
Combat Antibiotic Resistance
This growing problem needs to be addressed across all health care fields.
As important members of the health care team, dental professionals must have a general understanding of what is happening in the microbial world. Novel viruses and bacteria can emerge at any time, and may pose a risk for health care providers. The most recent outbreak of Ebola in West Africa, which then appeared in the United States, is an example of how pathogens can impact public health.1,2

FROM THE CENTERS FOR DISEASE CONTROL AND PREVENTION REPORT ANTIBIOTIC RESISTANCE THREATS IN THE UNITED STATES, 2013
In the dental setting, a variety of patients is seen on a daily basis, and it’s impossible to know which microorganisms may accompany them to the dental chair. Health histories provide self-reported pictures of patients’ current health status, but their accuracy cannot be guaranteed. A comprehensive review of patients’ health histories prior to providing treatment is critical. Patients may not report certain conditions due to the stigma attached to the problem or because they don’t think it’s important. Standard precautions should always be implemented to reduce the risk of disease transmission, and to protect dental professionals. 3,4
Another threat to effective infection control and the protection of health care workers is antibiotic resistance. At least 2 million people in the US are infected each year with bacteria that are resistant to antibiotics, and 23,000 die as a direct result of these infections.5 More deaths are caused by conditions related to antibiotic-resistant infections.5
Many of these antibiotic-resistant infections are spread through direct or indirect contact, putting oral health professionals at risk. Direct contact means interaction with the microorganisms at their source, such as the oral cavity or the skin.5 Indirect contact occurs when a clinician is exposed to the microorganism through an intermediary item, such as a needle, instrument, piece of equipment, or surface.3
In 2013, the US Centers for Disease Control and Prevention (CDC) released a 114-page report, Antibiotic Resistance Threats in the United States, 2013.6 The report is organized into three sections: the threat of antibiotic resistance, fighting back against antibiotic resistance, and current antibiotic threats in the US.6 In order to effectively protect themselves and their patients, oral health professionals should be familiar with this report and the overall risks posed by antibiotic resistance.
THE RISKS
According to the CDC, the use of antibiotics is the single most important factor leading to antibiotic resistance around the world. Antibiotics are among the most commonly prescribed drugs in medicine, but up to 50% of prescription drugs are not needed.6 The report notes that humans’ exposure to antibiotics is vast, as they are commonly used in food-producing animals to prevent, control, and treat disease, and to promote growth. Drug-resistant bacteria are present in water and animal feces; when used on crops, their spread continues. Once individuals develop these resistant bacteria, they can spread them through direct contact. Figure 1 provides more detail on how antibiotic resistance develops and how it spreads.6
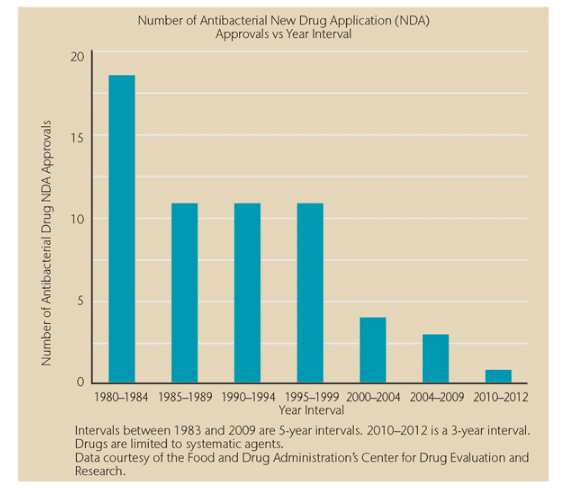
FIGURE 2 FROM THE CENTERS FOR DISEASE CONTROL AND PREVENTION REPORT ANTIBIOTIC RESISTANCE THREATS IN THE UNITED STATES, 2013
THE FIGHT AGAINST ANTIBIOTIC RESISTANCE
The second section of Antibiotic Resistance Threats in the United States, 2013 focuses on the four strategies implemented to battle antibiotic resistance:
- Prevent infections from developing
- Gather data on antibiotic-resistant infections
- Promote antibiotic stewardship
- Develop new antibiotics
To accomplish the second strategy, the CDC is gathering data on antibiotic-resistant infections, including the causes of these infections and the predominant risk factors. Armed with this information, experts can develop specific strategies to prevent antibiotic-resistant infections and resistant bacteria from spreading.6
Promoting the responsible use of antibiotics, or antibiotic stewardship is the third strategy. The CDC reports that health care professionals around the world are increasingly adopting the principles of responsible antibiotic use, including implementing antibiotics only when necessary to treat, and, in some cases, prevent disease; choosing the right antibiotics for the infection at hand; and administering them in the correct manner in every case.6 Effective stewardship ensures that every patient gets the maximum benefit from antibiotics, avoids unnecessary harm from allergic reactions and side effects, and helps preserve the life-saving potential of these drugs for the future.6
The final strategy in the battle against antibiotic resistance is the development of new antibiotics. Because antibiotic resistance is part of a natural evolution, it can be significantly slowed but not stopped. Therefore, new antibiotics will always be needed to keep up with resistant bacteria, as well as new diagnostic tests to track the development of resistance.6 The use of antibiotics became widespread in the 1940s, and it seems logical that new drugs would be introduced each year, but this is not the case (Figure 2).6,7
CURRENT ANTIBIOTIC THREATS
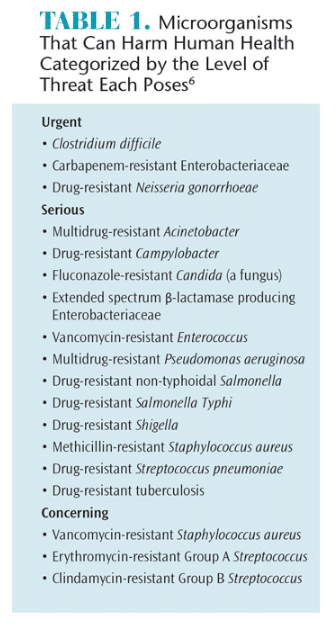
The final section of Antibiotic Resistance Threats in the United States, 2013 lists the current antibiotic-resistant organisms that pose a threat to human health, and categorizes them as urgent, serious, or concerning (Table 1).6 The organisms that pose an urgent threat cause widespread illness and death in patients who acquire the associated infections that often become resistant to nearly all available antibiotics.6 These bacteria require immediate and aggressive action. For example, Clostridium difficile causes life-threatening diarrhea and is passed via contact transmission. Many C. difficile cases occur in patients who have been on prolonged antibiotic therapy.7
Microorganisms characterized as a serious threat necessitate prompt and sustained attention to keep the risks they pose from growing. The label of concerning threat means that the microorganisms need careful monitoring and preventive action to ensure they don’t move into the higher threat levels. The report provides a wealth of information on each of the bacteria included within all three threat categories, including how health care professionals can support the CDC’s efforts to reduce the threat posed by these microorganisms.
CONCLUSION
Oral health professionals need to be aware of antibiotic-resistant organisms and how they can support the battle against them. By keeping up-to-date and supporting the CDC’s strategies to reduce antibiotic resistance, clinicians are protecting their health, as well as the health of their patients.
REFERENCES
- World Health Organization. Ebola Virus Disease. Available at: who.int/mediacentre/factsheets/fs103/en. Accessed December 16, 2014.
- McCoy CE, Lotfipour S, Chakravarthy B, Schultz C, Barton E. Emergency medical services public health implications and interim guidance for the Ebola virus in the United States. West J Emerg Med. 2014;15:723–727.
- Miller CH. Infection Control and Management of Hazardous Materials for the Dental Team. 5th ed. St. Louis: Mosby Elsevier; 2014:19–21.
- Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;52:1–61
- Centers for Disease Control and Prevention. Antibiotic/Antimicrobial Resistance. Available at: cdc.gov/drugresistance/threat-report-2013. Accessed December 16, 2014.
- Centers for Disease Control and Prevention. Antibiotic Resistance in the United States, 2013. Available at: cdc.gov/drugresistance/threat-report-2013. Accessed December 16, 2014.
- Centers for Disease Control and Prevention. Get Smart: Know When Antibiotics Work. Available at: cdc.gov/getsmart/antibiotic-use/antibiotic-resistance-faqs.html. Accessed December 16, 2014.
From Dimensions of Dental Hygiene. January 2015;13(1):44–46,48,50


[…] and their patients, dental teams should be aware of the many symptoms of thrush, and understand how antibiotic-resistant infections are spread through both direct and indirect […]