagnosis is made by biopsy and histologic examination. The treatment for verruca vulgaris is topical salicylic acid or liquid nitrogen.1 For lesions that occur intraorally, the treatment is surgical excision. Other treatments include removal using lasers, cryotherapy, or electrosurgery.
Condyloma Acuminatum. This venereal wart primarily occurs in the anogenital region. It is the most commonly reported sexually transmitted infection in the US7 and presents in approximately 1% of sexually active individuals.1 Condyloma acuminatum presents as exophytic, pink nodules with short blunt surface projections (Figure 3). Common oral locations include the labial mucosa, lingual frenum, and soft palate.1,7 While uncommon in the oral cavity, the lesion can be transferred to the mouth through orogenital contact or self-inoculation.5 These lesions are more commonly seen in adults ages 30 to 40.7 HPV low-risk types 6 and 11 contribute to 90% of condyloma acuminatum cases.1 Many patients are coinfected with HPV high-risk types 16 and 18 (Table 1). Diagnosis is made by biopsy and histologic examination. Treatment is surgical excision.
Heck Disease. Also called multifocal epithelial hyperplasia, Heck disease is a benign condition that presents as solitary nodular lesions or multiple whitish to pale pink masses occurring primarily on the buccal and labial mucosa and the tongue (Figure 4).1,7,10 The lesions can present as smooth surface nodules or exhibit a pebbly surface texture.1 Genetics is believed to play a role in the development of this condition, as many with the infection test positive for the human lymphocytic antigen: DR4.7,11 Multifocal epithelial hyperplasia can occur at any age but presents most commonly in children and young adolescents.1,10 Heck disease is associated with HPV low- risk types 13 and 32 (Table 1).7,11 These lesions are asymptomatic and rarely require treatment as they have been reported to regress.1,5 Surgical excision is the treatment modality for longstanding lesions.
Sinonasal Papillomas. These benign growths arise from the sinus and nasal mucosa. They can develop in various locations, including the nasal septum, lateral walls of the nasal cavity, and maxillary and ethmoid sinuses. Sinonasal papillomas compose 10% to 25% of all tumors arising in this region.1 Their etiology is not well understood but a history of allergies, sinusitis, and nasal polyps has been suggested.1 Infection with HPV is also a possibility. Syrjänen and Syrjänen12 reported approximately 39% of sinonasal papillomas studied were positive for HPV. Based on clinical and histological features, papillomas are classified as fungiform, inverted, or cylindrical. 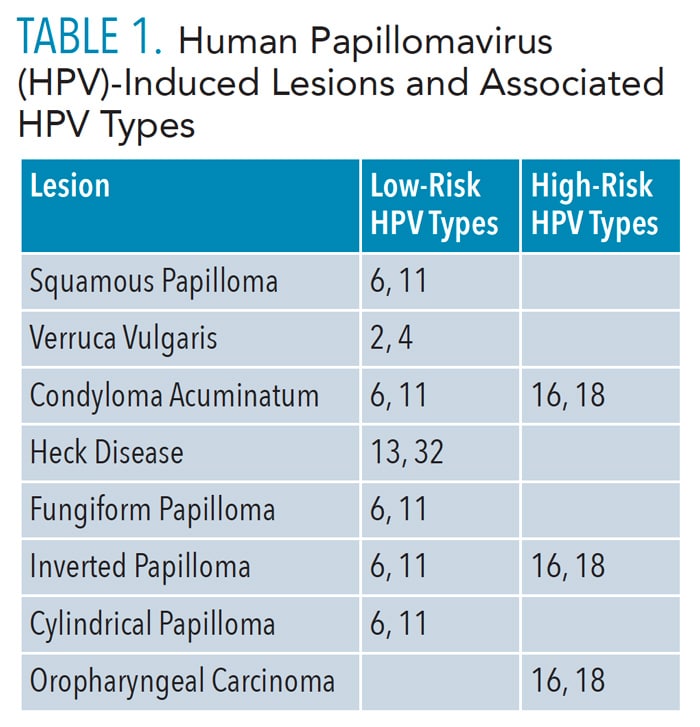
The fungiform papilloma presents as a pinkish nodule with a papillary surface architecture similar to the squamous papilloma. It arises on the nasal septum and occurs more often in men than women. The most common presenting symptom is nasal obstruction or bleeding.1 Most cases test positive for HPV 6 or 11 (Table 1). Treatment involves surgical excision.
The inverted papilloma is the most common and presents with significant clinical behavior as it can be locally destructive extending to surrounding structures. Three percent to 24% of cases transform into a malignancy.1 Similar to the fungiform papilloma, the inverted papilloma presents as a pink nodule but arises on the lateral nasal walls. Occurring more often in men, inverted papilloma may cause nasal obstruction with bleeding, headaches, and hinder the ability to smell. The most prevalent HPV types identified are HPV 6, 11, 16, and 18 (Table 1). The treatment of choice is transnasal endoscopic surgery but may be combined with an external surgical approach in aggressive cases.1
The cylindrical papilloma is the least common and presents as a red or brown nodule with a pebbly surface texture. It arises on the lateral nasal walls, ethmoid, or maxillary sinuses. Nasal obstruction is the most common presenting symptom. The prevalence of HPV is low in cylindrical papilloma with types 6 and 11 being the ones detected (Table 1). Treatment involves transnasal endoscopic surgery or an external surgical approach.1

Malignant Lesions
Oropharyngeal Squamous Cell Carcinoma. This subset of squamous cell carcinoma occurs in the head and neck. It has a predilection for the pharyngeal walls, soft palate, base of tongue, and tonsillar region. Approximately 70% to 80% of cases occur in the tonsillar region.1 This location makes diagnosis more challenging. A definitive diagnosis is often delayed until symptoms develop with advanced disease. Symptoms include a prolonged sore throat, dysphagia, and pain upon swallowing.1 Due to the delay in diagnosis, lesions are commonly greater in size than carcinomas that present in the oral cavity; they are more likely to have metastasized.1
The primary causes for most cancers in the head and neck are smoking and alcohol use.13 Over the past two decades, the incidence of oropharyngeal squamous cell carcinoma has been increasing, particularly in men. This increase is associated with HPV and sexual behavior. Approximately 72% of oropharyngeal carcinomas are caused by HPV, with 62% induced by the high-risk types, HPV 16 and HPV 18.4 HPV type 16 has been identified in more than 90% of oropharyngeal squamous cell carcinoma cases.13 The prevalence of non-HPV-associated cases has been decreasing, and smoking and alcohol are more significant compared with HPV-associated cases (Table 2).14,15
In early cases, the treatment of oropharyngeal squamous cell carcinoma involves surgery or radiation therapy. For advanced disease, a combination of surgery, radiation, and chemotherapy is used. Determination of active HPV infection is imperative as HPV-positive oropharyngeal squamous cell carcinoma has a better prognosis than non-HPV oropharyngeal squamous cell carcinoma.1,14,15

Diagnosis
HPV-induced lesions are diagnosed by biopsy and microscopic evaluation. Oral lesions identified on examination should be referred to a dentist, oral pathologist, or oral surgeon for evaluation and biopsy. Benign lesions do not generally recur, however, follow-up at subsequent visits is recommended. Cases of oral pharyngeal squamous cell carcinoma require a multidisciplinary approach to include the expertise of otolaryngologists, head and neck surgeons, and oncologists.
Discussion
HPV is transmitted via skin or mucosal contact. The ease of infectivity is attributed to the affinity of the virus for human skin and mucosa. HPV invades the most superficial layers of the epithelium, making it more likely to evade the body’s immune surveillance system. On contact, microtrauma occurs to the epithelium, allowing the virus to easily enter and infect epithelial cells.16
The virus can be transmitted sexually and nonsexually through skin-to-skin, skin-to-mucosa, or mucosa-to-mucosa contact with an infected person. Horizontal transmission occurs via contact with mucosa, skin, fingers, mouth, and objects. The virus has been reported to live on surfaces for several days.7,16 Vertical transmission occurs between a mother and child either during pregnancy through the placenta or during natural delivery by contact with genital mucosa.16,17
Self-inoculation is another mode of transmission. Patients can transmit the virus from one part of the body to another. This is particularly true with young children. When lesions present in children, the mode of transmission warrants investigation by a healthcare provider. Auto inoculation from skin warts to genital areas can occur. However, the presence of anogenital type warts in children should prompt further evaluation to rule out sexual abuse.18

According to the CDC, approximately 14 million people, including teens, become infected with HPV each year.3 The risk for infection is high with 80% of women and 90% of men becoming infected with at least one type of HPV during their lifetimes.16 Most people are asymptomatic when infected and will clear the virus within 1 year to 2 years without any sequela.1–3 In a certain percentage of people, the virus will persist and, depending on the type, can lead to benign and/or malignant lesions.12 An impaired immune system, older age, and sexual behavior are linked with persistent infections.1
Lesions can develop with any of the HPV types; however, the risk of oral pharyngeal squamous cell carcinoma is the most significant concern. Even though the prevalence for HPV-induced oropharyngeal carcinoma has increased over the past 20 years, the risk remains low. The overall prevalence of HPV in the oral cavity is approximately 6.9%.5 A 5-year study conducted by Souza et al13 revealed that the incidence of HPV oral infections was 6% for men and 1% for women across all age groups. The prevalence for men ages 50 to 59 was slightly higher at 8%. The prevalence was lower for oral HPV 16. Engaging in oral sex with an increased number of partners also showed a connection with higher infections in men compared to women.13 HPV infection is the leading cause of sexually transmitted diseases in the US.2–4 Factors that increase infection risk include multiple sex partners, unprotected sex, adolescent start of sexual activity, and oral sex. In the US, more than 85% of sexually active adults ages 18 to 44 reported having had oral sex at least once with a partner of the opposite sex.3 Smoking is another risk factor due to its systemic and immunosuppressive effects. The prevalence of HPV 16 is higher among tobacco users.15 D’Souza et al13 reported that smoking doubled the prevalence of HPV infections in men (Table 3).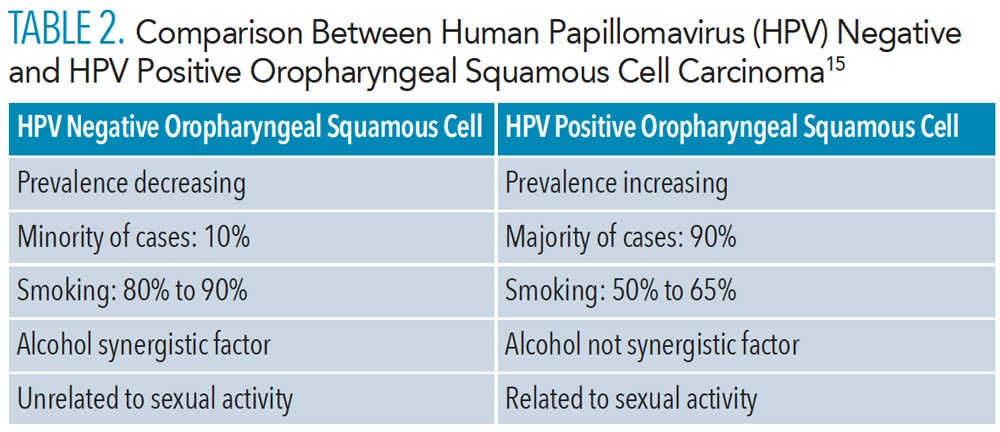
Currently, treatment is not available for HPV infections. The most effective mitigation strategy is to decrease infection rates via prevention. Sexual activity is the most significant causative factor. Participating in low-risk sexual activities, such as those that do not involve the exchange of body fluids or direct contact between mucus membranes with another person, is an effective way to avoid infection.19 Other preventive strategies include monitoring health status (eg, undergoing regular Pap tests and pelvic exams for women and being regularly tested for HPV). Limiting sexual activity to a monogamous relationship significantly diminishes exposure to infection.20 Another way to mitigate risk is to use condoms and other barriers, such as dams, when engaging in sexual activity.19
Another highly effective preventive strategy to not only reduce HPV transmission but also to prevent cancers is vaccination. Most HPV vaccines protect against the viral strains frequently associated with cancer (HPV types 16 and 18) and genital warts (HPV types 6 and 11). Currently, the only vaccine distributed in the US is Gardasil 9, a nine valent one that protects against HPV types 6, 11, 16,18, 31, 33, 45, 52, and 58.3 The CDC reports that since HPV vaccination was first recommended in 2006, there has been a significant reduction in HPV infections, but the number of preventable cancer cases remains high. The CDC calculates the number of HPV-associated cancers (a specific type of cancer that is diagnosed in a part of the body where HPV is often found including the cervix, vagina, vulva, penis, anus, and oropharynx) to estimate the percentage of HPV-attributable cases (cases where the cancer is probably caused by HPV). HPV-attributable cases are estimated by multiplying the number of HPV-associated cases by the percentage attributable to HPV based on genotype studies.21 Based on data from 2014 to 2018, the CDC estimates 79% of these cancer cases were attributable to HPV each year. Out of those cases, approximately 92% could have been prevented by the 9 valent HPV vaccine.21 Vaccination has proven most effective if administered prior to exposure to the virus.4,12 The CDC recommends vaccination for children at ages 11 to 12 but advises the vaccine can be administered as early as age 9. Vaccination is also recommended for individuals up to age 26 if they were not vaccinated at a younger age. Routine vaccination is not recommended for adults older than age 26. For individuals ages 27 to 45, vaccination should be based on risk, and determined by medical guidance from a physician.
As healthcare providers, dentists and dental hygienists play an integral role in disease prevention and patient education not only in clinical practice as part of the oral cancer examination but in community outreach events. They are well positioned to educate patients on strategies to mitigate risks of infection but also to advocate for the benefits of HPV vaccination. 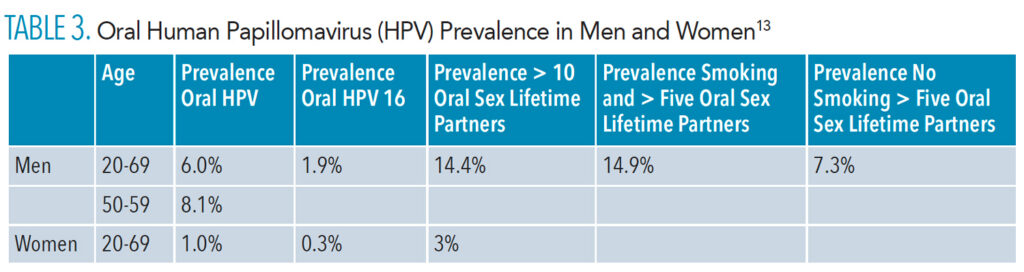
Conclusion
HPV infections are common and can lead to both benign and malignant lesions. Although some of the lesions possess shared viral subtypes, they differ in clinical presentation and prognosis. To adequately diagnose and treat, the clinician needs to be familiar with the various clinical presentations and demographics. Due to the possible sexual transmissibility of some of these lesions, patient education is critically important to prevent an increase in infection rates. Although vaccinations have proven effective in driving down infection rates, patients need to be educated on the value of vaccination in addition to awareness of the relationship between HPV and behaviors such as smoking and sexual activity.
References
- Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology. 4th ed. St. Louis: Saunders Elsevier; 2016:331–340, 378–372.
- National Cancer Institute. HPV and Cancer. Available at: cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-and-cancer. Accessed March 23, 2022.
- United States Centers for Disease Control and Prevention. HPV, the Vaccine for HPV, and Cancers Caused by HPV. Available at: cdc.gov/hpv/index.html. Accessed March 23, 2022.
- Vázquez-Otero C, Vamos CA, Thompson EL, et al. Assessing dentists’ human papillomavirus-related health literacy for oropharyngeal cancer prevention. J Am Dent Assoc. 2018;149:9–17.
- Ibsen OA, Phelan JA. Oral Pathology for the Dental Hygienist. 7th ed. St. Louis: Saunders Elsevier; 2014:125–126.
- Babaji P, Singh V, Chaurasia VR, Masamatti VS, Sharma AM. Squamous papilloma of the hard palate. Indian J Dent. 2014;5:211–213.
- Betz SJ. HPV-related papillary lesions of the oral mucosa: a review. Head and Neck Pathol. 2019;13:80–90.
- Jaju PP, Suvarna PV, Desai RS. Squamous papilloma: case report and review of literature. Int J Oral Sci. 2010;2:222–225.
- Ural A, Arslan S, Ersoz Ş, Değer B. Verruca vulgaris of the tongue: a case report with a literature review. Bosn J Basic Med Sci. 2014;14:136–138.
- Regezi JA, Sciubba JI, Jordan RC. Oral Pathology Clinical Pathologic Correlations. 7th ed. St. Louis: Saunders Elsevier; 2017:148–152.
- Bennett LK, Hinshaw M. Heck’s disease: diagnosis and susceptibility. Pediatr Dermatol. 2009;26:87–89.
- Syrjänen K, Syrjänen S. Detection of human papillomavirus in sinonasal papillomas: systematic review and meta-analysis. Laryngoscope. 2013;123:181–192.
- D’Souza G, McNeel TS, Fakhry C. Understanding personal risk of oropharyngeal cancer: risk-groups for oncogenic oral HPV infection and oropharyngeal cancer. Ann Oncol. 2017;28:3065–3069.
- Rettig EM, D’Souza G. Epidemiology of head and neck cancer. Surg Oncol Clin N Am. 2015;24:379–396.
- Kalmar J. Oral and Tonsillar Cancer: What About HPV? Lecture presented at: Thomas P. Hinman Dental Meeting; March 31, 2019; Atlanta.
- Petca A, Borislavschi A, Zvanca ME, Petca RC, Sandru F, Dumitrascu MC. Non-sexual HPV transmission and role of vaccination for a better future (Review). Exp Ther Med. 2020;20:186.
- Syrjanen S, Puranen M. Human papillomavirus infections in children: the potential role of maternal transmission. Crit Rev Oral Biol Med. 2000;11:259–274.
- Cao CD, Merjanian L, Pierre J, Balica A. A discussion of high-risk hpv in a 6-year-old female survivor of child sexual abuse. Case Rep Obstet Gynecol. 2017;2017:6014026.
- John Hopkins Medicine. Safer Sex Guidelines. Available at: hopkinsmedicine.org/health/wellness-and-prevention/safer-sex-guidelines. Accessed March 23, 2022.
- Stanley M. Prevention strategies against the human papillomavirus: the effectiveness of vaccination. Gynecol Oncol. 2007;107(2 Suppl 1):S19–S23.
- United States Centers for Disease Control and Prevention. Cancers Associated With Human Papillomavirus, United States—2014–2018. Available at: cdc.gov/cancer/uscs/about/data-briefs/no26-hpv-assoc-cancers-UnitedStates-2014-2018.htm. Accessed March 23, 2022.`
From Dimensions of Dental Hygiene. April 2022;20(4):42-45.



