How to Care for Patients With Diabetes
Dental hygienists play an important role in providing effective oral health care to patients with diabetes, and in recognizing the symptoms of undiagnosed diabetes.
This course was published in the January 2013 issue and expires January 2016. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
1. Define type 1 and type 2 diabetes.
2. Discuss the association between diabetes and periodontal diseases.
3. Explain strategies for providing effective dental treatment to patients with diabetes.
4. Identify the signs of undiagnosed diabetes.
More than 25.8 million people in the United States have diabetes.1 This metabolic disorder is associated with many health complications that result from microvascular and macrovascular diseases. Periodontal disease is now considered the sixth complication of diabetes, following retinopathy, nephropathy, neuropathy, macrovascular disease, and poor wound healing. As such, people with diabetes must receive regular, preventive dental hygiene care and dental professionals need to be well versed in how to provide the highest level of care to this patient population. Clinicians should also be familiar with the signs and symptoms of diabetes, so they can refer patients who may have undiagnosed diabetes to their physicians.
DIABETES DEFINED
Patients with diabetes experience either impaired action of insulin or altered secretion of insulin that results in hyperglycemia.2 Of the 25.8 million people in the United States with diabetes, the federal Centers for Disease Control and Prevention (CDC) estimates 7 million remain undiagnosed.1 Diabetes is a leading cause of death, in addition to creating significant health problems, including cardiovascular disease, stroke, hypertension, retinopathy, renal disease, neuropathy, dental disease, amputations, and pregnancy complications.1
Type 1 diabetes is characterized by absolute insulin deficiency. The most common cause is the autoimmune destruction of pancreatic beta cells. Any loss of pancreatic tissue, however, can result in insulin deficiency. Patients with type 1 diabetes require insulin for glycemic control.2 The development of type 1 diabetes is strongly linked to genetics, and is usually diagnosed before the end of adolescence.2
Type 2 diabetes is caused by insulin resistance in which the target tissues do not respond appropriately to normal levels of circulating insulin. These target tissues then require increased levels of insulin for an adequate response.2 Although more common in adults, an increasing number of children are being diagnosed with type 2 diabetes due to the nationwide increase in childhood obesity. Type 2 diabetes has an even stronger genetic predisposition than type 1. In fact, 40% of patients with type 2 diabetes have at least one parent with the disease.2 Some individuals with type 2 diabetes may control their glucose levels with lifestyle modifications, such as nutritional changes, exercise, and weight loss. Others may require oral hypoglycemic agents or insulin.2
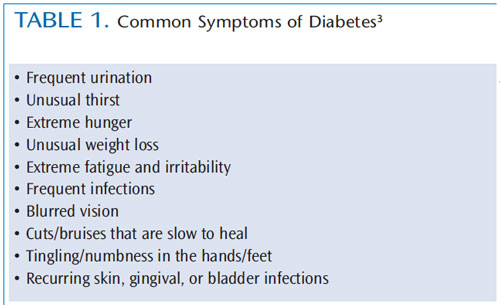
Table 1 provides a list of the most common symptoms of diabetes.3 All medical history forms in dental offices should ask questions related to these signs and symptoms so patients can be screened for diabetes. Prediabetes is diagnosed when fasting plasma glucose levels are equal to or greater than 100 mg/dl or when impaired glucose tolerance occurs, but the diagnostic threshold of type 2 diabetes (126 mg/dl or greater) has not been reached.2 People who are diagnosed at the prediabetes stage have the opportunity to make lifestyle modifications that can significantly delay, if not prevent, the development of type 2 diabetes.2
PERIODONTAL HEALTH
Research demonstrates an association between diabetes and periodontal diseases.4 The CDC reports that adults age 45 years and older with poorly controlled diabetes (defined as HbA1c > 9%) were 2.9 times more likely to experience severe periodontitis than adults without diabetes.1 Glycemic control is an important factor in this association, with a higher prevalence and severity of gingival inflammation and periodontal destruction found among people with diabetes who have poor glycemic control.5 Individuals with well-controlled diabetes do not have a significantly higher risk of periodontal destruction.5 Research suggests that the association between periodontal disease and type 2 diabetes is much stronger than for type 1 diabetes.6
The association between the two diseases may be due to the advanced glycation end products (AGEs) that result from hyperglycemia.4 These AGEs can bind to receptors and transform macrophages into cells that are more destructive with the release of higher levels of interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor-? (TNF-?). These cytokines play an important role in the initiation and progression of periodontal diseases.4,7–9 The formation of AGEs also leads to increased collagen accumulation in the periodontal tissues, which can cause thickening of the vessel walls and decreased tissue perfusion and oxygenation. This may be why patients with diabetes are more prone to periodontal infection and impaired healing.4
The relationship between periodontal diseases and diabetes is bidirectional, meaning that periodontal diseases also contribute to poor metabolic control of diabetes.10 The presence of TNF-? leads to increased insulin resistance, and some studies have shown that treatment of periodontal diseases may lead to improved metabolic control, while others have found no statistically significant difference.4,11 A review was conducted of studies that examined the effect of periodontal therapy on glycemic control among patients with diabetes.11 The researchers concluded there is some evidence that periodontal therapy may have a modestly favorable effect on glycemic control in patients with diabetes.11 However, they noted that the available data are limited and further research is needed.
TREATMENT
Because patients with diabetes are at increased risk of periodontal diseases, they need to receive periodontal therapy and preventive dental hygiene care on a frequent recare schedule—ideally every 3 months. Dental professionals should obtain information about the patient’s disease status, medications, and be prepared for the possibility of a hypoglycemic emergency. A thorough medical history should be obtained and reviewed for every patient. Medical consultation may be required if the patient presents with uncontrolled diabetes or unexplained positive responses to questions.12 Table 2 provides a list of the information that should be garnered from patients with diabetes before beginning treatment.12 If patients are unable to provide complete information, a consultation with their physician is recommended before dental treatment is provided.
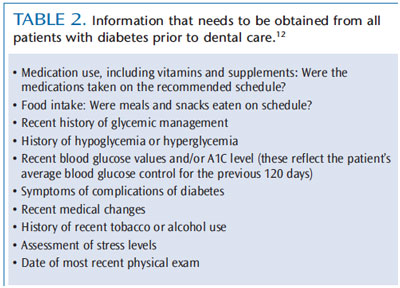
Dental patients with diabetes should be questioned about their blood glucose levels on the day of the appointment, as well as their A1C levels. Preprandial glucose levels (before a meal) should be 70 mg/dl to 110 mg/dl, and post-prandial glucose levels (after a meal) should be less than 180 mg/dl.13 Individual patients may have more or less stringent goals as determined by their physician.
Before the dental hygiene appointment, record the most recent A1C level. Patients with diabetes should have their A1C, which measures the percent of glycated hemoglobin (HbA1c) in the blood, checked at least twice per year.14 The A1C reflects the patient’s average blood glucose control for the previous 120 days, providing an overall picture of how well the patient’s diabetes treatment plan is controlling his or her blood sugar.14 This test measures how much glucose is glycated with hemoglobin on red blood cells (RBC). RBCs have a lifespan of about 120 days, therefore, glycation values change with RBC turnover.14 For most patients with diabetes, the A1C should be less than 7%; if the A1C is higher, dental treatment should be postponed and a physician should be consulted.14,15 For every 1% increase in A1C level, there is an increase in complication rates for microvascular and macrovascular disease, as well as the risk of poor wound healing and post-operative problems.2 If the patient does not know his or her A1C, then the most recent blood glucose values should be recorded.
Although patients with well-controlled diabetes do not require antibiotic premedication prior to dental treatment, those with uncontrolled diabetes require physician consultation to determine whether there is a need.12 Patients with diabetes should be scheduled soon after they have eaten breakfast and taken their medications. After lunch is also a possibility. Patients with diabetes should always be asked when they last ate.12 Appointments should be scheduled so they do not interfere with the patient’s regular meal times, and long stressful appointments should be divided into multiple, shorter appointments.12
There are no specific guidelines regarding hyperglycemia and how it should be managed before and during a dental procedure. It is safe to provide dental treatment as long as blood glucose values are not elevated to the point where a patient’s ability to think clearly or concentrate is altered.2
HYPOGLYCEMIA
The most common medical emergency experienced by dental patients with diabetes is hypoglycemia. Dental professionals need to be able to recognize the signs of hypoglycemia, which include confusion, dizziness, shakiness, hunger, headache, irritability, racing pulse, pale skin, sweating, trembling, weakness, and anxiety.2 Patients exhibiting symptoms of hypoglycemia should immediately consume 15 g of carbohydrates, such as glucose tablets or gels, fruit juice, milk, soft drink, honey, corn syrup, or table sugar.2 Dental team members should have a plan for treating hypoglycemia in patients who are conscious and unconscious.2
Patients who use insulin are at the highest risk of developing hypoglycemia. Patients taking oral diabetic medications are also at risk, especially if they also have renal or hepatic disease.2 Glucose testing can be used in the dental office to confirm that a patient’s blood glucose level is safe prior to treatment.12
RECOGNIZING SYMPTOMS OF UNDIAGNOSED DIABETES
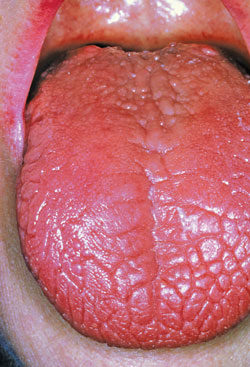
Diabetes does exert oral manifestations that dental professionals may recognize before the patient is diagnosed. These include: dry mouth (Figure 1), periodontal diseases, oral candidiasis (Figure 2), burning mouth syndrome, impaired wound healing, recurrent oral infections, and acetone breath, which smells fruity and is indicative of diabetic ketoacidosis.16 Approximately 60% of Americans visit a dental office each year, which makes it an opportunistic site for screening patients with undiagnosed diabetes.16 Early diagnosis and treatment can reduce the life-threatening complications of diabetes and improve quality of life.12

Dental professionals also need to educate their patients about the oral effects of diabetes. One study found that only 33% of participants with diabetes were aware of their elevated risk for periodontal diseases.17 Many patients with diabetes are not familiar with the association between poor oral health and systemic health. The development of closer partnerships between dental and medical professionals can help improve patient care.17
CONCLUSION
Patients with diabetes are at increased risk of periodontal diseases, thus, dental professionals should be familiar with the disease and how to treat patients with diabetes safely in the dental office. Dental hygienists are in a unique position to recognize the signs and symptoms of undiagnosed diabetes, which can result in earlier diagnosis and referral to a physician. Dental hygienists have an important role to play in improving interprofessional disease management.
ACKNOWLEDGEMENTS / PHOTOGRAPHY
LAGUNA DESIGN / SCIENCE PHOTO LIBRARY
JAMES STEVENSON/SCIENCE PHOTO LIBRARY
DR P. MARAZZI/SCIENCE PHOTO LIBRARY
REFERENCES
-
- Centers for Disease Control and Prevention.2011 National diabetes fact sheet. Available at:www.cdc.gov/diabetes/pubs/estimates11.htm#1. Accessed December 6, 2012.
- Kidambi S, Patel SB. Diabetes mellitus:Considerations for dentistry. J Am Dent Assoc.2008;139:8S–18S.
- American Diabetes Association. Diabetes basics: Symptoms. Available at:www.diabetes.org/diabetesbasics/symptoms/?loc=DropDownDB-symptoms. Accessed December 6, 2012.
- Acharya AB, Satyanarayan A, Thakur SL. Status of association studies linking diabetes mellitus and periodontal disease in India. Int J DiabetesDev Ctries. 2010;30:69–74.
- Roy S, Trudeau K, Roy S, Behl Y, Dhar S,Chronopoulos A. New insights into hyperglycemia-induced molecular changes in microvascular cells. J Dent Res. 2010;89:116–127.
- Chavarry NGM, Vettore MV, Sansone C,Sheiham A. The relationship between diabetes mellitus and destructive periodontal disease: a meta-analysis. Oral Health Prev Dent.2009;7:107–127.
- Nield-Gehrig J, Willmann D. Foundations of periodontics for the dental hygienist. 2nd ed.Baltimore, Md: Lippincott Williams and Wilkins;2008.
- Kaur G, Holtfreter B, Rathmann W, et al.Association between type 1 and type 2 diabetes with periodontal disease and tooth loss. J Clin Periodontol. 2009;36:765–774.
- Gomes MAB, Rodrigues FH, Afonso-Cardoso SR,et al. Levels of immunoglobulin A1 and messenger RNA for interferon and tumor necrosis factor in total saliva from patients with diabetes mellitus type 2 with chronic periodontal disease. J Periodontal Res. 2006;41:177–183.
- Cullinan MP, Ford PJ, Seymour GJ. Periodontaldisease and systemic health: Current status. AustDent J. 2009;54(Suppl):62–69.
- Simpson TC, Needleman I, Wild SH, Moles DR,Mills EJ. Treatment of periodontal disease for glycemic control in people with diabetes. Cochrane Database Syst Rev. 2010;12:CD004714.
- Wilkins EM. Clinical practice of the dentalhygienist. 10th ed. Philadelphia, Pa: Lippincott,Williams & Wilkins; 2009.
- American Diabetes Association. Living withdiabetes: Checking your blood glucose. Availableat: www.diabetes.org/livingwithdiabetes/treatment-and-care/blood-glucosecontrol/checking-your-blood-glucose.html. Accessed December 6, 2012.
- American Diabetes Association. Living withdiabetes: A1C. Available at:www.diabetes.org/living-with-diabetes/treatmentand-care/blood-glucose-control/a1c. Accessed December 6, 2012.
- Weinberg MA, Theile CMW, Fine JB. Oralpharmacology for the dental hygienist. 2nd ed.Upper Saddle River, NJ: Pearson; 2012.
- American Diabetes Association. Living withdiabetes: Insulin routines. Available at:www.diabetes.org/living-with-diabetes/treatmentandcare/medication/insulin/insulin-routines.htmlAccessed December 6, 2012.
- Boyd LD, Hartman-Cunningham M, CalomeniJ. Survey of diabetes knowledge and practices ofdental hygienists. J Dent Hyg. 2008;82:43–59.
From Dimensions of Dental Hygiene. January 2013; 11(1): 62–65.



