Dental Management of Patients with Rickets
A successful prevention protocol can significantly improve the oral health of children with this rare but serious disorder.
This course was published in the February 2013 issue and expires February 2016. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define rickets.
- Discuss the three different types of rickets.
- Identify those at risk of developing rickets.
- Explain the treatment protocols for the dental management of patients with rickets.
Rickets is a disorder that causes softening and weakening of the bones due to insufficient levels of vitamin D, calcium, and/or phosphate levels in the body.1 Vitamin D plays a vital role in the absorption of calcium and phosphate.1 Low levels of vitamin D can trigger the body to release hormones that lead to the eventual loss of calcium and phosphate from bones,2,3 which causes insufficient bone mineralization.1
Vitamin D is obtained either from food sources or produced by the body through sunlight exposure.4 The two most common forms of vitamin D are vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol).4 Vitamin D2 is obtained from plants and can be man-made in a supplement form.2,4 Vitamin D3, the most active form, is processed in the skin through ultraviolet radiation or obtained from animal sources.2,4
TYPES OF RICKETS
Rickets is present in three different forms: nutritional vitamin D deficiency rickets, vitamin D dependent rickets, and vitamin D resistant rickets.1 Nutritional vitamin D deficiency rickets affects children who have low levels of vitamin D, while vitamin D dependent rickets and vitamin D resistant rickets are inherited.1 Vitamin D dependent rickets occurs when children are unable to absorb calcium through the intestines. Vitamin D resistant rickets is present in children with unstable phosphate levels who can’t absorb calcium and vitamin D.1 All three disorders affect skeletal development and dentition formation similarly.1
VITAMIN D DEFICIENCY RICKETS
Vitamin D deficiency rickets is known as nutritional rickets and results from low levels of vitamin D being absorbed endogenously from the diet and exogenously through the epidermis.1 Although this disorder is rare in the United States, cases do occur.5 New immigrants and adopted children from other countries are most at risk in the US.5 Nutritional rickets is also seen in children who are breastfed for an extended period without vitamin D supplementation and, thus, have low levels of calcium and phosphate in the body.1
Oral manifestations include delayed tooth eruption.6 Early detection is vital when treating primary teeth in order to preserve space and prevent deformities of the permanent dentition. Physical manifestations of rickets in children include varying types of deformities of the extremities.1 Skeletal conditions may include impaired growth, leg and rib cage deformities, enlargement of wrists and ankles, costochonaral junctions, and orthopedic deformities.2 Individuals may also experience bone pain in the legs, delayed standing and walking, and growth impairment.2 These deformities may become permanent if the disorder is not diagnosed and treated early.7
VITAMIN D DEPENDANT RICKETS
Vitamin D controls the levels of calcium and bone mineralization in the body.8 Vitamin D dependent rickets is an autosomal recessive disorder characterized by hypocalcaemia, secondary hyperparathyroidism, and early onset severe rickets.3 Vitamin D dependent rickets results from a 1?-hydroxylase deficiency and is characterized by extremely low serum calcitriol levels.3 This deficiency plays a critical role in the biosynthesis of calcitriol in the body.3
Physical symptoms include joint pain and bone deformities in children.3 Vitamin D dependent rickets affects children younger than 2 and causes metabolic abnormalities that are generally treated with supplemental doses of calcitriol.3 Oral manifestations include delayed tooth eruption, dentinal defects, large pulp chambers, and enamel hypoplasia.3,9
VITAMIN D RESISTANT RICKETS

Vitamin D resistant rickets is a metabolic sex-linked dominant disorder that is caused by a gene defect, which reduces renal phosphate resorption.10 Individuals with this disorder may have unstable phosphate levels within the body, causing an inability to absorb calcium and vitamin D.1 This type of hereditary vitamin D resistant rickets with X-linked hypophosphatemic dominant rickets (XLH) is the most common form, and is caused by the inability of the kidneys to retain phosphate in the body (phosphate-wasting disorder).7 Phosphate levels are controlled by the kidneys, which are responsible for either excreting phosphate through urine or reabsorbing phosphate back into the bloodstream.1,7
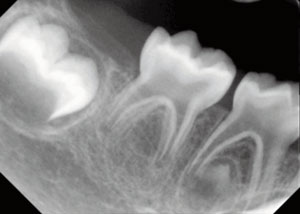
Physical manifestations have a tremendous effect on growth, and include pain and bone fractures.7 A wide range of symptoms are associated with this disorder, including growth retardation, short stature, bowing of legs, pseudo fractures, bone deformities, bone pain, boney overgrowths, and dentin defects.7 Dental manifestations associated with XLH can include: enamel hypoplasia, hypocalcification, hypominerilization, and interglobular dentin.11–17 A study by Seow suggests that hypophosphatemia leads to the formation of interglobular dentin within the tooth, which significantly impairs the calcification of the primary and permanent dentition.18 The globular dentin is formed when the channels within the dentin do not mature beyond the dentin-enamel junction, thus creating gaps between these junctions. These gaps are where globular dentin eventually forms.18 This impaired calcification creates microscopic enamel cracks and dentinal microleakage within the tooth. The resulting hypomineralized dentin and enamel can trap bacteria and microorganisms, which often leads to dental abscesses.19–21 Primary teeth in patients with XLH also exhibit high pulp horns and large pulp chambers, described as taurodontism, which make primary teeth more susceptible to abscesses19,22,23
CASE STUDY

This case study reports on the dental treatment and dental hygiene care for a patient with XLH rickets. A 3-year-old boy presented to Texas Scottish Rite Hospital in Dallas with a medical history of maternally-inherited XLH rickets. The patient was 2.84-ft tall and weighed 32 lbs. Developmentally, the patient appeared age appropriate and his vital signs were within normal limits.
The boy was born in Hawaii and moved to Dallas with his family to pursue treatment for the disorder. The mother stated that she breastfed her son until 14 months with no vitamin D supplementation. The patient’s mother, maternal grandfather, and maternal aunt also have XLH. The mother reported that, as a child, she also had rampant dental abscesses and pulpectomy therapies.
Past medical treatments included a tonsillectomy and craniotomy surgery to close the sagittal suture. These procedures were performed before dental treatment was initiated. The patient’s current medications included Phos-NaK (potassium phosphate/ sodium phosphate), calcitriol (vitamin D), and ibuprofen. The patient was taking one pack of Phos-Nak Oral powder three times a day to increase phosphate levels, calcitriol 0.25 mg per day as a vitamin D replacement, and ibuprofen as needed to reduce inflammation and pain.
The patient presented wit numerous dental abscesses along with additional symptoms associated with XLH rickets, including short stature, bowing of the lower extremities, widening of the wrist, widening of the distal metaphysic femur and tibia, coxa vara, potbelly, occipital cupping, dolichocephaly, and pectus carinatum.
The patient was very cooperative and was able to walk normally and participate in activities of daily living. Although the patient did present with bowing of the legs and widening of the wrists, physical limitations were not present.
CLINICAL FINDINGS
The patient presented with dental abscesses on teeth #E and #O, with tooth #E exhibiting a greenish tint of unknown origin. Additionally two fistulas were present on the facial gingiva above teeth #E and #O. Tooth #F did not have caries, but the prognosis was poor due to severe inflammation and mobility. (Figure 2 and Figure 3) The presence of gingivitis and biofilm was minimal.
The patient’s mother brushes his teeth twice daily. He drinks filtered water at home and tap water at day care. The boy and his and family follow a vegan diet. The patient’s pediatrician recommended adding fortified orange juice to his diet to increase iron levels. The widening in the boy’s wrist has not affected his brushing, eating with utensils, or picking up toys and crayons. He takes gummy vitamins rather than hard chewable vitamins in order to preserve the existing composite sealants.

TREATMENT PLAN
The patient was first given an initial course of antibiotic therapy to reduce the abscesses and swelling. Following antibiotic therapy, the patient underwent dental treatment to resolve clinical and radiographical abscesses and fistulas. Tooth #E was treated with a pulpectomy and restored with a composite resin restoration and tooth #O was extracted due to class I mobility. Due to a poor prognosis, teeth #E and #F were later extracted because of recurrent abscesses (Figure 4).
Common treatments performed on patients with XLH rickets include full mouth pulpectomies, placement of posterior stainless steel crowns, and anterior composite resin restorations. While discussing treatment options, the patient’s father brought up a study done in another country on a child with the same disorder who was treated with flowable sealants on all surfaces of the primary teeth. Since this was not a common form of treatment for XLH rickets, the patient’s parents signed a consent form to approve treatment. After the attending dentist and the dental board investigated and approved the proposed treatment, flowable composite sealants were placed on the surfaces of all remaining primary teeth.
The patient visits Texas Scottish Rite Hospital every 3 months and receives periodic dental exams and a prophylaxis with fluoride application. Recare treatment includes irrigation with water, debridement, rubber cup polishing, and/or toothbrush polishing every visit, as well as fluoride varnish application. The dental hygienist recommended brushing three times daily and drinking water after consuming juice.
The patient presented at a 3-month recare with good oral hygiene and continues to be healthy. The dental resident performed toothbrush polishing, application of fluoride varnish, and a periodic oral examination. The dental hygienist reviewed oral hygiene instructions with the patient’s father and recommended the patient brush after lunch. The formation of dental abscesses could not have been prevented in this case until a diagnosis was made.
A year after sealants were placed, no spontaneous abscesses and/or dental caries have occurred. Normal, slight posterior buccal wear on the sealants was noted and the dentist recommended reapplication of sealants in 1 year. Since this disorder was diagnosed early, the patient has a very good prognosis for avoiding invasive procedures on primary teeth. When permanent teeth begin to erupt, occlusal sealants will be placed in order to prevent caries.
CONCLUSION
XLH rickets is the most common form of hereditary rickets among children and appears in one out of 20,000, occurring more frequently in boys.19 Boys are affected when the mother is a carrier of the XLH rickets trait and girls are at risk when the father and mother are carriers.19
Early diagnosis of XLH rickets can be vital in preventing extensive decay in primary teeth and allows clinicians to focus more on preventive care. Through careful and thorough management of this disorder, more conservative dental treatments can be performed, such as composite sealant restorations. However, preventive treatments, such as placement of posterior stainless steel crowns and composite resin on anterior teeth, and invasive dental treatments, including pulpotomies and extractions, are the most commonly performed dental treatments in patients with XLH rickets.24
The importance of oral hygiene should be stressed to every patient with XLH rickets. The dental hygienist should work with the patient’s parents or guardian on oral hygiene instructions and encourage early flowable sealant placement on all teeth. A successful preventive protocol can reduce the need for more invasive dental treatments. Dental hygiene treatment and management of patients with XLH rickets are vital to prevent primary and permanent tooth loss.
REFERENCES
-
- Nield LS, Mahajan P, Joshi A, Kamat D. Rickets:not a disease of the past. Am Fam Physician.2006; 74:619–626.
- Thacher TD, Clarke BL. Vitamin D insufficiency.Mayo Clin Proc. 2011;86:50–56.
- Malloy PJ, Feldman D. Genetic disorders anddefects in vitamin D action. Endocrinol Metab ClinNorth Am. 2010;39:333–346.
- Reinhold V. Vitamin D nutrition and its potential health benefits for bone, cancer andother conditions. J Nutr Environ Med.2001;11:275–291.
- Kumaravel R. Vitamin D, cod-liver oil, sunlight,and rickets: a historical perspective. Pediatrics.2003;112:e132–e135.
- Craviari T, Pettifor JM, Thacher TD, et al. Rickets:an overview and future directions, with special reference to Bangladesh. A summary of theRickets Convergence Group meeting, Dhaka, 26-27 January 2006. J Health Popul Nutr.2008;26:112–121.
- Carpenter TO, Imel EA, Holm IA, Jan de BeurSM, Insogna KL. A clinician’s guide to X-linked hypophosphatemia. J Bone Miner Res.2011;26:1381–1388.
- Tsiaras WG, Weinstock MA. Factors influencing vitamin D status. Acta Derm Venereol.2011;9:115–124.
- Zambrano M, Nikitakis NG, Sanchez-Quevedo MC, Sauk JJ, Sedano H, Rivera H. Oral and dentalmanifestations of vitamin D-dependent rickets type I: report of a pediatric case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:705–709.
- Souza MA, Soares Junior LA, Santos MA,Vaisbich MH. Dental abnormalities and oral health in patients with hypophosphatemic rickets.Clinics (Sao Paulo). 2010;65:1023–1026.
- Coelho A, Marques P, Canta JP. Case report:dental treatment of a child with hypophosphataemic rickets. Eur Arch Paediatr Dent. 2007;8(1):35-38.
- Fadavi S, Rowold E. Familial hypophosphatemic vitamin D-resistant rickets:review of the literature and report of case. ASDC JDent Child. 1990;57:212–215.
- Larmas M, Hietala EL, Simila S, Pajari U. Oral manifestations of familial hypophosphatemic rickets after phosphate supplement therapy: a review of the literature and report of case. ASDC J Dent Child. 1991;58:328–334.
- Seow WK, Needleman HL, Holm IA. Effect of familial hypophosphatemic rickets on dental development: a controlled, longitudinal study. Pediatr Dent. 1995;17:346–350.
- Kawakami M, Takano-Yamamoto T.Orthodontic treatment of a patient withhypophosphatemic vitamin-D resistant rickets.ASDC J Dent Child. 1997;64:395–399.
- Murayama T, Iwatsubo R, Akiyama S, AmanoA, Morisaki I. Familial hypophosphatemic vitaminD-resistant rickets: dental findings and histologic study of teeth. Oral Sung Oral Med Oral Pathol Oral Radiol Endod. 2000;90:310–316.
- Pereira CM, Andrade CR, Vargas PA. Dental alterations associated with x-linked hypophosphatemic rickets. J Endod. 2004;30:241–245.
- Seow WK. Diagnosis and management of unusual dental abscesses in children. Aust Dent J.2003;48:156–168.
- Batra P, Tejani Z, Mars M. X-linked hypophosphatemia: dental and histologic finding.J Can Dent Assoc. 2006;72:69–72.
- Murayama T, Iwatsubo R, Akiyama S, AmanoA, Morisaki I. Familial hypophosphatemic vitaminD-resistant rickets: dental findings and histology study of teeth. Oral Surg Oral Med Oral Pathol OralRadiol Endod. 2000;90:310–316.
- Seow WK. X-linked hypophosphatemic vitaminD-resistant rickets. Aust Dent J. 1984;29:371–377.
- McWhorter AG, Seale NS. Prevalence of dental abscess in a population of children with vitaminD-resistant rickets. Pediatr Dent. 1991;13:91–96.
- Yasufuku Y, Kohno N, Tsutsumi N, Ooshima T,Sobue S, Murakami Y. Dental management of familial hypophosphatemic vitamin D-resistant rickets: report of case. ASDC J Dent Child.1983;50:300–304.
- Rakocz M, Keating J 3rd, Johnson R.Management of the primary dentition in vitaminD-resistant rickets. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1982;54:166–171.
From Dimensions of Dental Hygiene. February 2013; 11(2): 64–67.



