Caring for Stroke Survivors
Maintaining the oral health of patients who have experienced stroke is critical to supporting their systemic health.
This course was published in the October 2015 issue and expires October 31, 2018. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define stroke and identify its risk factors.
- Discuss the risk of recurrence among stroke survivors.
- Explain the symptoms of stroke and how to respond.
- Identify the components of providing effective dental care to patients who have experienced stroke.
A stroke, or cerebrovascular accident, occurs when there is an interruption of blood, oxygen, and glucose to the brain tissue.1 Stroke is the fifth leading cause of death and the second leading cause of death among older adults in the United States.2 Each year, approximately 795,000 Americans experience a stroke, with 130,000 dying from stroke-related causes.2 Older adults who are stroke survivors have a 50% chance of sustaining moderate to severe disabilities after the incident.2
The interruption of the blood supply to the brain that occurs during a stroke is caused by a blocked vessel (ischemic stroke) or a ruptured vessel (hemorrhagic stroke).3 The prognosis for those experiencing a hemorrhagic stroke is generally poor, with 50% of patients dying after the initial event.4 There are two types of hemorrhagic strokes: intracerebral hemorrhage and subarachnoid hemorrhage. Intracerebral hemorrhage most commonly occurs in vessels of the basal ganglion in which blood leaks into brain tissue, causing increased pressure and damage to the surrounding cells. Hypertension and vessel abnormalities are the main causes of intracerebral hemorrhage. Subarachnoid hemorrhage occurs when blood from a ruptured vessel accumulates between the skull and the brain (subarachnoid space). The main cause of a subarachnoid hemorrhage is a cerebral aneurysm (a weak, bulging spot on an arterial vessel wall). Wear and tear on arteries, injury, infection, and genetics are risk factors for a cerebral aneurysm.4 Approximately 85% of strokes are classified as ischemic and are subcategorized into thrombotic (blood clot forms in the vessels that supply blood to the brain) or embolic (blood clot forms away from the brain, breaks free, and travels to block a vessel that provides blood to the brain).3 Thrombotic strokes can occur in large or small vessels.4 Long-term plaque build-up and clot formation are the cause of large vessel strokes, with high cholesterol being the main contributing factor. Small vessel strokes (lacunar infarctions) occur when blood flow is blocked in distant arterial vessels.4 An embolus consisting of fat globules, air bubbles, or pieces of plaque will float through the bloodstream until it reaches a blood vessel too small for the embolus to pass through. Normal blood perfusion of brain tissue is 60-70mL/100 grams per minute. Because the brain stores little glycogen, if sustained blood flow drops below 25mL/100 grams per minute, irreversible brain damage will result.5
RISK FACTORS
Modifiable risk factors for stroke include: being overweight, physical inactivity, heart disease, diabetes, high cholesterol, heavy drinking, hypertension, tobacco or methamphetamine use, and active periodontal disease. Nonmodifiable risk factors include a family history of stroke, gender, race, and age.1–3 According to the American Heart Association, the prevalence of a first stroke is nearly twice as high for blacks as for whites and blacks are more likely to die from a stroke.2 Other high-risk groups include American Indians and Native Americans. It is projected that by 2030, 3.4 million individuals older than 18 will have experienced a stroke, representing a 20.5% increase from 2012.2 According to death certificate data, the mean age for stroke-related death in the United States is 791?2.2 Approximately 77% of those who have their first stroke had blood pressure higher than 140/90 mmHg. For each additional 10 mmHg, the incidence increased by 8% for whites and 24% for blacks.2 Reducing systolic blood pressure to measure below 130 mmHg decreases stroke risk by 20%.2
Impaired blood glucose levels double the risk of stroke, and triples the risk if the individual also has diabetes mellitus. Atrial fibrillation (abnormal heartbeat) is another risk factor for stroke, increasing the incidence approximately fivefold for all age groups. Smokers are two times to four times more likely to experience stroke than nonsmokers. There is a 25% higher risk for stroke in patients who are older than 65 and have a family history of the disease, compared to 7.5% in patients with no family history of stroke. The risk for stroke was found to be five times higher in patients undergoing dialysis compared to the general population.2
DIAGNOSIS AND TREATMENT
Strokes are officially diagnosed through laboratory tests, diagnostic imaging, electrocardiograms, and echocardiograms. These tools are used to determine the location and severity of an event and evaluate the status of the heart to determine future stroke potential.3,4 Treatment occurs in a hospital setting and consists of breaking up the clot or repairing the ruptured vessel with surgery to restore blood flow to the infarcted site.3 Once the patient is stabilized, anticoagulants, antihypertensives, corticosteroids, and antiseizure medications may be used to prevent recurrent stroke symptoms.6
Stroke survivors have a wide variety of prognoses, ranging from no permanent cognitive dysfunction to debilitating impairments in cognition and motor skills.3 Damage and disabilities caused by stroke depend on the location and severity of the incident (Table 1).6 In general, the cerebrum controls speech, emotion, sensory stimuli, and large and fine motor movements, while the cerebellum manages reflexes, balance, and coordination. The brainstem is responsible for the body systems that sustain life, such as breathing, digestion, and heart regulation.6 On average, among patients who survive a stroke, 10% will experience no impairments, 50% will have mild residual disabilities, 15% to 30% will have disabilities and require special services, and 10% to 20% will require institutionalization.4
STROKE RECURRENCE
The highest risk of stroke recurrence occurs during the first week after a transient ischemic attack (TIA) and stroke, but the risk of recurrence remains high for the first year following the incident. Late and early stroke recurrence have similar rates but may have different causes. There is not enough evidence at this time, however, to definitively determine those causes or how to prevent early or late stroke recurrence.7 A retrospective study examined the incidence and predictors of ischemic stroke or recurrent attack during hospitalization for an initial TIA event.8 This study found that 1.7% of patients had an ischemic stroke while in the hospital following TIA and the majority of incidents were from blockage in small vessels.9 The rate of recurrence was correlated with hypertension, history of untreated alcoholism, and hemiparesis.7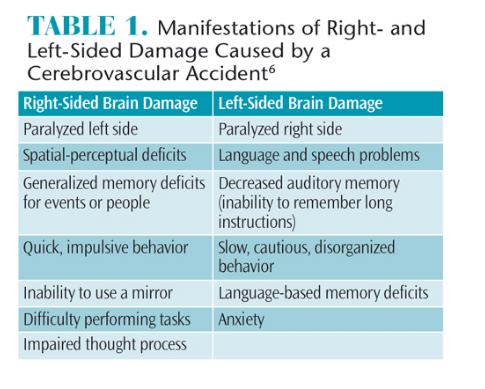
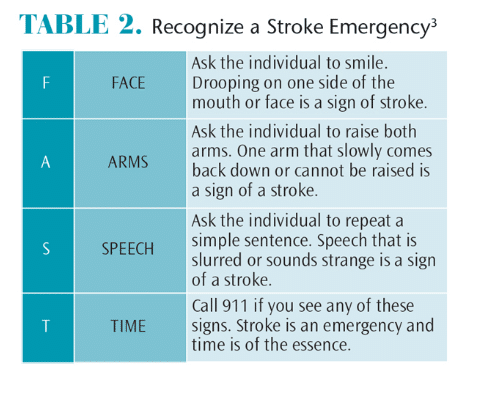
BE PREPARED TO RECOGNIZE A STROKE EMERGENCY
Dental professionals should be trained and prepared to handle a medical emergency, including stroke. Symptoms of a stroke may include: difficulty walking; trouble speaking or understanding speech; paralysis or numbness in the face, arm, or leg; vision problems with one or both eyes; and a sudden severe headache that may be accompanied by dizziness or vomiting.3 If a patient is showing signs of a stroke, seek immediate medical attention. To evaluate for signs of a stroke, remember the acronym FAST: face, arms, speech, and time (Table 2).3 Look for one side of the face drooping when the patient smiles or deviation of the tongue upon extrusion, one arm drifting downward when both arms are raised, slurred or incoherent speech, and time, which is of the essence in getting treatment.3 In order to minimize negative outcomes of a stroke, hospital-based treatment must be initiated within 3 hours of the onset of symptoms.3 While waiting for emergency responders, note the time and signs of stroke and administer oxygen therapy.10
Dental professionals can significantly impact their patients’ health by assessing and referring those who are at elevated risk for stroke. The National Institute of Neurological Disorders and Stroke provides invaluable stroke assessment tools on its website: stroke.nih.gov/materials/brainbasics.htm. High-risk patients should be encouraged to seek medical care and educated about controlling and reducing stroke risk factors.4
PROVIDING DENTAL CARE
The first dental appointment should not be scheduled until 6 months after an initial stroke event (unless emergency treatment is required). At the time of the appointment, a health history update should be obtained, including the date of the stroke, magnitude, treatment, and residual disabilities. Clinicians should identify all medications the patient is taking daily, review recent laboratory tests, and consult with the patient’s physician before treatment. Obtaining the names of caregivers and other health care providers is recommended to promote collaborative care.4 To protect patients’ right of autonomy, dental hygienists should ask for consent to treat from patients, not caregivers. If they are able to understand the consent process, patients should sign their own forms and be involved in the treatment planning process.10 Patients who have hemiparesis might need assistance to get in and out of the dental chair.11 The staff should approach patients with a positive, optimistic attitude so they will feel comfortable and welcome during the visit.12 Individuals who have experienced stroke should be scheduled for morning appointments with at least an additional 15 minutes so they do not feel rushed and enough time is available to provide oral hygiene instructions.13–15
In order to communicate effectively with patients who have experienced a stroke, dental hygienists should speak slowly and exercise patience waiting for a response while they formulate the words.3 When speaking with patients, sit at eye level on their unimpaired side and use slow, deliberate speech.4 Reduce noisy distractions and maintain a smooth routine. Stroke survivors may have aphasia (lack of comprehension), so do not depend on yes or no responses when determining whether they understand.4 Patients may need modified oral hygiene aids and instruction based on their level of cognitive and motor skill abilities. Large handle grips for toothbrushes and floss aids enable patients with limited dexterity to maintain their oral health. Dental hygienists should consider providing care to patients in their place of residence because many stroke survivors are in hospitals or live in long-term care facilities (LTCFs), and arranging transportation to appointments can be difficult.16
Patients who have limitations after a stroke might also experience depression, grief, loss, and feelings of helplessness, which can affect their behavior. Post-stroke depression can cause delays in functional recovery and can lead to an increase in cognitive impairments. Depression can be both physical and psychosocial in origin. It may be caused by elevated levels of pro-inflammatory cytokines due to the ischemia or increased glucocorticoid levels initiated by stress and overactivation of the hypothalamus, pituitary, and adrenal glands. To date, not much is known about effective treatment options for post-stroke depression.15
During the appointment, patient oxygen saturation and blood pressure should be monitored. Blood pressure should not exceed 140/90 mmHg.17 Minimal amounts of anesthetic solution (a cardiac dose) should be used, with low amounts of epinephrine (1:100,000 or 1:200,000) to maintain low blood pressure.6 Many patients will be taking anti-platelet drugs, such as aspirin, clopidogrel, dipyridamole, and ticlopidine, or anticoagulants, including warfarin, dabigitran, apixaban, and rivaroxaban, to prevent stroke recurrence. Anticoagulants are recommended for individuals at elevated risk for stroke and those with atrial fibrillation. When treating patients taking warfarin, International Normalized Ratio (INR) testing should be completed prior to dental hygiene treatment. The INR should be between 1.5 and 3.5 for effective blood coagulation. If it is less than 1.5, consult with the patient’s physician before treatment.17 Avoid using metronidazole and tetracyclines for patients taking warfarin, as the two medications decrease the effectiveness of blood thinning drugs.5 A patient who is taking anticoagulant or antiplatelet medications is at increased risk of bleeding after dental treatment, so nonadrenergic hemostatic agents should be readily available.5,13–15
Extensive bridgework is contraindicated for patients who have experienced stroke. Fixed appliances are favored over removable partial or complete dentures. Patients need to be able to perform adequate oral hygiene, especially on fixed bridge abutments.4 A shorter continuing care interval is usually required for stroke survivors, so self-care efforts can be evaluated and professional prophylaxis can be provided.
Periodontally involved patients who receive appropriate treatment have a lower incidence rate for stroke and recurrence.18 Educating caregivers about their roles in preventing caries and periodontal diseases is crucial for successful treatment outcomes.18 Providing comprehensive and safe care requires screening patients for stroke risk, understanding drug contraindications, reducing stress during the provision of oral health care, maintaining an empathetic approach, and developing an individualized treatment plan.
In one survey, less than half of stroke survivors evaluated had seen a dentist in the year prior to their stroke.19 Women, those who were married, had a high school diploma or higher, and those who visited their physician within the last year were most likely to see a dental provider prior to their stroke. Nationally, 60% of stroke survivors seek dental treatment following the incident.19 The study showed that the presence of significant medical comorbidities was a barrier to dental care and black and Hispanic individuals were less likely to receive professional dental care than whites.19 Preventive care is the most effective way to prevent or reduce the rates of oral and systemic disease. A direct relationship exists between chronic inflammation, cerebrovascular accidents, and atherosclerosis. The immune response triggered by chronic inflammation speeds up the process of atherosclerosis and predisposes individuals to another ischemic attack.19
The cytokine, tumor necrosis factor (TNF), causes apoptosis in cells and is found extensively in cases of periodontal disease.20 TNF is also involved in the pathophysiology of stroke recovery, with high amounts of TNF leading to increased brain dysfunction and decreased recovery rates post-stroke. Decreasing the amount of TNF present in the oral cavity increases cognitive function and recovery rates for stroke survivors.20
CONCLUSION
Maintaining the oral health of individuals who have experienced stroke is paramount to supporting their systemic health and reducing the risk of stroke recurrence. Many individuals remain in hospitals or LTCFs post-stroke and have limited access to professional dental care. Oral hygiene can significantly improve patients’ prognosis for recovery after stroke, as well as their quality of life. In order to meet the oral health needs of this patient population, dental hygienists should consider working in hospitals or LTCFs (where state laws allow). Dental hygienists should also collaborate with nursing staff to educate caregivers on how to properly perform basic oral hygiene tasks. All individuals affected by stroke should be educated on methods of oral hygiene that can be modified for stroke survivors, as well as the important role oral health plays in systemic health and stroke recovery.
REFERENCES
- National Institute of Neurological Disorders and Stroke. Brain Basics: Preventing Stroke. Available at: stroke.nih.gov/materials/brainbasics.htm. Accessed September 11, 2015.
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322.
- Mayo Clinic. Stroke. Available at: mayoclinic.org/ diseases-conditions/stroke/basics/causes/con- 20042884. Accessed September 11, 2015.
- Signorino CS. Stroke: An overview and resources for dental hygienists. Available at: adha.specialissues. cdeworld.com/courses/20206Stroke:An_Overv iew_ and_Resources_for_Dental_Hygienists. Accessed September 11, 2015.
- Fatahzadeh M, Glick M. Stroke: epidemiology, classification, risk factors, complications, diagnosis, prevention, and medical and dental management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:180–192.
- Little JW, Falace DA, Miller CS, Rhodus NL. Dental Management of the Medically Compromised Patient. 8th ed. St Louis: Elsevier Inc; 2013:500–506.
- Sørensen RT, Rasmussen RS, Overgaard K, Lerche A, Johansen AM, Lindhardt T. Dysphagia screening and intensified oral hygiene reduce pneumonia after stroke. J Neuro Nurs. 2013;45:139–146.
- Purroy F, Jiménez Caballero PE, Gorospe A, et al. How predictors and patterns of stroke recurrence after a TIA differ during the first year of follow-up. J Neurol. 2014;261:1614–1621.
- Kelly T. Review of the evidence to support oral hygiene in stroke patients. Nurs Stand. 2010;24:35– 38.
- Lee YL, Hu HY, Huang N, Hwang DK, Chou P, Chu D. Dental prophylaxis and periodontal treatment are protective factors to ischemic stroke. Stroke. 2013;44:1026–1030.
- Bodnar C, Varlan CM, Varlan V, Vaideanu T, Popa MB. Dental Management in Stroke Patients. Available at: tmj.ro/pdf/2008_number_3_4_ 343185458712449.pdf. Accessed September 11, 2015.
- Ovbiagele B, Goldstein LB, Higashida RT, et al. Forecasting the future of stroke in the United States: a policy statement from the American Heart Association and American Stroke Association. Stroke. 2013;44:2261–2375.
- Brady M, Furlanetto D, Hunter RV, Lewis S, Milne V. Staff-led interventions for improving oral hygiene in patients following stroke. Cochrane Database Syst Rev. 2006;4:CD003864.
- Prendergast V, Kleiman C, King M. The bedside oral exam and the barrow oral care protocol: translating evidence-based oral care into practice. Intensive Crit Care Nurs. 2013;5:282–290.
- Li W, Ling S, Yang Y, Hu Z, Davies H, Fang M. Systematic hypothesis for post-stroke depression caused inflammation and neurotransmission and resultant on possible treatments. Neuro End Lett. 2014;35:104–109.
- Dickinson H. Maintaining oral health after stroke. Nurs Stand. 2012;26:35–39.
- Beall A. Dental management and care of the stroke survivor. Access. 2014:9–13.
- The Stroke Center at University Hospital. Risk Factors: Brain Anatomy. Available at: uhnj.org/stroke/types.htm. Accessed September 11, 2015.
- Sanossian N, Gatto NM, Ovbiagele B. Subpar utilization of dental care among Americans with a history of stroke. J Stroke Cerebrovasc Dis. 2011;20:255–259.
- Ignatowski T, Spengler RN, Dhandapani KM, Folkersma H, Butterworth RF, Tobinick E. Perispinal etanercept for post-stroke neurological and cognitive dysfunction: scientific rationale and current evidence. CNS Drugs. 2014;28:679–697.
From Dimensions of Dental Hygiene. October 2015;13(10):57–60.



