MAKSYM BELCHENKO/ISTOCK/GETTY IMAGES PLUS
MAKSYM BELCHENKO/ISTOCK/GETTY IMAGES PLUS
A Dental Hygiene Approach Toward COVID-19
The medical history provides an opportunity for clinicians to discuss COVID-19 and how patients can best protect themselves from severe illness.
This course was published in the February 2021 issue and expires February 2024. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
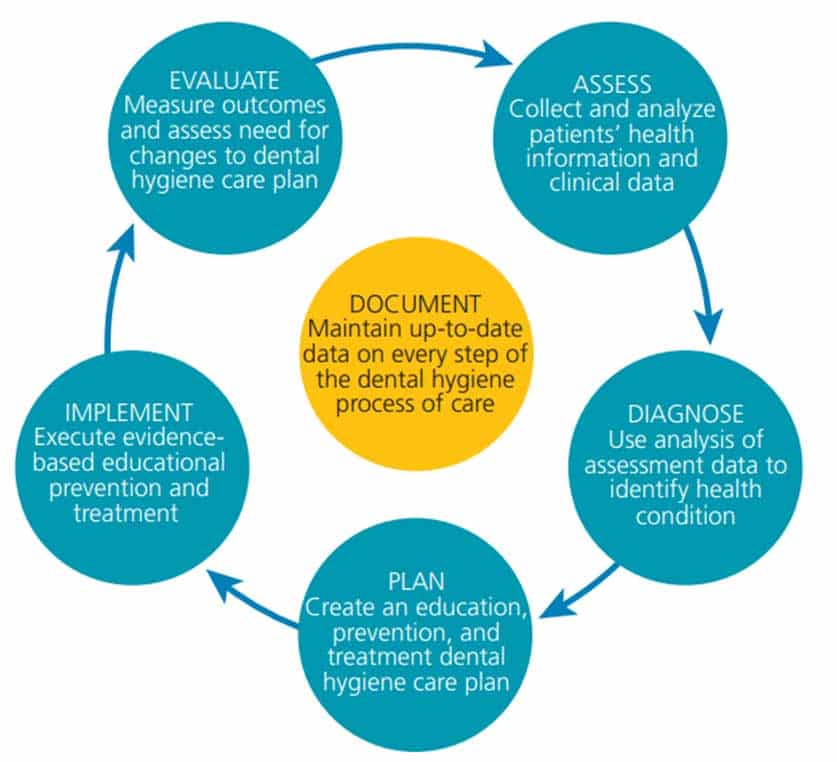
- Identify the dental hygiene process of care.
- Discuss the relationship between underlying health conditions and the risk for severe COVID-19 illness.
- Explain the role the medical history can play in educating patients about the risk of COVID-19.
- Provide patients with important information on how to protect themselves against SARS-CoV-2.
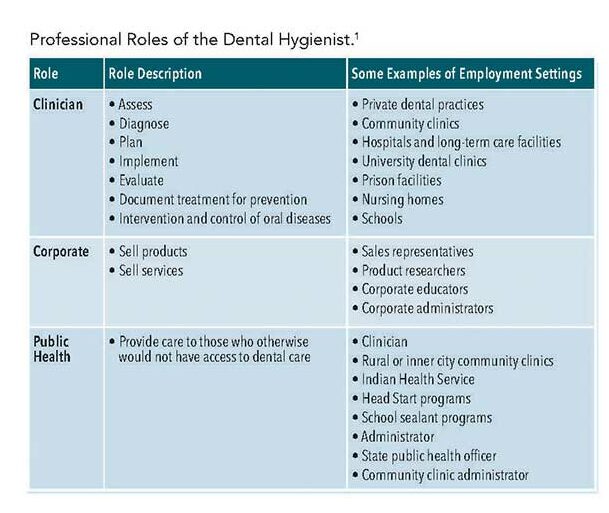
Professional dental hygiene practice is no longer defined only by the provision of oral healthcare. The dental hygienist is an educated and licensed primary dental healthcare provider who fills numerous roles.1,2 Education, promotion, and prevention are essential components of the dental hygiene practice as patients’ health cannot be improved if they do not understand the association between oral and systemic disease and do not have the knowledge and skills to properly take care of their health.
Oral conditions reflect the general health of patients. Research suggests an association between periodontal diseases and systemic conditions such as cardiovascular disease, diabetes mellitus, metabolic syndrome, obesity, and respiratory disease, among others.3–5 Additionally, evidence shows that dental procedures and outcomes may complicate or be negatively impacted by these existing physiological and or pathological conditions.1,2,6
In light of the current COVID-19 pandemic, it is more important than ever for dental hygienists to routinely apply their knowledge and skills in health education and promotion and disease prevention to help patients with systemic health problems take better care of themselves. According to the United States Centers for Disease Control and Prevention (CDC), individuals with underlying conditions are at heightened risk for severe COVID-19 illness and death.7–12
As healthcare and public health professionals, dental hygienists need to raise patients’ awareness of their susceptibility to COVID-19 and encourage them to take steps necessary to manage their chronic conditions and prevent possible infection. These conversations should take place during the assessment phase of the dental hygiene process of care and continue at any subsequent appointments.
DENTAL HYGIENE PROCESS OF CARE
The first step in the dental hygiene process of care is assessment (Figure 1).1,2 This phase involves collecting and analyzing patients’ health information and clinical data in order to provide comprehensive and adequate care. An essential part of the assessment phase is the medical history, also known as a personal health record or health history.1,2
The primary purpose of the medical history is to obtain and document information about patients’ past and present history of medical conditions and diseases, as well as to identify risk factors for oral disease and systemic conditions. In the midst of the COVID-19 pandemic, dental hygienists need to identify conditions and risk factors that may heighten patients’ risk for severe COVID-19 illness. The medical history can be obtained through a self-administered questionnaire or an interview conducted by the dental hygienist. Regardless of how the medical history is obtained, it is important to clearly and concisely document all information regarding signs, symptoms, medical conditions, and other risk factors in chronological order.1,2 Maintenance of a complete medical history is essential to providing appropriate patient care as well as for clinical, ethical, and legal risk management for professional practice.13,14
Basic medical history forms in more than 25 languages are available through the Multi-Language Health History Project at: oralfitnesslibrary.com/Home/Tools-Items/Multi-Language-Health-History-Forms. Medical history forms are also available through the American Dental Association.13 Alternatively, dental hygienists may prefer to develop their own medical history forms. An adequate form should encompass the following elements:1,2,6
- Available in the patient’s primary or dominant language to avoid language barriers and miscommunication.
- Space to record the patient’s own words.
- Space for provider notes concerning the patient’s attitudes and knowledge.
- Organized in a way that enables the dental hygienist to quickly identify important information, such as allergies and medications.
Though it seems routine, obtaining an accurate and comprehensive medical history poses numerous challenges. Patients may not understand the link between medical conditions and oral health and, thus, avoid disclosing important medical information. Similarly, patients may be unaware that dental procedures may complicate or be negatively impacted by existing physiological and/or pathological conditions. Patients may also be fearful of discrimination due to the presence of certain medical conditions.
Obtaining a thorough medical history is also challenging when dental hygienists do not ask follow-up questions to answers provided during the assessment, or when they fail to review and update patients’ medical history during subsequent appointments. Reviewing and updating the medical history during each patient encounter are vital as health status is fluid. Finally, the great diversity in ethnicity, culture, and language that exists among patients can also make it difficult for dental hygienists to communicate important health information in a way that resonates with patients.
Following are examples that may help elicit relevant and complete information from patients:1,2,6
- Questions related to how patients’ cultural backgrounds are related to health beliefs and how they may influence dental hygiene interventions or recommendations. These questions allow patients to supply answers based on their unique perspectives and backgrounds. Dental hygienists should increase their awareness of and sensitivity toward diverse patient populations and understand culturally influenced health behaviors and attitudes.
- Questions that elicit specific symptoms or signs of a disease, such as “Are you thirsty much of the time?” or “Does your mouth frequently become dry?” Positive answers to these questions could lead to further examination or referrals.
- Questions about specific diseases, such as “Do you have or have you had any of the following diseases or problems?” (eg, diabetes, asthma, or hypertension).
- Questions about diseases specific to certain systems of the human body. These questions may contain references to specific organs.
Aside from asking these types of questions, dental hygienists must also follow an organized process for information gathering and review. The process should help dental hygienists prevent omission of important information. If patients’ responses suggest the presence of risk factors or medical conditions, dental hygienists should ask follow-up questions to determine dates of illness, severity, and outcomes, in addition to consulting and collaborating with patients’ physicians or refering patients to their physicians, if needed. If patients do not have a primary healthcare provider, dental hygienists should advise them to contact their nearest community health center or the public health department. Discussion of patients’ medical history should also be used as an opportunity for dental hygienists to educate patients about the actions they can take to better manage their medical conditions and the consequences of not properly addressing them, including increasing their risk for severe illness from COVID-19.7–12
CHRONIC CONDITIONS AND COVID-19
According to the CDC, six out of 10 US adults have at least one chronic medical condition, and four in 10 have two or more chronic medical conditions. Chronic diseases are defined broadly as conditions that last 1 year or longer, require ongoing medical attention, and/or limit activities of daily living.9 Chronic illnesses, such as heart disease, cancer, and diabetes, are the leading causes of death and disability in the US. Additionally, the more underlying medical conditions people have, the higher their risk of serious illness and negative outcomes.9
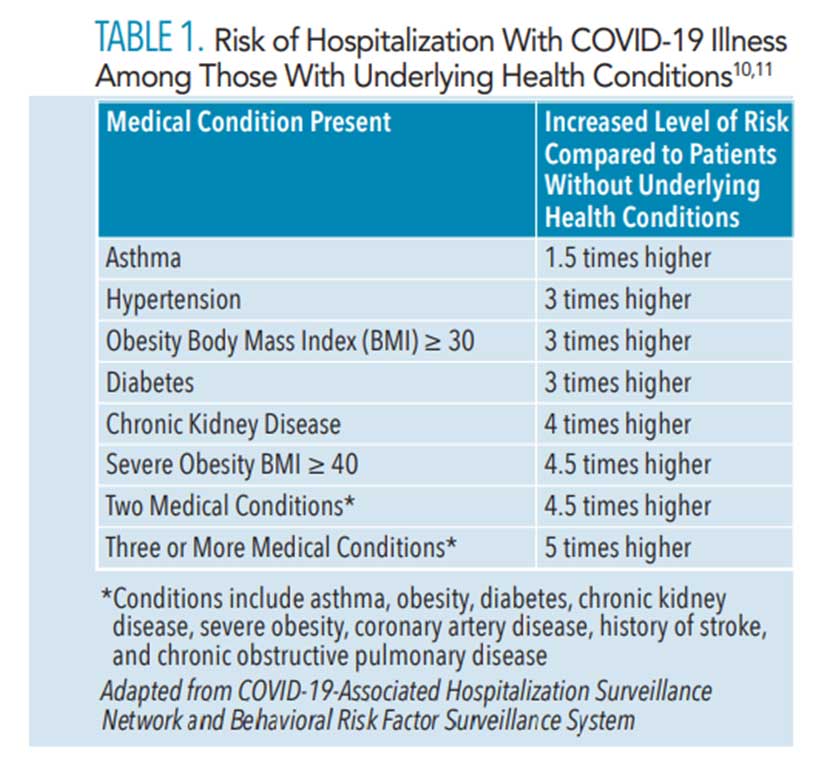
The most common underlying health conditions reported among those with COVID-19 infection in the US are cardiovascular disease (32%), diabetes (30%), and chronic lung disease (18%).7,10,12 As of June 2020, hospitalizations were six times higher and deaths were 12 times higher among those with reported underlying conditions compared to those with no reported health problems.10,12 Table 1 shows the risk for hospitalization among individuals who have select underlying health conditions and become infected with COVID-19 compared to people who do not have any underlying health conditions.
Because dental hygienists see patients with these medical problems on a daily basis, they should use the clinical encounter to educate patients about how they can protect themselves and others from getting COVID-19. Additionally, dental hygienists can stress to patients how important it is to manage their chronic conditions to help prevent severe consequences in the event that they do contract SARS-CoV-2.
![Risk of hospitalization with COVID-19]() DENTAL HYGIENE PRACTICE AND COVID-19
DENTAL HYGIENE PRACTICE AND COVID-19
Considering that dental hygienists see a large number of patients each year —often caring for the same patients twice a year—and conduct medical health histories with these patients, dental hygienists can play a vital role in identifying chronic medical conditions, helping patients seek and receive appropriate medical care for these problems, and educating patients on what they can do to prevent COVID-19 infection. Even though special attention should be given to patients at high risk of complications from COVID-19, all patients should be educated about the importance of taking care of their health and adopting measures to prevent against COVID-19 infection.
Dental hygienists can use the medical history as a starting point to talk to patients about their susceptibility to the virus and how they can protect themselves and others from catching or spreading it. When talking with patients, dental hygienists should stress the link between chronic medical conditions and COVID-19, and remind patients they can reduce their risk for severe complications from the virus by properly managing their underlying conditions.7–12 Patients need to understand that managing their medical conditions includes keeping appointments with their healthcare providers, taking their medications as prescribed, following all nutrition and exercise regimens recommended by their medical providers, and seeking medical attention when feeling sick.9
As efforts to combat the spread of the SARS-CoV-2 virus are constantly evolving, dental hygienists need to stay up to date on evidence-based scientific information about the virus and current CDC guidelines and recommendations surrounding how to avoid contagion and spread. Based on current guidelines, dental hygienists should explain to patients that COVID-19 spreads mainly from person to person, between people who are in close contact with one another, and through respiratory droplets produced when an infected person coughs or sneezes. In addition, patients should be reminded that those infected with the virus (including children) may not show any symptoms. Moreover, dental hygienists should clearly communicate the importance of avoiding close contact with others and keeping a 6-foot distance whenever possible, wearing a mask in public spaces, and maintaining good hand hygiene.15–17 These conversations should be part of regular patient visits as they do not take much time and are in line with the purpose of the medical history, which is to help the dental hygienist provide comprehensive patient care.
In discussing the use of a face mask, dental hygienists need to emphasize that it should be worn in public settings, especially when social distancing is difficult to maintain, but clarify that the mask is not a substitute for social distancing. It is also important to review how to wear a face mask correctly. Following are some recommendations for how to put on and take off a face mask properly:15–17
- Wash your hands with soap and water or use an alcohol-based hand sanitizer before putting on the mask to avoid contaminating your mask.
- Hold the mask by the ear loops or strings and place a loop around each ear or tie the strings behind your head.
- Expand the mask in order to cover both your nose and mouth and secure it under your chin.
- Pinch the bendable piece—if there is one—at the bridge of your nose to secure it.
- Make sure your mask fits snuggly against the sides of your face.
- Remove the mask by grabbing it by the strings or the ear loops to avoid touching the front of the face mask.
- Wash your hands with soap and water or use an alcohol-based hand sanitizer once the face mask is removed.
- Avoid placing a used mask on a bare surface or counter. Instead, place it on a napkin or inside a paper bag.
In regard to maintaining good hand hygiene, dental hygienists should promote washing hands with soap and water as often as possible. Handwashing is especially important after touching items or surfaces that may be frequently touched by other people, such as tables, door handles, electronic cashier registers/screens, and elevator buttons, and before touching the eyes, nose, or mouth. Dental hygienists should also instruct patients to use alcohol-based hand sanitizers that contain at least 60% alcohol when washing hands is not possible.15–17
Following are recommendations on how to keep hands clean:15–17
When using soap and water:
- Wet your hands with clean running water and apply soap.
- Lather your hands with the soap by rubbing them together, making sure the soap covers the back of the hands, between the fingers, under the nails, and over the wrist.
- Scrub your hands for at least 20 seconds.
- Rinse your hands thoroughly with clean running water.
- Dry your hands using a clean towel or air dry them.
When using hand sanitizer:
- Apply the hand sanitizer to the palm of one hand.
- Lather your hands by rubbing them together, making sure the hand sanitizer covers the back of the hands, between the fingers, under the nails, and over the wrist.
- Continue rubbing until hands are dry. Do not dry them with a paper towel or air dry.
SUMMARY
Because COVID-19 is a novel disease that is not fully understood and due to the fact that certain locations are experiencing a second wave of increased cases, all healthcare providers need to monitor pandemic trends and identify groups at risk for infection and severe outcomes. Considering that patients often see their oral health professional much more frequently than they see their physicians, initiating ongoing conversations with patients concerning preventive behaviors related to COVID-19 is critical. The medical history portion of the patient visit provides clinicians with an opportunity to identify medical conditions and risk factors that can put patients at greater risk for the virus and to talk to patients about how they can protect themselves and others. Oral health professionals should use the medical history as a tool to help protect patients and potentially save lives during these uncertain times.
![]() REFERENCES
REFERENCES
- Boyd LD, Mallonee LF, Wyche CJ, eds. Wilkins’ Clinical Practice of the Dental Hygienist. 13th ed. Burlington, Massachusetts: Jones & Bartlett Learning, LLC; 2020.
- Bowen DM, Pieren JA. Darby ML, Walsh P. Dental Hygiene: Theory and Practice. 5th ed. St Louis: Saunders Elsevier; 2020.
- Jemin K, Salomo A. Periodontal disease and systemic conditions: a bidirectional relationship. Odontology. 2006;94:10–21.
- Bui FQ, Almeida-da-Silva CLC, Huynh B, et al. Association between periodontal pathogens and systemic disease. Biomed J. 2019;42:27–35.
- Seitz MW, Listl S, Bartols A, et al. Current Knowledge on correlations between highly prevalent dental conditions and chronic diseases: an umbrella review. Prev Chronic Dis. 2019;16:180641.
- Nield-Gehrig J. Patient Assessment Tutorials. 4th ed. Philadelphia: Lippincott, Williams & Wilkins; 2018.
- United States Centers for Disease Control and Prevention. Evidence used to update the list of underlying medical conditions that increase a person’s risk of severe illness from COVID-19. Available at: cdc.gov/coronavirus/2019-ncov/need-extra-precautions/evidence-table.html Accessed January 22, 2021.
- US Centers for Disease Control and Prevention. People with Certain Medical Conditions. Available at: cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed January 22, 2021.
- US Centers for Disease Control and Prevention. About Chronic Diseases. Available at: cdc.gov/chronicdisease/about/index.htm. Accessed January 22, 2021.
- US Centers for Disease Control and Prevention. COVID-19 Associated Hospitalization Related to Underlying Medical Conditions. Available at: cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-underlying-medical-conditions.htm. Accessed January 22, 2021.
- Ko JY, Danielson ML, Town M, et al. Surveillance Team. Risk Factors for COVID-19-associated hospitalization: COVID-19-Associated Hospitalization Surveillance Network and Behavioral Risk Factor Surveillance System. Clin Infect Dis. 2020:1419.
- Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:759-765.
- Guidelines on the Dental Patient Record. Chicago: American Association of Dental Boards; 2009:4–12.
- Collier A. The management of risk part 3: recording your way out of trouble. Dent Update. 2014;41:338–340.
- US Centers for Disease Control and Prevention. How to Protect Yourself and Others. Available at: cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html Accessed January 22, 2021.
- US Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Available at: cdc.gov/coronavirus/2019-ncov/index.html. Accessed January 22, 2021.
- American Dental Hygienists’ Association. COVID-19 Updates for Dental Hygienists. Available at: adha.org/covid19. Accessed January 22, 2021.
From Dimensions of Dental Hygiene. February 2021;19(2):40-43.