
FDA Releases New Guidelines for Medication Labeling
Helping your patients use analgesics safely.
This course was published in the November 2009 issue and expires November 2012. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe the warning information required on labels for all over-the-counter antipyretic, analgesic, and antirheumatic medications including acetaminophen and nonsteroidal anti-inflammatory drugs.
- Identify the maximum daily dose for acetaminophen for adults, for children younger than 12 years of age, and for individuals who have hepatitis C.
- Advise patients who are taking acetaminophen or NSAIDs on their safe usage.
The Food and Drug Administration (FDA) issued a final ruling April 24, 2009, that requires manufacturers of over-the-counter pain relievers, antirheumatic agents, and fever reducers to revise the labeling of these analgesic products.1 The new required labeling includes warnings about the drugs’ potential safety risks, such as liver damage with excessive doses of acetaminophen and internal bleeding with average doses of nonsteroidal antiinflammatory agents (NSAIDs). Drug companies have until April 20, 2010, to comply with the new labeling requirements.
Because these drugs are used by millions of consumers each year and are commonly recommended in the dental office, dental hygienists need to be aware of these new guidelines in order to help advise their patients on the drugs’ safe usage.
DRUG FACTS
Acetaminophen and NSAIDs are widely used by children and adults to relieve pain and reduce fever. These drugs are also frequently recommended in the dental practice prior to or following procedures that may result in pain and inflammation. Other uses include the treatment of various types of arthritis and dysmenorrhea (severe uterine pain during menstruation). Acetaminophen is often the first choice for treating children with viral illnesses; managing arthritis, treating patients who have gastrointestinal (GI) conditions and cannot take NSAIDs; and treating bleeding disorders, cardiovascular disease, and renal disease.2
Acetaminophen and NSAIDs are cyclooxygenase (COX) inhibitors. A type of enzyme, COX creates key biological mediators called prostanoids. The drug-induced inhibition of COX can offer relief from pain and the symptoms of inflammation. Nonselective NSAIDs inhibit both COX 1 and COX 2 whereas a selective NSAID inhibits only COX 2. See Table 1 and Table 2 for examples of nonselective NSAIDs and selective NSAIDs. Acetaminophen inhibits COX 3.3
Acetaminophen and NSAIDs may be purchased over the counter or in prescription strength. These drugs may be used by themselves, but they are often used in combination with other ingredients such as opioids (hydrocodone, codeine); cold medicines; and antihistamines.
RECOMMENDED DOSAGES OF ACETAMINOPHEN
The maximum daily dose of acetaminophen for adults is 4 g within 24 hours, and for children younger than 12 years the maximum dose is 2.6 g within 24 hours.3 Acetaminophen is one of the most commonly used drugs in the United States, yet data show that its overuse can cause serious liver injury.4 Problems with acetaminophen use are principally due to overdosage of the drug, which can occur when individuals are unaware that acetaminophen is present in another drug they are taking. For example, when the combination of acetaminophen and hydrocodone is used for pain but the pain relief is not sufficient, the individual may self-administer an over-thecounter agent, such as Tylenol (acetaminophen). The acetaminophen/ hydrocodone drug contains 500 mg of acetaminophen and 5 mg of hydrocodone.5 The normal dose range of acetaminophen/ hydrocodone for adults is one to two tablets every 4 hours to 6 hours as needed for pain relief.5 Over a 16-hour period, if two tablets are consumed in each administration segment, 4 g of acetaminophen will be ingested. If additional over-the-counter doses are taken during the same 2-day to 4-day period, an unintentional overdose can occur.4,6
Calculating the total amount of acetaminophen ingested after using different products is difficult. Some professional associations have guidelines that conflict with normal dose recommendations approved by the FDA. The American Association for the Study of Liver Disease Clinical Practice Guidelines state that patients with chronic hepatitis C should be treated with a maximum daily dose of 2 g of acetaminophen rather than the over-thecounter maximum daily dose of 4 g. Conflicting data exist about whether acetaminophen can be safely taken at labeled doses (4 g/day) by individuals with liver disease.7 The FDA advises consumers who have liver disease to consult with their physician before using acetaminophen.
MECHANISM OF ACETAMINOPHEN TOXICITY
Unlike other commonly used drugs that reduce pain and fever (aspirin, ibuprofen, naproxen), acetaminophen does not cause adverse effects when used at recommended doses. The FDA warning is based on data that indicates unintentional overuse (or overdose) of acetaminophen is associated with a large number of emergency department visits and hospital admissions, possibly causing an estimated 100 deaths each year.2
The main danger of acetaminophen overdose is the drug’s production of a toxic metabolite. This toxic metabolite binds with liver proteins, resulting in hepatic cellular injury. The toxicity ranges from abnormalities in liver function blood tests to acute liver failure. Toxicity can occur when the amount of acetaminophen taken exceeds the recommended total daily dose by a small amount (5 g to 7.5 g/day).9 The onset of liver damage may be difficult to recognize because the symptoms can take several days to appear, are frequently nonspecific, and may mimic signs of the flu.3 In addition, the maximum safe dose may not be the same for all individuals because of variances in age and systemic health status. Some medical conditions may cause individuals to be overly sensitive to acetaminophen effects. Individuals who use alcohol or have liver disease may be overly sensitive to acetaminophen because they produce more toxic metabolites or because they are unable to easily clear the metabolite from the body.3,9 The FDA reports that not enough research has been done on the effects of drinking alcohol while taking acetaminophen.2,9 However, given common knowledge that excessive use of alcohol can damage the liver, the FDA decided to install specific warnings regarding the concurrent use of acetaminophen and alcohol.9
Identifying acetaminophen as an ingredient within other medications is also a problem. Prescription products that contain acetaminophen are often labeled as APAP, especially when acetaminophen is combined with an opioid. Individuals who are unfamiliar with this acronym may not know the product contains acetaminophen and may unknowingly take other products containing acetaminophen, resulting in an overdose.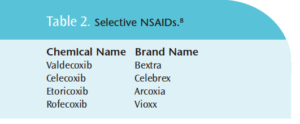
Acetaminophen liquid preparations for children come in a variety of strengths (160 mg/5 mL, 166.6 mg/5 mL, 500 mg/5 mL, 100 mg/mL).10 Liquid preparations are frequently more concentrated to permit the correct dose using less liquid. However, if more than one preparation is given with different strengths, an accidental overdose may result. For example, 100 mg per 1 mL is approximately three times more concentrated than 160 mg acetaminophen in 5 mL of liquid.
The FDA determined that the association between acetaminophen and liver injury is not widely known.9 Advertisements of over-the-counter products emphasize the effectiveness of the product but may not provide adequate warning information about potential toxicities. Acetaminophen can also cause excessive bleeding when taken in combination with warfarin, an anticoagulant.9,11,12 The use of acetaminophen and warfarin may dangerously raise individuals’ international normalized ratio (INR)—a laboratory blood test used to monitor therapeutic levels of warfarin—when therapeutic doses are consumed for more than 4 days.11,12
NSAID TOXICITY
NSAIDs are acidic in nature and can injure GI mucosa in some situations. The risk for GI bleeding with NSAIDs may be increased in individuals who regularly use NSAIDs in recommended doses.2 GI bleeding can develop when NSAIDs and anticoagulants or steroids are taken at the same time.9 Other conditions specifically associated with stomach bleeding include the following: when multiple NSAIDs are taken at the same time; in individuals who have GI disease or peptic ulcer disease; individuals who are 60 years of age or older; or when NSAIDs are taken longer than directed.2 Aspirin is contraindicated in individuals with peptic ulcer disease because it can aggravate the condition.3 All NSAIDs can reduce the antihypertensive effect of antihypertensive agents.3,4 Alcohol use can increase the risk for stomach bleeding with or without concurrent NSAID use.
LABELING
The FDA previously addressed the labeling of acetaminophen and NSAIDs in December 2006. Past advisories required that all over-thecounter acetaminophen products include an alcohol warning on their labels.2,13 An FDA Advisory Committee recommended a specific and distinctive labeling on over-the-counter packages warning of liver toxicity.13 In 2004, the FDA began a public education campaign about the risk of acetaminophen overdosing and liver injury and has expanded efforts regarding this warning since then.2,9 The organization made requests to every State Board of Pharmacy to consider the following changes: relabeling prescription products that contained acetaminophen to use the term “acetaminophen” instead of APAP; providing instructions for patients about avoiding the use of other acetaminophen-containing products so as not to exceed the recommended dosage of 4 g; and adding a warning about avoiding alcohol while taking acetaminophen prescriptions.2 Unfortunately, the FDA was informed by the National Association of Boards of Pharmacy that as of February 2008 no states had implemented the requested regulations.2 Table 3 includes the FDA proposed regulations for over-the-counter labeling for acetaminophen and NSAID products proposed in 2006 and the revisions done in 2009. The final version of this regulation is currently under review.
NEW REGULATIONS
1 Labels for over-the-counter NSAIDs must include warnings of GI bleeding even when recommended doses are taken and include labeling that states aspirin is an NSAID.9 The active ingredients of the drugs must be prominently displayed on drug labels on both packages and bottles.
CLINICAL APPLICATIONS FOR DENTAL HYGIENISTS
Dental hygienists review patients’ health and drug histories at each appointment to identify any clinical implications.3,14 When acetaminophen is reported on a patient’s health history, the milligram content in the specific product should be verified. Doseforms (tablets, capsules, gelcaps) of acetaminophen can include 325 mg, 500 mg, or 650 mg per doseform. The patient should understand the maximum daily dose should not exceed 4 g and be able to calculate how much acetaminophen is being consumed per day. One thousand milligrams equal 1 g.
When the dentist prescribes a combination product with acetaminophen, the patient must understand that acetaminophen is included in the product and that other pain relievers at home should not be used with the prescription. Patients should also be informed of the potential risk of consuming alcohol in conjunction with acetaminophen.
Dental hygienists should review the drug history for potential drug interactions with acetaminophen, such as warfarin. If acetaminophen is needed for oral pain, the patient should be advised to monitor the INR levels during concurrent acetaminophen administration with warfarin.
Because GI bleeding is a side effect of alcoholism (and the acidic nature of NSAIDs can irritate the GI mucosa and stimulate additional bleeding), the most appropriate analgesic for alcoholic individuals is acetaminophen. It is unclear if acetaminophen dose reduction is warranted in the alcoholic, but the FDA suggests reducing the dose in alcoholic individuals to 2 g/day.9
NSAIDs are excellent analgesics for the relief of oral pain3 but should not be recommended in certain situations. They are contraindicated in individuals with peptic ulcer disease.3,5,14 NSAIDs should be used with caution when antihypertensive medications are taken as they can reduce the antihypertensive effect of some medications.3,5 Acetaminophen is the preferred analgesic when peptic ulcer disease or hypertension drug therapy is present.
Reviewing the drug history section of the health history can have important implications for patient safety. It should be a standard of care to inform patients of the effects of drugs being taken, and provide information on recommended dosages and warnings when they pertain to patients’ systemic health.
REFERENCES
1. FDA requires additional labeling for over-the-counter pain relievers and fever reducers to help consumers use products safely. Available at: www.fda.gov/bbs/topics/NEWS/2009/NEW02004.html. Accessed October 6, 2009.
2. June 29-30, 2009: Joint Meeting of the Drug Safety and Risk Management Advisory Committee with the Anesthetic and Life Support Drugs Advisory Committee and the Nonprescription Drugs Advisory Committee: Meeting Announcement. Available at: www.fda.gov/AdvisoryCommittees/Calendar/ucm143083.htm. Accessed October 6, 2009.
3. Pickett FA, Terezhalmy GT. Basic Principles of Pharmacology with Dental Hygiene Applications. Baltimore: Lippincott Williams & Wilkin; 2009:99-114.
4. Larson AM, Polson J, Fontana RJ, et al. Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology. 2005;42:1364-1372.
5. Pickett FA, Terezhalmy GT. Dental Drug Reference with Clinical Implications. 2nd ed. Baltimore: Lippincott Williams & Wilkins; 2009:197.
6. Bower WA, Johns M, Margolis HS, Williams IT, Bell BP. Population-based surveillance for acute liver failure. Am J Gastroenterol. 2007;102:2459-2463.
7. Benson GD, Koff RS, Tolman KG. The therapeutic use of acetaminophen in patients with liver disease. Am J Therapeutics. 2005;12:133-141.
8. United States Food and Drug Administration. COX-2 Selective (includes Bextra, Celebrex, and Vioxx) and Non-Selective Non-Steroidal Anti-Inflammatory Drugs (NSAIDs). Available at: www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm103420.htm. Accessed October 6, 2009.
9. Department of Health and Human Services. Food and Drug Administration. Organ-Specific Warnings; Internal Analgesic, Antipyretic, and Antirheumatic Drug Products for Over-the-Counter Human Use; Final Monograph. Available at: http://edocket.access.gpo.gov/2009/pdf/E9-9684.pdf. Accessed October 6, 2009.
10. Drug Facts and Comparisons 2009. St. Louis: Wolters Kluwer Health; 2009:820.
11. Hylek EM, Heiman H, Skates SJ, Sheehan MA, Singer DE. Acetaminophen and other risk factors for excessive warfarin anticoagulation. JAMA. 1998:279:657-662.
12. Parra D, Beckey NP, Stevens GR. The effect of acetaminophen on the International Normalized Ratio in patients stabilized on warfarin therapy. Pharmacotherapy. 2007;27:675-683.
13. FDA Proposes Labeling Changes to Over-the-Counter Pain Relievers. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2006/ucm108811.htm. Accessed October 6, 2009.
14. Pickett FA, Gurenlian JR. Preventing Medical Emergencies: Use of the Medical History. 2nd Ed. Baltimore: Lippincott Williams & Wilkins; 2010:1-233,199-200.
From Dimensions of Dental Hygiene. November 2009; 7(11): 54-57.



