Current Concepts In Esthetic Crown Lengthening
Esthetic periodontal treatment for the “gummy smile.”
The dental hygienist is involved not only in providing therapy to establish and maintain periodontal health but also as an information resource for treatment options. Therapeutic procedures to create an esthetic smile are often presented in the treatment plan. Many patients today want health and function as well as an esthetic smile.
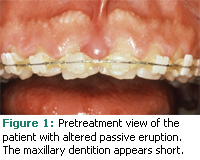
The gingival framework that surrounds the maxillary anterior dentition is part of the esthetics of a smile. Sometimes patients present with a large gingival framework and clinically short teeth in an occlusal-apical dimension. This condition is referred to as the “gummy smile” (see Figure 1).1 In circumstances where a gummy smile is not due to attrition (ie, occlusal wear from grinding the anterior dentition), this excessive display of gingival tissues is classified as a mucogingival deformity and may be the cause for the appearance of short clinical crowns.2
Aside from medications that cause gingival overgrowth or skeletal variations and lip position during smiling, the teeth may appear short simply because the free gingival margin is significantly coronal to the cemento-enamel junctions (CEJs) of the maxillary anterior dentition. This condition results in excessive display of gingival tissues and is called delayed passive eruption or altered passive eruption.3,4
EXCESSIVE GINGIVAL DISPLAY
Many factors may contribute to the manifestation of excessive gingival display. One factor is the position of the upper lip when a patient smiles. The maxillary lip position varies from individual to individual. Typically, the location of the lip during smiling is described as a high, medium, or low lip line.
A high lip line may result in the appearance of the gummy smile simply because so much tissue is visible. Furthermore, there may be a skeletal component relative to the maxilla and mandible that contributes to this appearance. An excessive vertical component to the maxilla in conjunction with a short upper lip may contribute to the appearance of a considerable amount of soft tissue during smiling. Treatment of these cases may require significant orthognathic surgery or plastic surgery of the upper lip.5
DELAYED PASSIVE ERUPTION
Active eruption is the migration or displacement of the dentition through the alveolar bone and the gingival tissues into the oral cavity and toward the occlusal plane. The anatomic crown is the portion of the tooth coated with enamel that terminates at the CEJ. The clinical crown is the portion of the tooth that is coronal to the free gingival margin. Typically at the completion of active eruption, a portion of the anatomical crown is still subgingival.6
Passive eruption does not involve any continued tooth displacement but relates to the continued apical migration of the gingival tissues and associated supracrestal attachment apparatus, which results in further exposure of the enamel of the crown. Gargiulo et al reported about the measured dimensions of the supracrestal attachment apparatus, also known as the dentogingival junction, during the four stages of passive eruption in 1961.7 They noted that the dentogingival junction was composed of a junctional epithelium and a connective tissue attachment both averaging 1 mm in length. These two segments of the dentogingival junction are called the biologic width and average 2 mm in length.8 The biologic width in conjunction with the unattached gingiva associated with the sulcus is referred to as the supraosseous gingiva.9
Initially, the junctional epithelial segment of the attachment is completely on enamel. In the fourth and final stage of passive eruption, the junctional epithelial segment of the attachment is completely on the root surface. At the final stage of passive eruption, the free gingival margin approximates the level of the CEJs and the anatomical crown is completely exposed.
Delayed passive eruption was first described by Coslet et al in 1977 as an anatomical variation resulting in the display of excessive gingiva during smiling.10 The free gingival margin was located significantly coronal to the CEJ of the dentition simply because passive eruption had not been completed.
WIDTH OF GINGIVAL DIMENSION AND BONE CREST
Coslet et al described a 2-part classification system of delayed passive eruption as involving two parameters both relating to the periodontal soft and hard tissues. The first is the occlusal-apical width of the gingiva and the second is the location of the osseous crest. Both play critical roles in how to predictably treat delayed passive eruption.
Classification 1 refers to a variation in which the gingival tissues covering enamel extend apically, resulting in a wider dimension of gingiva. Classification 2 refers to a variation in which the gingival tissues covering the enamel terminate at the CEJ, resulting in a narrow dimension of gingiva. In this second classification, all of the gingiva is located on the anatomic crown.
The location of the osseous crest is the subclassification A or B. In subclassification A, the bone is located 1.5 mm or more apical to the CEJ. In subclassification B, the osseous crest is directly adjacent to the CEJ or no more than 1.5 mm apical to the CEJ.
 The clinical manifestation of any of these classifications is that the teeth appear short. The reality is, however, the teeth are not short but rather a significant amount of enamel is covered with excess gingival tissue. In other words, the clinical crown length—the distance between the incisal edge and the free gingival margin—is much shorter in occlusal-apical length than the anatomical crown length, which is the distance between in cisal edge and the CEJ.
The clinical manifestation of any of these classifications is that the teeth appear short. The reality is, however, the teeth are not short but rather a significant amount of enamel is covered with excess gingival tissue. In other words, the clinical crown length—the distance between the incisal edge and the free gingival margin—is much shorter in occlusal-apical length than the anatomical crown length, which is the distance between in cisal edge and the CEJ.
Average incisal-apical crown lengths for maxillary central incisors and canines range between 11 mm to 13 mm. Average incisal-apical crown lengths for maxillary lateral incisors range be tween 9 mm to 10 mm.11 If a patient’s maxillary anterior dentition does not have incisal-apical measurements similar to these averages, and incisal wear is not evident due to attrition, the patient may have delayed or altered passive eruption.
EVALUATION OF TOOTH LENGTHS
During an examination, the dental hygienist can measure the occlusal-apical lengths of the maxillary anterior clinical crowns by placing the tip of a periodontal probe at the most apical location of the free gingival margin on the facial aspect of the maxillary anterior tooth, and then measure the distance from that point to the incisal edge. If the measured occlusal-apical lengths do not fall within average lengths, the patient may have delayed passive eruption.
To further characterize the patient’s clinical manifestation of short teeth, the patient history should be reviewed to rule out medications that may result in drug-induced gingival overgrowth. In addition, incisal wear must be evaluated as this can also result in short clinical crowns.
Evaluation of the patient’s radiographs is another component to diagnosing delayed passive eruption. The incisal edge of the tooth as well as the mesial and distal termination of the enamel coated portion of the tooth can be seen on a radiograph (ie, the proximal CEJs).
By placing a periodontal probe adjacent to the distal aspect of an incisor on a periapical radiograph and measuring the distance between the radiographic CEJ and the incisal edge, an approximate anatomical tooth length can be determined. Measurements on a digital periapical radiograph can be made in a similar manner. If the distance from the distal CEJ to the incisal edge is still less than average, these radiographic findings may corroborate the diagnosis of incomplete passive eruption.
TREATMENT OPTIONS
Treatment of this condition and exposure of the complete anatomical crown can be achieved by gingivectomy with a scalpel, laser,12 or electro-surgery. Another option is to elevate a flap and position the existing gingival tissues to approximate the level of the CEJ. A flap may need to be elevated to gain access to the bone crest. This would be done in order to alter the position of the bone to a more apical level relative to the CEJ.13,14
Patients may be afraid of looking worse post-treatment because of the possibility of gingival recession. They may also be concerned about whether this type of surgery is predictable and if the tissue will grow back. The answers to these important patient concerns are based on whether the patient presents with a wide or narrow zone of gingiva, and whether the osseous crest is within close proximity to the CEJs of the affected maxillary anterior dentition.
Regarding post-operative gingival recession, the width of gingiva present prior to the surgery will determine the type of procedure that can expose the anatomical crowns without inadvertently exposing the root surfaces. If a patient has a narrow dimension of gingiva, the dentist will apically position the entire width of gingiva, preserving the gingival tissue. If a patient has a wide dimension of gingiva, the dentist may be able to just remove the excess tissue, resulting in a simple exposure of the affected dentition.
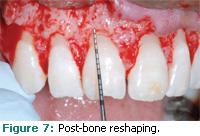
Regarding the concern of the tissue growing back, the relationship between the bone and the CEJ needs to be examined. If the bone crest is close to the CEJ of the affected teeth, the dentist will need to reshape the bone so the osseous crest is 3 mm away from the CEJ. The bone will have a scalloped appearance at the completion of the procedure. The proper visualization of the bone via a flap and appropriate bone resection will prevent rebound of the tissue from occurring. If the bony tissues are not properly resected, the gingiva may grow back.
In the case of a wide dimension of gingiva, described as a 1A or 1B Coslet classification, a margin of gingival tissue could be excised via gingivectomy resulting in a new gingival margin that approximates the CEJ. For this treatment to be predictable, the position of the bone must be evaluated. This can be accomplished via bone sounding after the patient is anesthetized.
If the bone is within close proximity to the CEJ, a flap should be elevated in order to better visualize the bone for resection so a new bone crest can be established 3 mm from the CEJs. The gingival flap could then be positioned either at the osseous crest or at the CEJ. Typically the surgical flap margin is placed approximating the CEJ.
 |
 |
During the healing process, a new dental gingival attachment apparatus will form. Wound healing studies by Lanning et al demonstrate that if the flap is positioned at the new osseous crest, a new dimension of supra-osseous gingiva will reform and be at least 3 mm in length.15
Positioning the flap at the CEJ will also allow for reformation of a new dental gingival attachment apparatus. The advantage of this flap design is to compensate for the possibility of post-operative recession. Postoperative to an apically positioned flap, root exposure may occur if the facial bone initially presented with an existing dehiscence on a particular tooth, was overcut during bone recontouring, or if unanticipated resorption occurs.
In the case of a narrow width of gingiva, described as a 2A or 2B Coslet classification, a gingivectomy with any instrument could result in complete excision of the existing dimension of gingiva. Unfortunately, this would result in a mucogingival deformity. In the case of the narrow zone of gingiva, an apically positioned flap positioning the free gingival margin to the level of the CEJ would preserve the entire gingival dimension.
CONTRAINDICATIONS TO TREATMENT
The condition of delayed or altered passive eruption is not a disease process. It is an anatomical variation that occurs in approximately 12% of the adult population.16 Treatment of this condition is for cosmetic purposes only. The dental team should be careful when presenting this therapeutic option to patients.
If patients understand that this is a healthy variation of the supracrestal gingival tissues, they may opt for no treatment. Some will not want to change their appearance based on a dental professional’s view of esthetics and, depending on how the treatment is proposed, they may be offended by the label of “gummy smile.”
TWO CLINICAL CASES
 |
 |
A 29-year-old African-American man presented with excessive gingival display. The patient’s medical history was unremarkable. The patient’s chief concern was the presence of a high frenum as well as the appearance of very short teeth. The patient’s dental history included orthodontic therapy, which was nearing completion at the time of the consultation.
Probing depths were in the range of 1 mm to 2 mm. A very wide dimension of gingiva was noted. A diagnosis of delayed passive eruption was made. The patient was presented with a treatment plan that included excision of excess tissue and a repositioning of the gingival margin to approximate his CEJs. Figure 1 shows the patient’s pre-operative appearance.
Measurements taken on the radiographs of the distance between the incisal edges and the distal CEJ of the maxillary anterior dentition indicated that the anatomical crowns were longer than the clinical crowns. The radiographs also indicated a diastema between teeth numbers eight and nine. The space was closed prior to initiating surgical therapy.
The surgical procedure consisted of an excision of some of the excess tissue and flap elevation to visualize the osseous crest. During surgery, the osseous crest was noted to be approximately 1 mm away from the CEJs of the involved dentition. These findings indicated a Coslet classification 1B.
Using a hand chisel, the bone was resected so that the osseous crest was approximately 3 mm away from the CEJs of the facial aspects of the maxillary anterior dentition. The interdental tissues were not treated as excess tissue. At the completion of the procedure, a flap was positioned to approximate the CEJs. A frenectomy was also provided. Figure 2 demonstrates the exposure of the anatomical tooth structure at the end of the surgical procedure. The sutures were removed after 1 week and the wound healing can be seen in Figure 3.
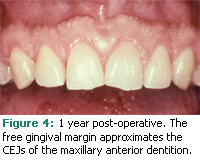
The patient returned for a follow-up evaluation at 3 months, 6 months, and 1 year. The appearance of the patient’s gingival framework relative to his exposed anatomical crowns can be seen in Figure 4.
The second clinical case involves a 19- year-old African-American woman who had completed orthodontic therapy 1 year prior to the periodontal consultation. The patient’s medical history was also unremarkable and she was not taking any medications. Her chief concern was the presence of a “gummy smile.” Clinical evaluation of the patient revealed that probing depths were less than or equal to 3 mm. No gingival inflammation was noted and the patient’s plaque control was good. The diagnosis was delayed passive eruption. The position of the free gingival margin relative to her lip can be seen in Figure 5.
 |
 |
Treatment consisted of an excisional removal of a margin of gingiva through an internal bevel incision. Prior to making the incision, the contours of the CEJs were determined by sounding the CEJs with a periodontal probe. This incision was made on the facial aspects of the maxillary anterior dentition to contour the flap to match the outlines of her CEJs. The interdental papilla tissues were not removed.
During subsequent flap elevation, it was noted that the osseous crest was within close proximity to the CEJs of most of the maxillary anterior affected teeth. The close proximity of the bone to the CEJ of tooth number eight can be seen in Figure 6. Using bone resection techniques, the osseous crest was recontoured so that it was 3 mm apical to the CEJs of the maxillary anterior dentition. At the end of the procedure, the bone had a scalloped appearance that reflected the contours of the flap as well as the twodimensional scalloped appearance of the CEJs. Figure 7 shows the new bone crest level associated with tooth number eight, which is 3 mm apical to the CEJ.
Figure 8 is a 6-month follow-up photograph. A more esthetic gingival framework now surrounds the maxillary anterior dentition. In addition, the upper lip rests just slightly coronal to the free gingival margin associated with the maxillary central incisors and canines.
SUMMARY
Delayed passive eruption can result in excessive gingival display. This is not a disease process but rather a variation of healthy anatomy. As the maxillary anterior teeth may appear short, surgical procedures can increase clinical crown length. This will provide a more esthetic manifestation of the gingival framework that surrounds the anatomical crowns associated with maxillary anterior dentition.
Discussing treatment options with patients should help assuage their fears about the proposed therapy. In addition, the dental team must be aware that not all patients who have this condition will want therapy. It is important to consider patients’ needs and desires when developing the optimal treatment.
REFERENCES
- Levine RA, McGuire M. The diagnosis and treatment of the gummy smile. Compendium Contin Educ Dent. 1997:18:757-762
- Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontal. 1999;44:1-6.
- Evian CI, Cutler SA, Rosenberg ES, Shah RK. Altered passive eruption: the undiagnosed entity. J Am Dent Assoc. 1993;124:107-110.
- Volchansky A, Cleaton-Jones P. Clinical definition of altered passive eruption. Br Dent J. 1979;147:292.
- Garber DA, Salama M. The aesthetic smile: diagnosis and treatment. Periodontol 2000. 1996;11:18-28.
- Bhaskar SN, ed. Orban’s Oral Histology. 8th ed. St. Louis: Mosby Co; 1976.
- Gargiulo AW, Wentz FM, Orban B. Dimensions and relations of the dentogingival junction in humans. J Periodontol. 1961;32:261-267.
- Ingber JS, Rose LF, Coslet JG. The “biologic width”— a concept in periodontics and restorative dentistry. Alpha Omegan. 1977;70:62-65.
- Perez JR, Smukler H, Nunn ME. Clinical dimensions of the supraosseous gingivae in healthy periodontium. J Periodontol. 2008;79:2267-2272.
- Coslet JG, Vanarsdall R, Weisgold A. Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adult. Alpha Omegan. 1977;70: 24-28.
- Nelson SJ. Wheeler’s Dental Anatomy, Physiology and Occlusion. 9th ed. Philadelphia: Elsevier Publishing; 2010.
- Russo J. Periodontal laser surgery. Dent Today. 1997;16:80-81.
- Allen EP. Surgical crown lengthening for function and esthetics. Dent Clin North Am. 1993;37:163-179.
- McGuire MK. Periodontal surgery. Dent Clin North Am. 1998;42:411-465.
- Lanning SK, Waldrop TC, Gunsolley JC, Maynard JG. Surgical crown lengthening: evaluation of the biological width. J Periodont. 2003;74:468-474.
- Volchansky A, Cleaton-Jones P, Fatti LP. A 3-year longitudinal study of the position of the gingival margin in man. J Clin Periodontol. 1979;6:231–237.
From Dimensions of Dental Hygiene. October 2009; 7(10): 24-26, 28, 30.