Anatomy of a Stroke
Building the foundation for effective therapy and good ergonomics.
In the course of a busy day treating patients, attention is rarely focused on the composition and character of a working stroke. Something as automatic as hand instrumentation may not merit scrutiny after years of clinical practice. But following the correct instrumentation fundamentals and principles in each placement and activation directly correlates to the efficacy of the dental hygienist’s efforts to treat periodontal infection.
In light of the growing body of evidence linking oral and systemic health, the dynamics of an effective stroke are worth revisiting—not only to support the goals of nonsurgical therapy but for secondary benefits to the clinician. These benefits include conserving effort, increasing  efficiency, and lowering risk of work-related musculoskeletal disorders (WMSD), such as repetitive strain injury (RSI) and carpal tunnel syndrome (CTS).
efficiency, and lowering risk of work-related musculoskeletal disorders (WMSD), such as repetitive strain injury (RSI) and carpal tunnel syndrome (CTS).
Basics Revisited
The principles of adaptation, angulation, and stroke activation are vital to effectiveness with hand instrumentation. Every practitioner can recall a clinical instructor imprinting these concepts in school, but students are not equipped to appreciate them when they are first introduced. Properly applied, principles form the basis for efficiency and effectiveness in nonsurgical therapy while also playing a critical role in ergonomic protection of the clinician.
Adherence to adaptation, angulation, and activation can spell the difference between chronic, continuous infection and healing. Burnished calculus left behind from misunderstanding or misapplication of principles is not the harmless entity previously believed.1 Endoscopy has clearly established that every incident of post-therapeutic bleeding on probing corresponds to burnished calculus left behind on the root surface.2 Mineralized and highly porous, these remnants of partially scaled deposit serve as the ideal reservoir for pathogenic biofilm, thus permitting the infection to continue as evidenced by the ulcerated lesion overlying each speck of burnished calculus. These soft tissue lesions mimic the shape of the residual deposit they cover in mirror image, leaving little doubt as to the origin of their presence. Removing this reservoir for biofilm—the burnished calculus—allows the soft tissue lesion to heal, resolving local infection.3
Beyond the scope of therapeutic effectiveness for the patient’s health is the issue of ergonomics for the practitioner’s health—to prevent WMSD and promote a long and satisfying career.4 The single most important tool to guard against neuromuscular injury may be to self-monitor and self-correct the deeply ingrained negative habits established over the course of clinical work. Statistics are dismal for dental practitioners suffering occupational injury, which is all the more reason to pursue an aggressive program of awareness and prevention.5,6
 Post-graduate hands-on instrumentation courses taught by experienced clinical educators who specialize in periodontal therapy are perhaps the best investment that can be made in a career. Practitioners should be selective in choosing quality courses that teach critical aspects of hand instrumentation. Advanced hands-on instruction should include essential components of ergonomic practice that can promote health/career longevity. Just like the well-intentioned patient who for years has incorrectly brushed and now has serious localized disease, it can be a rude awakening to find that a particular instrumentation technique has needlessly placed a practitioner at risk for occupational injury.
Post-graduate hands-on instrumentation courses taught by experienced clinical educators who specialize in periodontal therapy are perhaps the best investment that can be made in a career. Practitioners should be selective in choosing quality courses that teach critical aspects of hand instrumentation. Advanced hands-on instruction should include essential components of ergonomic practice that can promote health/career longevity. Just like the well-intentioned patient who for years has incorrectly brushed and now has serious localized disease, it can be a rude awakening to find that a particular instrumentation technique has needlessly placed a practitioner at risk for occupational injury.
Truth or Consequences
 The formation of a working stroke starts with a relationship between the instrument and the tooth. The first component is blade placement, which takes into account adaptation and angulation. The second component is activation or the movement of the blade over the tooth. Activation must sustain the tooth-to-blade angle (Figure 1) throughout instrument movement—from the start of the stroke to its end point.
The formation of a working stroke starts with a relationship between the instrument and the tooth. The first component is blade placement, which takes into account adaptation and angulation. The second component is activation or the movement of the blade over the tooth. Activation must sustain the tooth-to-blade angle (Figure 1) throughout instrument movement—from the start of the stroke to its end point.
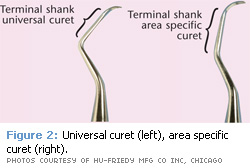
The terminal shank (Figure 2) provides visual guidance to set proper angulation for a working stroke and ensures the activation remains true to this angle relationship. Activations that modify this angle relationship can carry significant consequence. Blade closure (Figure 3B) burnishes the deposit onto the root. Opening the blade (Figure 3C) makes the smooth side or back of the curet compress the deposit, while also compromising control and risking trauma to the tissue. Both errors burnish (Figure 3D).
Vertical strokes that cause the handle of the instrument to move back and forth should be analyzed to determine if there is blade closure or opening. Movement in a plane parallel to the surface being instrumented, such as wrist rock activations, will not be problematic. If the plane of movement is perpendicular to the surface being instrumented, the tooth-to-blade orientation will be altered and the stroke compromised. The shank of the instrument should maintain the same relationship to the tooth surface from the onset of the stroke to its finish in a vertical pull stroke. In this way, working angulation is preserved for an effective and efficient stroke.7
Positioning Details
Blade-to-shank orientation of area specific curets differs from that of universal curets and these instruments must be positioned for activation according to their design. With the offset blade of a Gracey curet, establishing angulation for a working stroke is a matter of keeping the terminal shank parallel to whatever surface is being instrumented, regardless of which Gracey curet is used (Figure 5). However, universal curet blades are set at a 90° angle to the terminal shank. A parallel orientation of shank to surface sets the face of the universal blade perpendicular to the surface (Figure 6A). To establish working angulation of 70°, the universal shank must therefore close 20° toward the surface (Figure 6B).
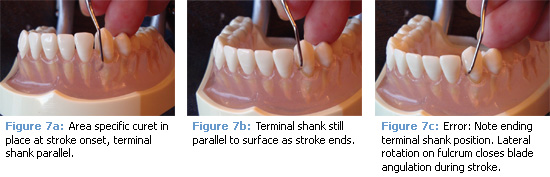
Once the terminal or toe-third of the blade is applied for correct adaptation, the instrument’s terminal shank provides visual cues to guide effective blade angulation. Since the blade cannot be observed once it is within the pocket, shank positioning and guidance are critical to establishing effective working angulation (Figure 7). The shank-tosurface orientation for either the area specific or the universal curet is maintained from stroke onset to completion, making each stroke perform to its maximum potential.
Proper angulation and stroke activation are major components of effective instrumentation that can prevent burnishing while increasing efficiency and conserving effort—all part of sound ergonomic practice. Devote the time to self-monitor and correct the common errors that sabotage therapeutic goals. Seek quality hands-on clinical coursework that supports professional development and injury prevention. These measures are worthwhile endeavors for the health and well being of practitioners as well as their patients.
 References
References
- Fujikawa K, O’Leary TJ, Kafrawy AH. The effect of retained subgingival calculus on healing after flap surgery. J Periodontol. 1988;59:170-175.
- Pattison A, Pattison G. Periodontal instrumentation transformed. Dimensions of Dental Hygiene. 2003;1(2):18-20, 22.
- Stambaugh RV. Perioscopy—the new paradigm. Dimensions of Dental Hygiene. 2003;1(2):12-15.
- Liskiewicz ST, Kerschbaum WE. Cumulative trauma disorders: an ergonomic approach for prevention. J Dent Hyg. 1997;71:162-167.
- Michalak-Turcotte C: Controlling dental hygiene work-related musculoskeletal disorders: the ergonomic process. J Dent Hyg. 2000;74:41-48.
- Valachi B, Valachi K. Mechanisms leading to musculoskeletal disorders in dentistry. J Am Dent Assoc. 2003;134:1344-1350.
- Matsuda SA. Instruments and principles for instrumentation. In: Clinical Practice of the Dental Hygienist. 10th ed. Baltimore, Md: Lippincott Williams and Wilkins; 2009.
From Dimensions of Dental Hygiene. November 2008; 6(11): 22, 24, 26.