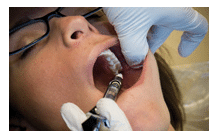
Alternative Anesthesia Techniques
When administering anesthesia to patients with anatomical variations, the Gow-Gates and Vazirani-Akinosi mandibular blocks may provide the best opportunity for successful pain control.
This course was published in the September 2015 issue and expires September 30, 2018. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe the causes of mandibular anesthesia failure.
- Discuss indications and contraindications for the Gow-Gates (GG) and Vazirani-Akinosi (VA) mandibular nerve blocks.
- Explain how to safely and effectively perform both GG and VA mandibular nerve blocks.
Most practitioners who provide local anesthesia encounter difficulty achieving adequate pain relief at some point. This is especially true for mandibular block anesthesia. Failure to achieve anesthesia may be due to a host of factors, ranging from operator-dependent to patient-dependent to a combination of both. Examples of operator-dependent factors include inappropriate choice of injection or anesthetic solution and/or poor technique. Patient-dependent factors include anatomical variation, pathological conditions such as infection, and psychological factors such as dental fear and anxiety.1
Anatomical differences between patients can make the delivery of anesthesia challenging. Mandibular anesthesia, specifically the traditional inferior alveolar (IA) nerve block, is the least reliable in achieving excellent pain control in dental local anesthesia. With variable rates of success (failure rates range from 31% to 81%),2 the IA is frequently impacted by anatomical variation. The most common anatomical factors that inhibit the success of mandibular anesthesia include deposition of solution below the level of the mandibular foramen, inconsistent intraoral landmarks, presence of supplementary innervation commonly provided by the mylohyoid and auriculotemporal nerves, and variation in height, width, and flare of the ramus.2–4
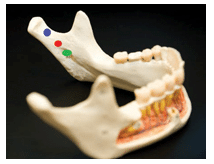
To address the relatively unpredictable success of mandibular anesthesia, two alternative mandibular blocks are available: the Gow-Gates (GG) mandibular block and the Vazirani-Akinosi (VA) mandibular block. The VA will anesthetize more structures innervated by the mylohyoid nerve than the IA, and the GG will anesthetize more structures innervated by the mylohyoid, auriculotemporal, and buccal nerves than the VA. The target sites for deposition vary in height on the condyle and the mandibular (V3) branch of the trigeminal nerve. The GG is highest (near the neck of the mandibular condyle), and the deposition site for the VA sits at an intermediate position between the GG and IA. Branches of V3 (lingual, buccal, IA, mylohyoid) stem from the main trunk as the nerve progresses inferiorly after exiting the foramen ovale. Thus, the higher the location of the injection, the greater number of branches will be anesthetized. Figure 1 provides a comparison of target sites for the IA, GG, and VA.5,6
While the GG and VA injections are simple to administer and provide profound pain relief, some clinicians may be unfamiliar with these alternatives to more traditional approaches to local anesthesia. The following section will present information specific to each injection, as well as detailed technique instructions and clinical photos.
GOW-GATES INJECTION
The GG injection is considered a true mandibular block that anesthetizes all oral structures of the mandible on the side in which the injection is administered. It has several advantages when compared to the traditional IA nerve block, including a higher success rate; lower incidence of positive aspiration (2% compared to 10% to 15% with the IA); and complete anesthesia of structures.2,7,8 This injection provides a wider area of anesthesia than a traditional IA because the anesthetic is delivered at the neck of the condyle on the mandibular ramus, which is superior to the branching of the mylohyoid, buccal, and lingual nerves. By anesthetizing the large mandibular nerve trunk (commonly referred to as V3), all mandibular structures are anesthetized.
1. Indications for Use
The GG injection can be used anytime mandibular anesthesia is required for multiple areas in the arch and for quadrant dentistry, but it is particularly helpful in cases when an IA injection results in incomplete or inadequate anesthesia. In addition, the GG anesthetizes all soft tissues in the quadrant, which is ideal for periodontal therapy procedures.
2. Contraindications
- Infection in the area of injection is a general contraindication of local anesthesia because advancing a needle through an area of infection can cause it to spread. Additionally, it is very difficult to achieve anesthesia in areas of infection due to the inflamed tissue’s low pH, as well as increased vascularity and inflammation.
- Patients who are unable to open their mouths widely (the mouth must remain open for the duration of the injection and for 1 minute to 2 minutes post injection, for a total of about 2 minutes to 3 minutes)
- Patients at risk of post-procedural trauma due to numbness, such as young children and patients with physical and developmental disabilities
3. Special Considerations
- The time required to achieve complete anesthesia with the GG is longer than a traditional IA injection. The clinician should wait a minimum of 5 minutes after administration to allow for complete penetration of the anesthetic into the nerve.2
- Compared to other injections, there is a steeper learning curve with the GG technique. This injection is not simply a “high IA,” but necessitates a different approach altogether. Some seasoned practitioners find the technique frustrating. Once clinicians gain experience in administering the GG injection, they should achieve higher success rates compared to the IA injection.2
4. Areas Anesthetized
- Mandibular teeth to the midline
- Buccal periosteum and soft tissues
- Lingual periosteum and soft tissues
- Anterior two-thirds of the tongue and the floor of the mouth
- Inferior portion of the ramus and the body of the mandible
- Facial skin in the zygomatic, buccal, and temporal regions
5. Technique
- Needle selection: a 25-gauge long needle is recommended for this injection. In addition to posing less resistance to aspiration, the 25-gauge needle is less likely to deflect as the clinician progresses through muscular tissues to the deposition site.9 While rare, the use of a thin needle (smaller gauges of 27 and 30) on a mandibular injection can contribute to needle breakage.10
![]()
FIGURE 4. This is the final position for deposition of local anesthetic for the Gow-Gates injection. - Identify the penetration site, which is just distal to the maxillary second molar, at the height of the mesiolingual cusp tip of the maxillary second molar (Figure 2).
- Prepare the tissues for the injection by applying a topical anesthetic.
- Establish the angle of the syringe, which should be along a line that connects the corner of the patient’s mouth to the tragus of the ear on the side to be anesthetized (Figure 3). This extraoral guideline can be difficult to judge when looking at the tissues intraorally. Placing a finger just inside the patient’s ear on the inter-tragic notch (tell the patient first) provides a visual target during the injection (Figure 3 and Figure 4). The barrel of the syringe should be in the corner of the patient’s mouth on the contralateral side, typically above the canine premolar area. This angle may vary depending on the degree to which the tragus diverges from the ear, resulting in a possible correct position as far anterior as the mesial of the canine or as far posterior as the distal of the second premolar. Generally, the more flat a tragus lies in relation to the face, the more anterior the barrel position will be (toward the canine). Conversely, the closer the tragus is to a 90° angle with the face, the more posterior the barrel position should be (toward the second premolar).
- Penetrate and advance to the site of deposition. Advance the needle until bone is gently contacted—about 25 mm (Figure 4). The target area for this injection is the anterolateral surface of the condyle. By contacting bone, clinicians ensure they have reached the nerve area, in addition to avoiding trauma to vascular structures, the temporomandibular capsule, and the otic ganglion.8,11 If bone is not contacted, withdraw the needle and re-establish the angle. The most common reason for missing the bony contact is deflection of the needle in the mesial direction. To correct this, re-establish the angle with the barrel of the syringe more posteriorly. This will result in the tip of the needle progressing in a more anterior direction, which should ensure contact with the ramus. For example, if the barrel was above the canine in the first attempt, place the barrel over the first premolar for the next try. In order for the GG technique to be successful, the patient needs to open his or her mouth as wide as possible and keep it open throughout the entire injection. When the patient opens wide, the condyle moves to an anterior position and the intraoral tissues are stretched taught, resulting in needle placement close to the mandibular nerve trunk. If the patient’s mouth is partially closed, reaching the target is difficult.

FIGURE 5. The syringe barrel must be placed at the height of the mucogingival junction for the Vazirani-Akinosi injection. The patient maintains a closed mouth with relaxed muscles. - Aspirate in two planes. Once bone is contacted, withdraw 1 mm and perform aspirations. To aspirate in two planes, aspirate the first time, and if the aspiration is negative, rotate the syringe 1/4 turn and aspirate again. If both aspirations are negative, proceed with depositing the anesthetic solution.
- Deliver the anesthetic. A full cartridge (1.8 mL) is sufficient for the GG injection in most cases. Slow administration is recommended, at a rate of one cartridge per minute. In the event of insufficient anesthesia, up to 1.2 mL of additional anesthetic can be administered.2,11 Insufficient anesthesia is typically due to the larger size of the nerve trunk at the neck of the condyle, which can require a larger volume of anesthetic for complete anesthesia. When the GG was originally introduced, the use of 2.2 mL of anesthetic solution was recommended.3
- Withdraw the needle and safely recap.
- Follow the post-injection protocol. Return the patient to an upright position and ask the patient to keep his or her mouth open wide for 1 minute to 2 minutes to aid in the diffusion of the anesthetic into the nerve. If patients are not seated upright and/or close their mouths, the solution will diffuse away from the nerve. The use of a bite block may be helpful.
VAZIRANI-AKINOSI INJECTION

Tha VA is a closed-mouth mandibular block. While it can be used for any mandibular anesthesia, the primary indication for the VA injection is for patients with limited ability to open their mouths. Administering an IA or a GG injection to a patient who cannot keep his or her mouth open is virtually impossible.6
1. Indications for Use
The VA is indicated when mandibular anesthesia is needed, but the patient has limited ability to open his or her mouth or if the landmarks for the IA or the GG are difficult to visualize and/or palpate.6
2. Contraindications
- Infection in the area of injection
- Patients at risk of post-procedural trauma due to numbness, such as young children and patients with physical and developmental disabilities
- Inability to visualize the area of injection
3. Special Considerations
- The VA injection is a closed-mouth procedure, so it is difficult to visualize the depth of penetration. Thus, clinicians must estimate their location (there is no bony contact to indicate proper depth of insertion). Overinsertion can result in penetration of the parotid gland, which may lead to anesthesia of the facial nerve (cranial nerve VII), causing temporary facial paralysis on the side of the injection.2 Paralysis resolves when the anesthetic wears off.
- Onset of anesthesia is about 5 minutes.2
4. Areas Anesthetized
- Mandibular teeth to the midline
- The buccal periosteum and soft tissues anterior to the mental foramen (mental foramen typically adjacent to the mandibular first and second premolar apices) are anesthetized. If the clinician needs the buccal mucosa adjacent to the molars anesthetized as well, a buccal/long buccal injection is needed in addition to the VA.
- Lingual periosteum and soft tissues
- Anterior 2/3 of the tongue and the floor of the mouth
- Inferior portion of the ramus and the body of the mandible
5. Technique
- Needle selection: a 25-gauge long needle is recommended for this injection.
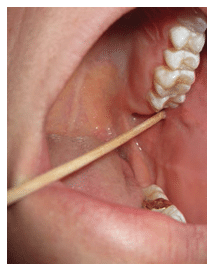
- Identify the penetration site, which is the soft tissue adjacent to the maxillary tuberosity at the height of the mucogingival junction on the medial side of the ramus.
- Prepare the tissues for the injection with topical anesthetic.
- Establish the angle. With the patient’s mouth closed, retract the cheek and visualize the soft tissue at the site of penetration. The barrel of the syringe will be parallel to the occlusal plane, with the needle at the height of the mucogingival junction (Figure 5).
- Penetrate and advance to the site of deposition. The average depth of penetration for the VA is 25 mm—with a 32-mm long needle, 7 mm would remain visible outside of the tissue (Figure 6). For most patients, the hub of the needle will lie just distal to the maxillary second molar.1 Typically, there should be no bony contact with this injection. The bevel of the needle should be positioned toward the midline—not toward the ramus. This will minimize needle deflection during the injection and guide any deflection toward the ramus while keeping the needle closer to the IA nerve.
- Aspirate in two planes. If both aspirations are negative, proceed with depositing the anesthetic solution.
- Deliver anesthetic. Slowly deliver 1.5 mL to 1.8 mL of anesthetic at a rate of one cartridge per minute.
- Withdraw the needle and safely recap.
CONCLUSION
Trying a new technique for the first time can be daunting. However, these alternative injections may improve anesthesia outcomes and increase patient comfort. Strict adherence to the protocol should ensure safe and effective anesthesia. Clinicians may want to consider attending a hands-on continuing education course on administering these injections to increase their confidence.
REFERENCES
- Meechan JG. How to overcome failed local anaesthesia. Br Dent J. 1999;186:15–20.
- Malamed S. Handbook of Local Anesthesia. 6th ed. St. Louis: Elsevier Mosby; 2013.
- Gow-Gates GA. Mandibular conduction anesthesia: a new technique using extraoral landmarks. OralSurg Oral Med Oral Pathol. 1973;36:321–328.
- Wong MK, Jacobsen PL. Reasons for local anesthesia failures. J Am Dent Assoc. 1992;123:69–73.
- Akinosi JO. A new approach to the mandibular nerve block. Br J Oral Surg. 1977;15:83–87.
- Haas DA. Alternative mandibular nerve block techniques: a review of the Gow-Gates and Akinosi-Vazirani closed-mouth mandibular nerve block techniques. J Am Dent Assoc. 2011;142:8S–12S.
- Watson JE, Gow-Gates GA. A clinical evaluation of the Gow-Gates mandibular block technique. N Z Dent J.1976;72:220–223.
- Watson JE, Gow-Gates GA. Incidence of positive aspiration in the Gow-Gates mandibular block. AnesthPain Control Dent. 1992;1:73–76.
- Reed KL, Malamed SF, Fonner AM. Local anesthesia part 2: technical considerations. Anesth Prog.2012;59:127–136.
- Augello M, von Jackowski J, Gratz KW, Jacobsen C. Needle breakage during local anesthesia in the oral cavity—a retrospective of the last 50 years with guidelines for treatment and prevention. Clin Oral Investig. 2011;15:3–8.
- Bassett K, DiMarco A, Naughton D. Local Anesthesia for Dental Professionals. 2nd ed. Upper SaddleRiver, New Jersey: Pearson; 2015.
From Dimensions of Dental Hygiene. September 2015;13(9):50–55.