Avoiding Additional Tooth Loss
Dental hygienists play an important role in helping partially edentulous patients maintain their oral health.
This course was published in the February 2013 issue and expires February 2016. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
Partially edentulous patients can be effectively served with removable partial dentures (RPDs). These devices can help patients retain their ability to chew and enjoy food, improve their esthetic appearance, and enable them to speak more clearly.1 While implant therapy and fixed bridgework are also options for those who are partially edentulous, utilizing an RPD, in some cases, may be the best treatment plan based on patient needs and desires. Dental hygienists play a key role in supporting the oral health of patients with RPDs, and in helping them retain their remaining teeth.
INDICATIONS FOR REMOVABLE PARTIAL DENTURES

RPDs are an appropriate prosthodontic choice for many types of patients. RPDs are less invasive and less expensive than fixed bridgework and implant-supported restorations. They are also simpler to adjust once fabricated than other prosthetic options.1,2
RPDs can offer patients improved speech, chewing ability, more even distribution of occlusal forces, and prevention of overeruption of unopposed teeth. Table 1 provides a list of clinical situations where RPDs are best suited.1,3,4 RPDs, however, are not without downsides. Patients with RPDs are at increased risk of plaque retention, which can lead to caries and periodontal diseases in the remaining teeth. They may experience dental trauma from the components of RPDs, and compliance may suffer if the design of the appliance is ill fitting.1
Dental hygienists can help patients with RPDs experience success with this noninvasive treatment and improve the prognosis of their remaining teeth over the long-term.
SELF-CARE FOR PATIENTS WITH REMOVABLE PROSTHESES
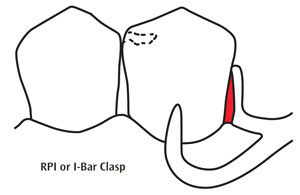
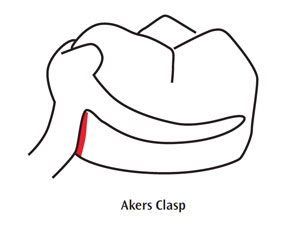
The teeth that abut RPDs require extra attention in order to ensure their health and longevity.5 Design features, such as rests, proximal plates, and clasp arms, notoriously retain food and plaque. Figure 1 shows the most commonly used clasp designs: Akers clasp and RPI/I-Bar clasp. The red areas designate where plaque retention is most problematic. These areas oppose natural teeth or abutment crowns and can increase tooth surface vulnerability to periodontal pocketing, as well as caries. The use of disclosing tablets can graphically illustrate plaque retention around abutment teeth to patients, which may motivate them to improve their self-care.
Straight mesial and distal surfaces in the partially edentulous arch can be easily missed by toothbrushing. Power toothbrushes may be helpful for partially edentulous patients, as well as for those with implant-supported prostheses.6 The use of supportive hygiene aids, such as superfloss, proxabrushes, or end-tuft brushes, can greatly facilitate plaque removal in these areas. When a patient removes his or her RPD prior to professional maintenance care, the dental hygienist should examine these areas on the appliance and instruct the patient on how to clean the prosthesis with soap (hand soap or dish soap) and a soft brush. A number of dental manufacturers make brushes and cleaning agents specifically designed for dentures.
Although many patients think it is a good idea, removable prostheses should never be cleaned with toothpaste.7 Over time, the abrasive content of the dentifrice will “scour” out the inner surface of the acrylic and cause space to form between the denture and the soft tissue, eventually resulting in a loose fit.8 Daily use of a denture cleaning tablet can minimize staining of teeth and acrylic.9 A clean denture should be stored in water. A small amount of mouthwash or vinegar can be added to the water for freshness.
Dental hygienists may be tempted to use a hand scaler or ultrasonic insert/tip to remove calculus from a partial or complete denture, and patients frequently request this. The practice, however, can produce small scratches in the metal or acrylic that promote more plaque, calculus, and stain accumulation. Placing the prosthesis in a sealed baggie with denture cleaning solution in an ultrasonic bath for 15 minutes or longer is the preferred option.10 If calculus remains on the prosthesis, the buildup may be carefully removed with hand or ultrasonic instrumentation, as long as any scratches are removed from the base acrylic.
Fine pumice powder with an air polishing prophylaxis system can be used to remove deep interproximal staining between denture teeth. The use of a laboratory wheel with light to medium grit pumice is also effective. Attention must be paid to the amount of pressure used in order to prevent injury of denture tooth surfaces.
DENTAL CARIES AND PATIENTS WITH REMOVABLE PARTIAL DENTURES
Dental hygienists need to educate partially edentulous patients about avoiding the consumption of sweetened beverages, which greatly increases their caries risk. The frequent use of breath mints or cough drops, which often have high sugar content, is also a risk factor that should be discussed during recare appointments. Patients may frequently ingest seemingly healthy items, such as dried fruit or apple juice, while remaining unaware of their impact on caries risk.
Many partially edentulous patients have xerostomia and are unaware of its effects on their oral health. Patients should be advised about the common causes of xerostomia, such as medication use and systemic medical problems, eg, Sjögren’s syndrome, diabetes, and rheumatoid arthritis. Low salivary flow results in reduced lubrication of the oral mucosa, which can lead to tissue trauma and discomfort under prostheses.11 Because patients with xerostomia are at increased risk of caries, it is imperative that they practice impeccable oral hygiene in order to prevent caries on tooth surfaces adjacent to an RPD.12
Regardless of a patient’s saliva flow, clinicians should use a formal caries management by risk assessment (CAMBRA) process to identify patients at risk of root caries. The dental hygienist may be the first clinician to notice softness on a root surface. Early intervention, such as fluoride varnish application on vulnerable tooth surfaces, can minimize the impact of caries in these areas.13
TOOTH LOSS PREVENTION
There is a misconception among patients with RPDs that the loss of another tooth is of no great consequence because it can just be added to the existing partial. An RPD may not be designed to grow or transition, particularly if a key abutment tooth is lost. The loss of a tooth that supports a rest or a clasp of a partial denture may necessitate removal and refabrication of the appliance, which is costly. In order to help reduce patient expenses, some dental offices may avoid redesigning and remaking the RPD, which can result in further tooth loss when stresses are not distributed evenly in the arch.

PATIENT EDUCATION
Dental hygienists may see a patient who is wearing a stayplate or “flipper” as a longterm prosthesis. Because these partial dentures are tissue-borne, intense gingival inflammation may be present underneath the stayplate and around its margins.14 If this is noted, the presence of candidiasis or other infections should be considered (Figure 2). These conditions may require the use of prescription medications such as fluconazole, nystatin, ketoconazole, or clotrimazole.15 Dental hygienists should encourage patients to pursue a definitive treatment plan that might include implant placement, a tooth-supported RPD, or a fixed bridge. Patients may not be aware of the soft tissue damage caused by these more inexpensive tooth replacements.
Inflammation under the resin base of an RPD, complete denture, or implant-supported prosthesis may also be due to continuous wearing of the appliance. Patients may not be aware that the denture should be removed at night in order to prevent thinning of the keratinized epithelium that occurs under constant pressure of the denture base.16 Dental hygienists should instruct patients to leave their dentures out at night to promote healthy tissues under denture-bearing surfaces.
Another patient education opportunity occurs when the dental hygienist hands the RPD back to the patient at the end of the recare appointment. Many patients use their teeth to seat or “bite” the partial to place upon insertion. This action puts stress on the metal rests of the partial denture, causing them to flex and weaken, and over time these rests can fracture off.17 The loss of a supporting metal rest significantly affects the stress distribution of the partial, and can cause mobility of abutment teeth. Patients should be advised to seat the RPD with finger pressure.
BREAKING BAD HABITS
Dental hygienists can significantly minimize the effects of dental disease on patients with RPDs. They may be the first health care providers to notice the signs of negative behaviors that patients may be afraid to discuss, such as the use of recreational drugs, smoking, or poor nutrition. Methamphetamine use, in particular, has increased dramatically DR in the United States, and its deleterious effects on the dentition are well-documented.18 Patients may not understand the devastation that these behaviors can exert on the oral cavity, and dental hygienists, who often have long-standing relationships with their patients, can provide a safe opportunity to discuss these difficult topics. Encouraging patients to begin a recovery program is invaluable. This can be done discreetly during the course of a dental hygiene appointment and local resources can be provided.
Many partially edentulous patients smoke, which increases the risk of tooth loss.19 Dental hygienists, who are well versed in tobacco cessation, can support patients in becoming tobacco-free, thereby helping them make serious improvements in both their systemic and oral health.20
CONCLUSION
Dental hygienists can make a significant difference in the oral health of patients with RPDs. By providing effective education and early detection and prevention, patients may be able to wear existing partials for much longer, and, more importantly, delay the need to transition to a complete denture. This is especially valuable in the mandibular arch because a complete denture in this area is much less satisfactory than an RPD in almost every case.
ACKNOWLEDGEMENTS
FIGURE 2: DR P. MARAZZI/SCIENCE PHOTO LIBRARY
REFERENCES
- Lynch CB. Successful removable partial dentures. Dent Update. 2012;39:122–126.
- Davenport JC, Basker RM, Heath JR, RalphJP, Glantz PO. The removable partial denture equation. Br Dent J. 2000;189:414–424.
- Craddock HL Youngson CC, Manogue M.Deviation from the Broadrick occlusal curve following posterior tooth loss. J Oral Rehabil. 2006;33:423–429.
- Ng YL, Mann V, Gulabivala K. Tooth survival following non-surgical root canal treatment: a systematic review of the literature. Int Endod J. 2010;43:171–189.
- Behr M, Zeman F, Passauer T, et al. Clinical performance of cast clasp-retained removable partial dentures: a retrospective study. Int J Prosthodont. 2012;25:138–144.
- Cagna DR, Massad JJ, Daher T. Use of a powered toothbrush for hygiene of edentulous implant-supported prostheses. Compend Contin Educ Dent. 2011;32:84–88.
- Dikbas I, Koksal T, Calikkocaoglu S.Investigation of the cleanliness of dentures ina university hospital. Int J Prosthodont. 2006;19:294–298.
- Freitas-Pontes KM, Silva-Lovato CH,Paranhos HF. Mass loss of four commercially available heat-polymerized acrylic resins after toothbrushing with three different dentifrices. J Appl Oral Sci. 2009;17:116–121.
- Alam M, Jagger R, Vowles R, Moran J.Comparative stain removal properties of four commercially available denture cleaning products: an in vitro study. Int J Dent Hyg. 2011;9:37–42.
- Cruz PC, Andrade IM, Peracini A, et al. The effectiveness of chemical denture cleansers and ultrasonic device in biofilm removal from complete dentures. J Appl Oral Sci. 2011;19:668–673.
- Noble WH, Aziz K, Edwards K, Salmon E. Xerostomia from A to Z. Dimensions of DentalHygiene. 2012;10(1):22–28.
- Featherstone JD, Domejean-Orliaguet S,Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 throughadult. J Calif Dent Assoc. 2007;35:703–713.
- Tan HP, Lo EC, Dyson JE, Luo Y, Corbet EF.A randomized trial on root caries prevention in elders. J Dent Res. 2010;89:1086–1090.
- de Baat C, Witter DJ, Creugers NH. Acrylic resin removable partial dentures. Ned Tijdschr Tandheelkd. 2011;118:32–37.
- Jacobsen PL. The Little Dental Drug Booklet.12th ed. Hudson, Ohio: Lexicomp; 2012.
- Mori S, Sato T, Hara T, Nakashima K,Minagi S. Effect of continuous pressure on histopathological changes in denture supporting tissues. J Oral Rehabil.1997;24:37–46.
- Keltjens HM, Mulder J, Käyser AF, CreugersNH. Fit of direct retainers in removable dentures after 8 years of use. J Oral Rehabil.1997;24:138–142.
- Shetty V, Mooney LJ, Zigler CM, Belin TR,Murphy D, Rawson R. The relationship between methamphetamine use andi ncreased dental disease. J Am Dent Assoc. 2010;141:307–318.
- Klein BE, Klein R, Knudtson MD. Life-style correlates of tooth loss in an adult Midwestern population. J Public Health Dent.2004;64:145–150.
- Arora M, Schwarz E, Sivaneswaran S, BanksE. Cigarette smoking and tooth loss in a cohort of older Australians: the 45 and up study. J AmDent Assoc. 2010;141:1242–1249.
From Dimensions of Dental Hygiene. February 2013; 11(2): 68–71.



