Ensure the Efficacy of Tooth Whitening
Tips for monitoring color change during the bleaching process.
This course was published in the May 2013 issue and expires May 2016. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the different types of whitening treatments.
- Identify the reasons why professionally supervised whitening is the preferred treatment plan.
- List the different kinds of shade guides available.
- Explain how instrumental methods are used to monitor color change.
The availability of OTC products and do-it-yourself methods has improved consumers’ access to whitening. However, the use of these materials without the supervision of a dental professional has raised several concerns, such as the inability to diagnose the etiology of the discoloration; overuse of whitening material, causing adverse events on the enamel surface; and inability to monitor the progress of tooth color change.4–7
Proper recording of baseline tooth color and subsequent monitoring of color change are essential for patient satisfaction and can only be provided in the dental operatory.
SHADE GUIDES
Recording the baseline tooth color prior to whitening can be performed using visual or instrumental methods. The quality of visual shade matching is influenced by many factors such as the shade guide used, individual shade matching ability, shade matching conditions, and the shade matching method utilized.8
Traditional shade guides used for visual shade matching include tabs of varying tooth colors. The clinician chooses the shade that most closely matches the tooth color and takes photographs of the patient’s teeth along with the tab selected. Many of these guides were hampered by limitations, such as lack of logical order, uniform color distribution, and variety of light shade tabs. Newer versions designed specifically for tooth whitening offer a wider color range and more consistent color distribution. They are typically easy to arrange and simple to navigate.9
Regardless of which shade guide is used, patients should be asked to remove anything that could attract the attention of the clinician who is performing the color evaluation, such as large jewelry, lipstick, and eyeglasses. The tooth color should be evaluated on clean teeth that are not dehydrated. The eyes of the evaluator should be aligned evenly with the patients’ teeth from a distance of 25 cm to 33 cm under a diffuse light source. Single shade measurements should not exceed 5 seconds and a neutral gray card can be used between observations.8

INSTRUMENTAL METHODS FOR SHADE DETERMINATION
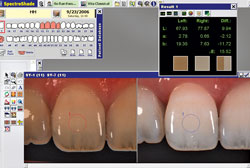
Specialized instrumental methods for shade determination are now available. They measure tooth color objectively without the influence of the human eye, environment, or light source, and provide reproducible results.10 The systems use classifications based on RGB, spectrophotometers, or colorimeters.
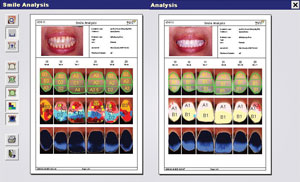
Spot measurement devices provide an easy and quick way to establish baseline color. These instruments typically use a fiberoptic tip approximately 5 mm in diameter to measure a broad range of shades. They also provide extended color information. Complete tooth measurement devices provide reliable data about the color map of the entire tooth. The image software enables many types of analyses once the image and pixilated spectral data are calculated. Print outs of patients’ smile analyses (Figure 1) can boost motivation to initiate tooth whitening. However, the complexity of the design, which combines digital imaging with spectrophotometric analysis, makes it more expensive.


TIPS FOR MONITORING TOOTH COLOR CHANGE
Professionally supervised whitening can be performed in the office with highly concentrated materials of up to 40% hydrogen peroxide, and are frequently combined with light-activating sources to speed up the process. Professionally dispensed, patient-applied home whitening kits come with custom fabricated trays and a wide range of carbamide peroxide gels (7.0% to 22%).
Current research on the efficacy of in-office whitening vs the above mentioned home whitening has shown that both techniques provide satisfactory whitening outcomes without significant adverse effects in terms of tooth and gingival sensitivity.11,12 The efficacy of both types can be accomplished with different tools. The following tips will help clinicians monitor and demonstrate whitening progress to patients.
Patients commonly inquire about the expected final shade after tooth whitening is complete. Rather than promising a specific shade, clinicians may want to suggest that the final shade will be whiter than the patient’s white of the eye. The white of the eye is a reliable reference point for monitoring the progress of tooth whitening as it is frequently whiter than the baseline tooth color (Figure 2).13
One of the best ways to demonstrate the efficacy and progress of whitening is to compare the color difference of the treated upper vs untreated lower arch. This difference is very helpful in encouraging compliance and can also be validated by friends or family (Figure 3). Photographs are essential tools for monitoring tooth whitening. The initial tab selected during baseline color measurements can be easily placed along the whitened teeth leading to the anticipation of the whitening progress (Figure 4).
The effect of tooth whitening can be easily monitored by selecting the closest shade tab before and after whitening and counting the difference in tab numbers as a new shade is achieved (Figure 5). Instrumental methods provide objective shade data (Figure 6) and enable the use of different image analysis options, such as basic shade analysis, smile analysis, and synchronization, to produce a split image of pre- vs post-whitening (Figure 7). These images effectively demonstrate objective data on the progress of tooth whitening. The overall color change can also be easily calculated and recorded.


MAINTENANCE CARE
Tooth color after whitening can be maintained for at least 1 year to 3 years and as long as 10 years with no further treatment.14 Even with some color rebound, the shade will not revert to the original color. As the color lightens throughout the whitening treatment, the patient’s interest in oral hygiene care often improves, as well. Proper maintenance methods should always be discussed at the end of treatment. Recommendations include effective self-care with proper toothbrushing and flossing, healthy diet that avoids staining foods and beverages, and regular touch-ups.
CONCLUSIONS
Professionally supervised tooth whitening offers several advantages over OTC products and do-it-yourself methods. Proper tooth color change monitoring is one of the many services that can be provided in the dental operatory with the use of different tools. This monitoring encourages compliance, motivates the patient to continue the whitening treatment to the desired level, and prevents abuse and overuse of whitening materials.
REFERENCES
- Haywood VB. History, safety, andeffectiveness of current bleaching techniquesand applications of the nightguard vital bleaching technique. Quintessence Int. 1992;23:471–488.
- Kwon SR, Li Y. Tooth whitening safety: Whatthe evidence says about the effects of bleaching on tooth structure. Dimensions of Dental Hygiene. 2012;10(5):30–39.
- Home Teeth Whitening: Baking Soda andStrawberries for a Whiter Smile. Available at: www.fitwatch.com/health/home-teethwhitening-strawberries-baking-soda-137.html.Accessed April 18, 2013.
- ADA Council on Scientific Affairs . ToothWhitening/Bleaching: Treatment Considerations for Dentists and Their Patients. Available at: www.ada.org/sections/about/pdfs/HOD_whitening_rpt.pdf. Accessed April 18, 2013.
- Cubbon T, Ore D. Hard tissue and home tooth whiteners . CDS Rev. 1991;84:32–35.
- Hammel S. Do-it-yourself tooth whitening is risky. US News and World Report. 1998;66.
- Li Y. Safety controversies in tooth bleaching.Dent Clin North Am. 2011;55:255–263.
- Paravina RD, Powers JM. Esthetic ColorTraining in Dentistry. St. Louis: Elsevier; 2004:127–172.
- Paravina RD. Ne w shade guide for tooth whitening monitoring: visual assessment. J Prosthet Dent. 2008;99:178–184.
- Chu SJ. Use of a reflectance spectrophotometer in evaluating shade change resulting from tooth-whitening products. J Esthet Restor Dent. 2003;15(Suppl):S42–S48.
- Aushill TM, Hellwig E, Schmidale S, SculeanA, Arweiler NB. Efficacy, side-effects and patients’ acceptance of different bleaching techniques (OTC, in-office, at-home). Oper Dent.2005;30:156–163.
- Giachetti L, Bertini F, Bambi C, Nieri M,Scaminaci Russo D. A randomized clinical trial comparing at-home and in-office tooth whitening techniques: A nine-month follow-up. J Am Dent Assoc. 2010;141:1357–1364.
- Haywood VB. Update on bleaching: anexamination for nightguard vital bleaching.Esthetic Dent Update. 1995;6(2):51–52.
- Leonard RH Jr, Bentley C, Eagle JC, GarlandGE, Knight MC, Phillips C . Nightgurad vita lbleaching: a long term study on efficacy, shade retention, side effects, and patients’perceptions. J Esthet Restor Dent. 2001;13:357–369.
From Dimensions of Dental Hygiene. May 2013; 11(5): 52–55.



