Advantages of Digital Radiography
Digital imaging offers significant benefits to practices, clinicians, and patients.
Radiography is an essential part of the dental hygiene process of care—playing an important role in assessment, diagnosis, planning, implementation, and documentation.Radiographs are integral to the evaluation of treatment outcomes. While film-based imaging is still used in dentistry, digital imaging is gaining more widespread acceptance, and has many advantages.1 There are many reasons why practices avoid implementing digital radiography into the dental office, including: high cost; analog-based practice (no computers in the office); trepidation regarding the conversion process and necessary staff training; and, for some, the disbelief that digital radiography is an improvement over conventional radiography.2 Digital radiography is available in a variety of systems—plates or sensors, wireless or hard-wired—and much debate exists over which is most effective. Table 1 lists the advantages and disadvantages of digital imaging.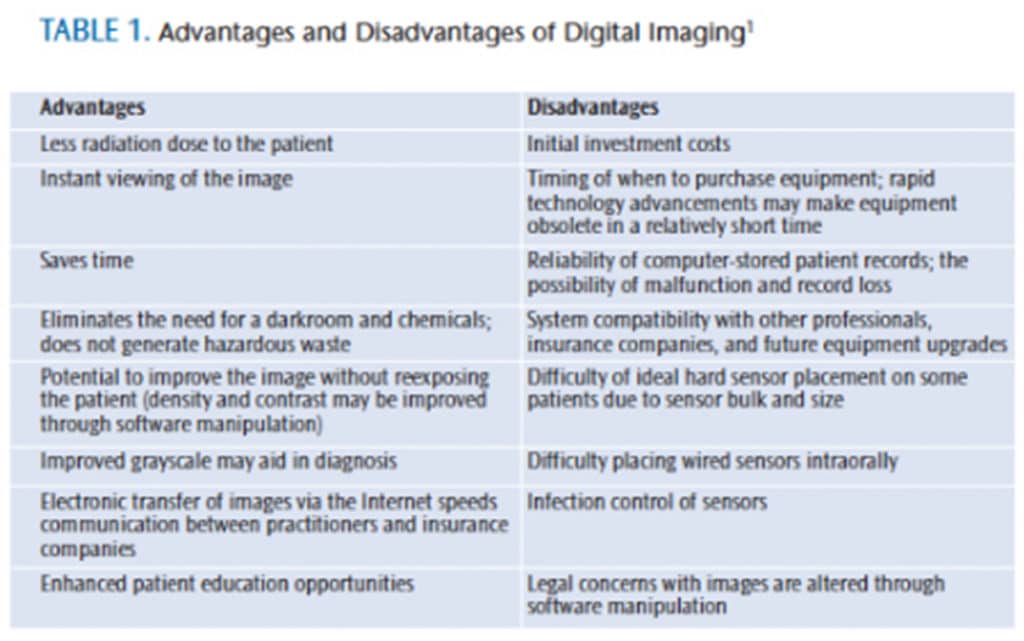
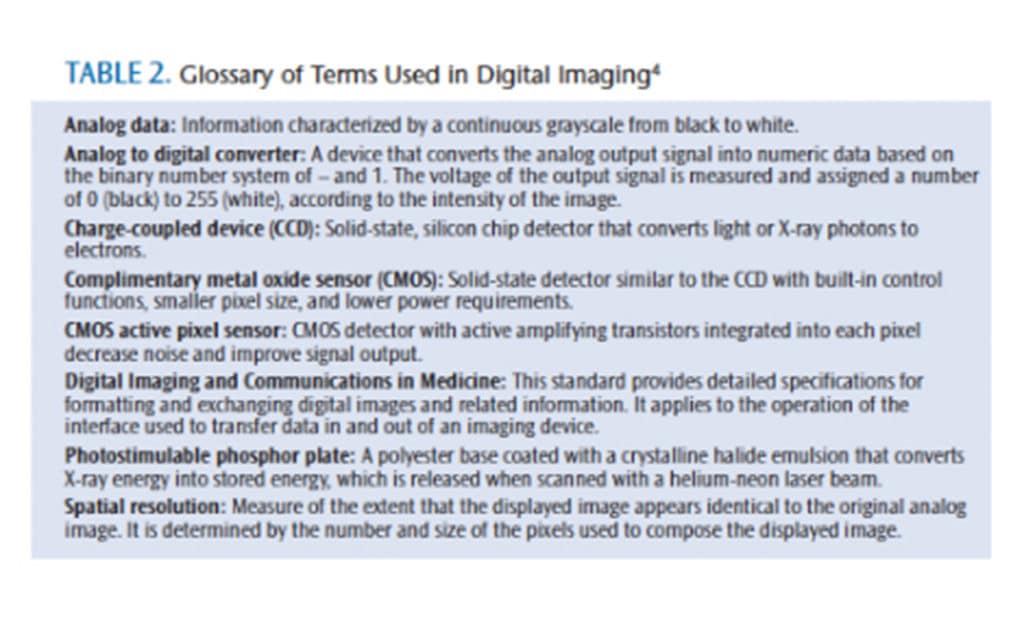
The turning point from film-based X-rays to digital radiography dates back to 1972, when Sir Godfrey Newbold Hounsfield—an English electrical engineer—introduced computerized transverse axial scanning. The first unit accommodated only the patient’s head, with the scan exposure time approximately 4.5 minutes per “virtual slice,” with an additional 1.5 minutes needed for reconstruction. The technique evolved into computed tomography, which requires only seconds to complete a full body scan. In 1987, a direct digital system became commercially available.3 The first dental digital system was capable only of acquiring a radiographic image for print; the image could not be stored on a disk. Table 2 provides a glossary of common terms used in digital radiography.4
MECHANICS
 Digital imaging is very similar to film-based imaging in that it requires X-ray interaction with a receptor, latent image processing, and subsequent viewing of the image. In digital imaging, the receptors are highly sensitive sensors that require less radiation exposure than film. The analog data acquired by the receptor include a continuous grayscale that must be converted to digital data in order to be used. The computer converts the data using an analog-to-digital converter (ADC). Once the computer processes the data, the image appears on the monitor for interpretation, enhancement, and subsequent storage.
Digital imaging is very similar to film-based imaging in that it requires X-ray interaction with a receptor, latent image processing, and subsequent viewing of the image. In digital imaging, the receptors are highly sensitive sensors that require less radiation exposure than film. The analog data acquired by the receptor include a continuous grayscale that must be converted to digital data in order to be used. The computer converts the data using an analog-to-digital converter (ADC). Once the computer processes the data, the image appears on the monitor for interpretation, enhancement, and subsequent storage.
Digital radiography receptors include “direct” and “indirect” receptors. Direct receptors communicate with the computer through an electronic cable or a battery-operated wireless sensor, which transfers data through a radiofrequency transmitter. Direct receptors include: charge-coupled device (CCD), complimentary metal oxide semiconductor (CMOS), and the complimentary metal oxide semiconductor active pixel sensor (CMOS-APS). The indirect sensor is made from a plastic plate coated with a phosphor material sensitive to X-ray radiation. The plate is called a photostimulable phosphor plate (PSP), or storage phosphor plate. When X-rays interact with the phosphor, a latent image is formed and stored until the energy is released during the scanning process.
BENEFITS OF DIGITAL RADIOGRAPHY
While digital X-ray sensors have long equaled analog film for diagnostic tasks, they have several practical advantages over film radiography, including:
- Immediate image production with solid-state devices, such as CCD and CMOS
- Interactive display on a monitor with the ability to enhance image features and make direct measurements
- Integrated storage, providing access to images through practice management software systems
- Security of available backup and off-site archiving
- Image duplicates to accompany referrals to other practitioners5
Table 3 provides additional practice considerations.2
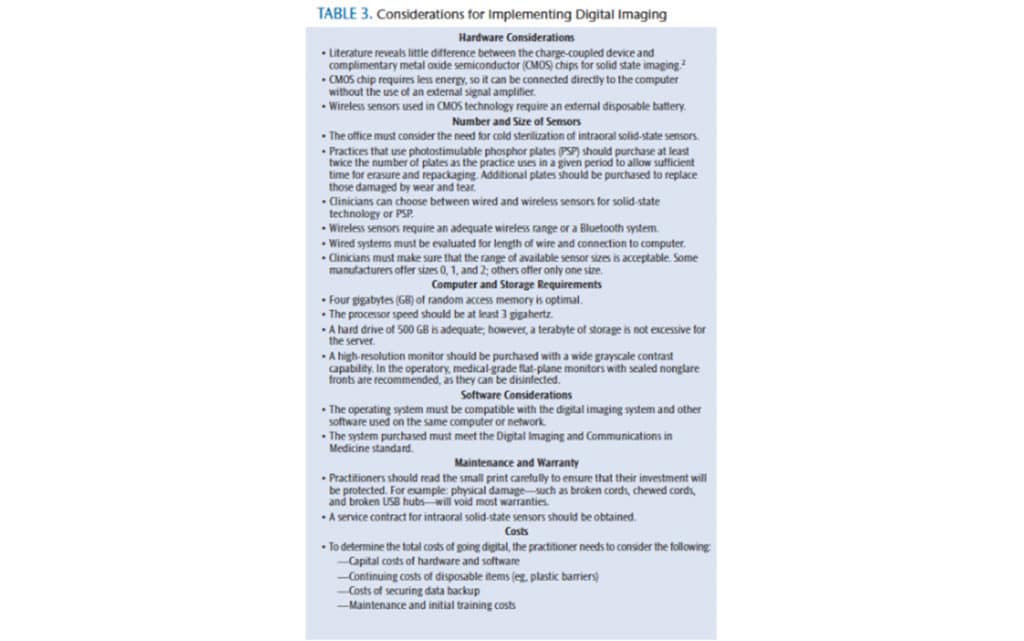 Digital radiography also offers benefits to patients and clinicians. Patients are exposed to significantly reduced radiation doses. Intraoral digital image receptors provide equal or greater dose reduction compared to F-speed film.6 Additional dose reduction can be achieved when retakes are eliminated and the number of additional captured images is limited.7 Anissi and Geibel8 found that the total number of dental films exposed during a 1-week period using CCD sensor systems was significantly higher than for film-based systems, whereas there was no significant difference for the PSP system users. When the subjects were asked why more radiographs were needed, CCD system users cited difficulties in detector positions and initial taking of bad images. In contrast to practitioners working with a PSP system that incorporated two or more plate sizes, CCD system users often utilized one small detector as opposed to multiple sensor sizes.8
Digital radiography also offers benefits to patients and clinicians. Patients are exposed to significantly reduced radiation doses. Intraoral digital image receptors provide equal or greater dose reduction compared to F-speed film.6 Additional dose reduction can be achieved when retakes are eliminated and the number of additional captured images is limited.7 Anissi and Geibel8 found that the total number of dental films exposed during a 1-week period using CCD sensor systems was significantly higher than for film-based systems, whereas there was no significant difference for the PSP system users. When the subjects were asked why more radiographs were needed, CCD system users cited difficulties in detector positions and initial taking of bad images. In contrast to practitioners working with a PSP system that incorporated two or more plate sizes, CCD system users often utilized one small detector as opposed to multiple sensor sizes.8
A pixel, or picture element, is one of the thousands of tiny dots that make up an image. Digital sensors are composed of an array of thousands of tiny electron wells. Each of these wells typically represents one pixel in the final image. Smaller and more tightly packed wells generally result in increased resolution.
IMAGE QUALITY
Spatial resolution is the eye’s ability to distinguish fine detail in an image. It is recorded and presented in line pairs per millimeter (lp/mm). While film provides more than 20 lp/mm, digital systems average anywhere from 7 lp/mm to 25 lp/mm, depending on the size of pixels in the image.9 Both systems create diagnostic images, however, PSPs can produce 15 lp/mm to 20 lp/mm and sensors can produce 24 lp/mm at the maximum resolution settings. The quality of the PSP images is lower than that of a sensor, but the human eye cannot distinguish above 12 lp/mm.10
Some sensors are capable of capturing up to a 16-bit image, meaning they can distinguish 65,536 shades of gray. A computer monitor, however, can only display an eight-bit image, or 246 shades of gray. The human eye can only see about 64 shades of gray. Based on the limitations of the human eye, all sensors are acceptable. The available data may provide improved results in the future with enhancement software and higher resolution monitors.11 In comparison to the average computer monitor display, a liquid-crystal display (LCD) monitor frequently used by radiologists is capable of displaying 2,048 shades of gray. High-resolution monitors or LCD medical-grade monitors are both options when choosing a digital radiography system.
EASE OF USE
The primary advantage of direct sensor systems is the speed in which images are acquired. The sensor is connected either by a wire or wirelessly to an ADC. Images are produced within seconds of sensor exposure. Most of the current sensors utilize cords (rather than wireless), which, along with sensor thickness, may make placement more difficult than conventional film or PSPs. Scientific literature reveals little difference between the CCD and CMOS chips for solid-state imaging in terms of physical properties, but it may be more difficult to obtain vertical bitewing radiographs with corded sensors.12 Cost is another consideration. At several thousand dollars per sensor, they will likely be shared rather than purchasing one or two sensors for each operatory. Practitioners must read the fine print of the warranty, as physical damage will void its validity.
As with direct systems, there are advantages and disadvantages to indirect systems. The smaller size and lack of a cord may make intraoral placement of PSPs easier than direct sensors. PSPs are somewhat flexible, but the corners cannot be bent (as is sometimes done with film) without damaging the plate. PSP sizes are almost identical to those available for conventional film. The disadvantages include the risk of scratching/damage to the plate, the time needed to prepare and package the plates, and the time required to scan with a laser to process the latent image. Bedard et al13 found that PSPs needed to be replaced after 50 uses to avoid degradation of image quality due to scratches and irregularities. Producing an image with a PSP is not immediate, but it is faster than film. Following exposure, plates must be removed from their contaminated barrier pouches, run through the scanner, “erased” with bright light, and repackaged in clean barrier pouches. Some scanners incorporate an erase cycle, while other units have a separate plate eraser that follows the scanning process. Contamination of the PSP is also a concern.
The advent of digital radiography has created new infection control challenges not seen with film-based imaging. With conventional film imaging, contamination is prevented by completely disposing of the packaging. In contrast, digital receptors are reused many times, but are not suitable for autoclave sterilization; therefore, cross-contamination is possible. PSPs must be disinfected following removal from a contaminated barrier envelope before placement into a new barrier envelope. Contamination of the PSP can result from perforation of the plastic barrier envelope, incorrect sealing of the edges of the barrier envelope, and contact during the removal of the plate during processing. In a study on PSP contamination, MacDonald and Waterfield14 found bacterial growth on 56% of PSPs, while Negron et al15 discovered streptococcus contamination in 61% of plates after 24 hours of culture.
The CDC recommends items that cannot tolerate heat or chemical immersion should be covered with a Food and Drug Administration-cleared barrier during intraoral use. The items must then be cleaned and disinfected with an Environmental Protection Agency-registered hospital disinfectant that offers tuberculocidal activity.16 Clinicians must consult with the manufacturer to determine appropriate methods of disinfection and sterilization for digital radiology sensors and how best to protect associated computer hardware.
CONCLUSION
Some of the advantages of digital radiography are not achievable with conventional film-based radiography. Current technological advances include the ability to measure bone height, root canals, and anatomical structures utilizing digital subtraction technology. Additional caries detection software can be purchased, which detects and measures density differences of digital radiographs.
Integrating digital radiography into the dental office requires additional training. Once the team is prepared, patients can benefit from several new diagnostic possibilities. Digital images may be enhanced once acquired, conveniently stored, accessed, printed, or transmitted. Digital radiography reduces patient radiation exposure and eliminates chemical processing. The quality of the images produced remains dependent on clinicians’ technical skills. Digital radiographic images are equivalent or superior to film-based radiography in their ability to diagnose caries, periodontal bone loss, and periapical lesions.17
REFERENCES
- Thomson E. Exercises in oral radiography techniques. In: Darby M, Walsh P, eds. Dental Hygiene Theory and Practice. Philadelphia: Saunders; 2007:384–385.
- Christensen GJ. Why switch to digital radiography? J Am Dent Assoc. 2004;135:1437–1439.
- Sanderink GC, Huiskens R, Van der Stelt PF, et al. Image quality of direct digital intra-oral x-ray sensor in assessing root canal length. Oral Surg Med Oral Pathol Oral Radiol Endod. 2003;96:223–228.
- Muhamedagic B, Muhamedagic L. Digital radiography versus conventional radiography in dentistry. Acta Inform Med. 2009;17;2:85–89.
- Farman AG, Levato CM, Gane D, Scarfe WC. In practice: how going digital will affect the dental office. J Am Dent Assoc. 2008;139:14–19.
- White SC, Pharoah MJ. Oral Radiology Principles and Interpretation. 6th ed. St. Louis: Mosby; 2009:37.
- Wenzel A., Moystad A., Work flow with digital intraoral radiography: a systematic review. Acta Odontol Scand. 2008;68:106–114.
- Anissi HD, Geibel MA. Intraoral radiology in general dental practices—a comparison of digital and film-based X-ray systems with regard to radiation protection and dose reduction. Rofo. 2014;186:762–767.
- Cederberg R. Intraoral digital radiography: elements of effective imaging. Compend Contin Educ Dent. 2012;33:656–664.
- Jablow M. Digital radiography: analyzing the benefits. Compend Contin Educ Dent. 2012;33:142–143.
- Emmott L. Making sense of sensors: aguide to choosing digital radiography sensors. Dental Products Report. 2002;3:36-40.
- Kitagawa H, Scheetz JP, Farman AG. Comparison of complementary metal oxide semiconductor and charge-coupled device intraoral X-ray detector using subjective image quality. Dentomaxillofac Radiol. 2003;32:408–411.
- Bedard A, Davis TD, Angelopoulos C. Storage phosphor plates: how durable are they as a digital dental radiographic system? J Contemp Dent. 2004:5:57–69.
- MacDonald DS, Waterfield DJ. Infection control in digital intraoral radiography: evaluation of microbiological contamination of photostimulable phosphor plates in barrier envelopes. J Can Dent Assoc. 2011;77:93.
- Negron W, Mauriello SM, Peterson CA, Arnold R. Cross-contamination of the PSP sensor in preclinical setting. J Dent Hyg. 2004;79:8.
- Kohn WG, Harte JA, Malvitz DM, et al. Guidelines for infection control in dental health-care setting—2003. J Am Dent Assoc. 2004;135:33–47.
- Williamson GF. Digital Radiography in Dentistry: Moving From Film-Based to Digital Imaging. Available at: dentalcare.com/media/enus/education/ce350/ ce350.pdf. Accessed November 12, 2014.
From Dimensions of Dental Hygiene. December 2014;12(12):43–46.

