Advancing Dentistry Into Primary Health Care
Screening for systemic disease in the dental office may become commonplace with the evolution of salivary diagnostics.
This course was published in the November 2012 issue and expires November 2015. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the association between oral health and cardiovascular disease and diabetes.
- List the effects of incorporating dental professionals into the chairside screening of medical conditions.
- Explain how saliva is used to detect the presence of systemic diseases.
- Discuss the status of current salivary diagnostic research.
Soon the phrase, “Let me check your saliva,” may become more common in a health care setting than “Let me draw your blood” when screening for various oral and systemic diseases. While dental offices are not typically used for the screening of systemic diseases today, emerging science that validates the use of saliva in diagnostics, as well as the strong scientific connection between oral and systemic health, may change this. As saliva’s potential to accurately reveal health status becomes more clear, dental professionals’ role in monitoring their patients’ systemic health, which influences their oral health, will grow. With more research uncovering the secrets of saliva and its implication for translational and clinical use, dental offices will likely change to better integrate oral and systemic health.
ORAL AND SYSTEMIC HEALTH
Studies show that cardiovascular disease (CVD), diabetes, pregnancy, and autoimmune diseases are strongly associated with oral health. Approximately 80 million Americans have some type of CVD, and it is one of the leading causes of death in the United States.1 Risk factors for CVD include smoking, diabetes, advanced age, male gender, high cholesterol levels, and hypertension.2,3 Periodontal diseases may also be a CVD risk factor. One of the landmark studies demonstrating an association between CVD and periodontitis found a higher amount of periodontal pathogens from dental plaque samples in patients with thickened intima–media of the carotid artery, which is the initial pro cess of atherosclerosis development.4 The study proposed that certain oral pathogens and their byproducts most likely adhere to and infect coronary endothelial cells, resulting in dysfunctioning endothelium (tissue of blood vessels) and eventually atherosclerosis.4
Diabetes affects 20 million Americans, with 35% to 40% remaining undiagnosed.5 Studies demonstrate that there is a higher prevalence of gingivitis and periodontitis among patients with diabetes.6 Researchers have elucidated the mechanism behind this association, showing that proinflammatory markers, such as tumor necrosis factoralpha, exacerbate insulin resistance—rendering glucose level more difficult to control. In turn, hyperglycemia in individuals with diabetes impairs their wound healing ability, and thus, the healing of periodontal damage caused by pathogens is delayed, resulting in sustained bone and attachment loss.7
Fortunately, both CVD and diabetes can be managed with lifestyle and dietary changes, especially when they are addressed early on.8 Although it is still unclear whether a causal relationship exists between oral infection and some systemic diseases, the association cannot be dismissed. responsibility should be delegated not only to physicians and nurses, but also to dental professionals.
Considering the prevalence and consequences of these conditions—such as morbidity, mortality, and elevated health care costs—on society as a whole, the entire health care community needs to support disease prevention and early intervention through screening and risk assessment. This responsibility should be delegated not only to physicians and nurses, but also to dental professionals.
Because Americans generally visit a dentist about 20% more regularly than their physician,9 integrating dentistry and dental hygiene into support for systemic disease identification needs to become an essential component of health care, with dental professionals providing chairside screening of medical conditions. If dental professionals become involved in preventive care for systemic diseases, the economic, emotional, and physical costs to not only patients but also society as a whole may be reduced.
More importantly, by identifying systemic diseases, dental professionals can deliver optimal care customized to each patient’s individual health status.
SALIVARY DIAGNOSTICS
Research into salivary diagnostics has grown along with the knowledge base supporting the oral–systemic health link. Over the past decade, much of this research has been supported by the National Institute of Dental and Craniofacial Research.10 In 2010, President Obama set a goal of detecting diseases using saliva and recognized it as one of the “grand challenges of the 21st century.”11
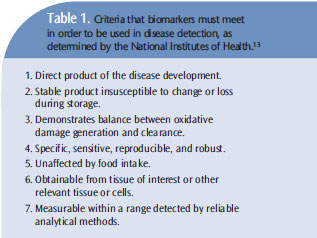
Conventionally, molecules such as DNA, RNA, proteins, enzymes, hormones, growth factors, and antibodies in blood, urine, and cerebrospinal fluid have also been used for diagnostic purposes. All of these constituents are also present in saliva.10 Molecules in saliva are secreted from salivary glands and from exudate formed by serum (blood). Physiological changes due to diseased conditions can alter genetic expression of specific genes, and such alteration can then can be used for detection of some diseases.12 Specifically, a person’s hormonal, emotional, immunological, neurological, nutritional, and metabolic changes can affect some salivary molecules, also called biomarkers, which can be used to detect certain diseases if they meet the criteria determined by the National Institutes of Health (Table 1).13
Saliva has notable advantages as a diagnostic tool over other bodily fluids because it is easy, safe, and cost–effective to collect, store, transport, and process.10 Saliva collection is noninvasive compared to blood drawing, which may enhance compliance with screening, especially among young, medically complex, or anxious patients.10 Consequently, population–wide screening for disease will be possible, which will reduce its associated morbidity and mortality. Early detection is key to reducing health care costs.
One concern about using saliva for translational and clinical applications is that the salivary biomarkers are present in small amounts,14 however, emerging molecular technologies have overcome this challenge by allowing detection of these molecules with high sensitivity, specificity, precision and accuracy.3
PROGRESS IS UNDER WAY
 Translational and clinical applications of saliva are rigorously being pursued and researched. The focus of most ongoing research is on finding biomarkers specific to certain disease conditions. Salivary biomarkers of oral squamous cell carcinoma (OSCC) are some of the most well–studied. Various studies have validated salivary biomarkers with high specificities and sensitivities, meaning their presence is associated with OSCC with high clinical accuracy.15 Moreover, certain biomarkers are associated specifically with early stages of OSCC.16 Periodontal disease is another oral disease in which salivary biomarkers are specific. The biomarkers specific for different stages of periodontal diseases aid not only in detection but also in monitoring disease progression, which is key to appropriate treatment planning. Point–of–care technologies (POCT) are being developed that can quickly measure salivary proteins, such as matrix metalloproteinase–8. This enzyme plays a crucial role in tissue destruction in periodontal diseases and can be detected using saliva samples as small as 20 ?L.17 In addition to its use in detecting oral diseases, saliva can also be utilized to detect systemic diseases that are distant from the oral cavity. Saliva testing is well–accepted in the identification of the human immunodeficiency virus (HIV).18 HIV testing detects antibodies against HIV present in saliva. Because of its reliability and accuracy, the US Food and Drug Administration (FDA) approved saliva–based HIV testing for clinical use in 2004.18
Translational and clinical applications of saliva are rigorously being pursued and researched. The focus of most ongoing research is on finding biomarkers specific to certain disease conditions. Salivary biomarkers of oral squamous cell carcinoma (OSCC) are some of the most well–studied. Various studies have validated salivary biomarkers with high specificities and sensitivities, meaning their presence is associated with OSCC with high clinical accuracy.15 Moreover, certain biomarkers are associated specifically with early stages of OSCC.16 Periodontal disease is another oral disease in which salivary biomarkers are specific. The biomarkers specific for different stages of periodontal diseases aid not only in detection but also in monitoring disease progression, which is key to appropriate treatment planning. Point–of–care technologies (POCT) are being developed that can quickly measure salivary proteins, such as matrix metalloproteinase–8. This enzyme plays a crucial role in tissue destruction in periodontal diseases and can be detected using saliva samples as small as 20 ?L.17 In addition to its use in detecting oral diseases, saliva can also be utilized to detect systemic diseases that are distant from the oral cavity. Saliva testing is well–accepted in the identification of the human immunodeficiency virus (HIV).18 HIV testing detects antibodies against HIV present in saliva. Because of its reliability and accuracy, the US Food and Drug Administration (FDA) approved saliva–based HIV testing for clinical use in 2004.18
The use of saliva is also promising in the early detection of Sjögren’s syndrome, a chronic autoimmune disease that affects more than 4 million Americans. Patients with Sjögren’s syndrome experience dry eyes (xerophtalmia), xerostomia, and sometimes rheumatoid arthritis or systemic lupus erythematosus.
The pathology is manifested by altered electrolyte concentration and various types of immunological and inflammatory molecules. Therefore, the current diagnosis is based on reduced salivary flow instead of biomarkers.19 Research is ongoing to develop salivary biomarkers for Sjögren’s syndrome detection.
Salivary diagnostics may also help in the early detection of other systemic cancers. Saliva of patients with breast and epithelial ovarian cancers has also shown increased levels of certain biomarkers compared to that of healthy patients. This change in salivary biomarkers has a positive correlation with the level of biomarkers in serum.20 In the case of breast cancer, a protein called c–erbB–2 or Her2/neu, a biomarker examined in tissue biopsy of patients with malignant tumors, is also found at higher levels in saliva and serum of women diagnosed with breast cancer. This biomarker can then be potentially used not only for early detection of malignant breast tumors but also subsequent monitoring of the tumor.20
Pancreatic cancer is another fatal malignancy with high mortality upon diagnosis.10 Early detection can significantly reduce the mortality among patients with resectable pancreatic cancer.10 Unfortunately, the early detection methods currently used have drawbacks such as invasiveness, lack of specificity and sensitivity, and limited use to patients who meet stringent criteria (lack of generalizability). Researchers at the University of California, Los Angeles, have discovered salivary biomarkers that are specific for malignant pancreatic cancer that can discriminate from other noncancerous pancreatic diseases with overlapping phenotypic manifestations.21 Salivary diagnostics have also been used in the early detection of CVD, even before symptoms are observed. In serum, human C–reactive protein (CRP) has been used to indicate the risk of coronary diseases. It has been shown that a certain concentration of CRP in saliva can also distinguish diseased patients from healthy subjects.22
THE FUTURE IS BRIGHT
If salivary diagnostics becomes fully integrated as a chairside screening tool in dental practice, its impact on many public health concerns may be significant. Before reaching this clinical reality, there are still obstacles to overcome. Even though many studies have discovered promising biomarkers, they need to ensure their validity in specific clinical context.
Once specific and sensitive biomarkers are validated, the mechanisms by which these biomarkers can indicate certain diseases also need to be elucidated. this clinical reality, there are still obstacles to overcome. Even though many studies have discovered promising biomarkers, they need to ensure their validity in specific clinical context. Once specific and sensitive biomarkers are validated, the mechanisms by which these biomarkers can indicate certain diseases also need to be elucidated.
After establishing a panel of biomarkers for each disease, POCT that can measure these biomarkers for different diseases needs to be developed. Currently, “lab–on-a– chip” technology is underway to achieve this goal of detecting multiple biomarkers for various diseases (Figure 1). POCT also allows customized medical care in a timely manner. The technology not only saves patients’ time but also improves their willingness to follow up by providing results immediately after the test. POCT will also enable clinicians to rapidly make treatment plans in the case of critical care settings, enhancing patient outcomes. Moreover, POCT can benefit countries without access to conventional laboratory tests. This technology needs to be refined to reach higher sensitivity, specificity, and scale, as well as to reduce the time needed for processing. Cost–effectiveness must also be demonstrated in order to be more readily accepted and used effectively by clinicians.19

In order to implement salivary diagnostics into practice, insurance policy and reimbursement need to be addressed. Insurance companies are generally supportive of preventive medicine to save long–term health care costs by intervening early. Most likely, third party payers are aware of these emerging opportunities and how they may alter the landscape of dentistry.
Even if all of these logistical issues concerning scientific and technical matters are resolved, there is yet another crucial step before salivary diagnostic tools become a clinical reality—the receptiveness of dental professionals and patients. Opposition must also be overcome from those within the medical and business communities who may resist a change in the conventional delivery system. However, recent studies have shown that dental professionals may respond positively to salivary diagnostics in the dental office. In Greenberg’s 2010 survey, 8 87% of the 1,945 US general dentists surveyed recognized the importance of conducting medical screening for diseases with high public health concern. A majority of the respondents also expressed willingness to conduct screening in their practices if it generated immediate results. They preferred collecting saliva to serum for diagnostic purposes. Intervention by dental professionals to prevent systemic diseases is not a completely new concept as many have counseled patients for smoking–cessation and screened for oral cancer. Another study demonstrated the efficacy of chairside screening by dental professionals in identifying patients at high risk of CVD, which especially benefited those who were unaware of their conditions.23
CONCLUSION
What is the role of dental hygienists with this emerging technology that can change the landscape of dental practices? As health care providers who see patients more routinely than other medical professionals, dental hygienists are at the forefront of monitoring their patients’ systemic health, in addition to oral health. Salivary diagnostics should not charge dental hygienists with the task of diagnosing patients’ systemic conditions. Rather, it is a way of prompting patients to consult with their physicians in case of positive or questionable results, and reassurance in the presence of negative results. If dental professionals are open to salivary diagnostics, in addition to being properly trained on using these emerging early detection tools, the future of health care delivery, as well as patient outcomes, may significantly benefit.
REFERENCES
- United States Centers for Disease Control andPrevention. Heart disease facts and statistics. Available at: www.cdc.gov/heartdisease/statistics. htm. Accessed October 17, 2012.
- Roger VL, Go AS, Lloyd–Jones DM, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2—e220.
- Malamud D, Rodriguez–Chavez IR. Saliva as a diagnostic fluid. Dent Clin North Am. 2011;55:159—178.
- Desvarieux M, Demmer RT, Rundek T, Boden–Albala B, Jacobs DR Jr, Sacco RL, Papapanou PN. Periodontal microbiota and carotid intima–media thickness: the Oral Infections and VascularDisease Epidemiology Study (INVEST). Circulation. 2005;111:576—582.
- National Center for Health Statistics. Chartbookon trends in the health of Americans: Table 55. Available at: www.cdc.gov/nchs/hus.htm.Accessed October 17, 2012.
- Papapanou PN. Periodontal diseases:epidemiology. Ann Periodontol. 1996;1:1—36.
- Willershauschen–Zonchen B, Lemmen C,Hamm G. Influence of high glucose concentrations on glycosaminoglycan and collagen synthesis in cultured human gingival fibroblasts. J Clin Periodontol. 1991;18:190—195.
- Greenberg BL, Glick M, Frantsve–Hawley J,Kantor ML. Dentists’ attitudes toward chairside screening for medical conditions. J Am Dent Assoc. 2010;141:52—56.
- Wong DT. Salivaomics. J Am Dent Assoc.2012;143(Suppl):19S—24S.
- Lee YH, Wong DT. Saliva: an emergingbiofluid for early detection of diseases. Am J Dent. 2009;22:241—248.
- Kalil T. Grand challenges of the 21st century.Available at: www.whitehouse.gov/blog/2010/02/04/grand–challenges–21st–century. Accessed October 17, 2012.
- Wong LJ, Lueth M, Li XN, Lau CC, Vogel H.Detection of mitochondrial DNA mutations tumor and cerebrospinal fluid of medulloblastoma patients. Cancer Res. 2003;63:3866—3871.
- Griffiths HR, Møller L, Bartosz G, et al.Biomarkers. Mol Aspects Med. 2002;23:101—208.
- Miller SM. Saliva testing: A nontraditional diagnostic tool. Clin Lab Sci. 1994;7:39—44
- Hu S, Wong DT. Oral cancer proteomics. CurrOpin Mol Ther. 2007;9:467—476.
- Parkin DM, Bray F, Ferlay J, Pisani P. Globalcancer statistics, 2002. CA Cancer J Clin. 2005;55:74—108.
- Herr AE, Hatch AV, Throckmorton DJ, et al.Microfluidic immunoassays as rapid saliva–based clinical diagnostics. Proc Natl Acad Sci USA. 2007;104:5268—5273.
- Malamud D. Oral diagnostic testing for detecting human immune–deficiency virus–1 antibodies: a technology whose time has come. Am J Med. 1997;102:9—14.
- Liu J, Duan Y. Saliva: A potential media fordisease diagnostics and monitoring. Oral Oncol. 2012;48:569—577.
- Streckfus C, Bigler L, Tucci M, Thigpen JT. Apreliminary study of CA15–3, c–erbB–2, epidermal growth factor receptor, cathepsin–D, and p53 in saliva among women with breast carcinoma.Cancer Invest. 2000;18:101—109.
- Zhang L, Farrell JJ, Zhou H, et al. Salivary transcriptomic biomarkers for detection of resectable pancreatic cancer. Gastroenteroloy. 2010;138:949—957.
- Punyadeera C, Dimeski G, Kostner K,Beyerlein P, Cooper–White J. One–step homogeneous C–reactive protein assay for saliva. J Immunol Methods. 2011;373:19—25.
- Greenberg BL, Glick M, Goodchild J, Duda PW,Conte NR, Conte M. Screening for cardiovascular risk factors in a dental setting. J Am Dent Assoc. 2007;138:798—804.
From Dimensions of Dental Hygiene. November 2012; 10(11): 46–49.



