Managing Medical Emergencies
Dental team members need to be prepared to handle a variety of emergencies during the provision of routine dental care.
This course was published in the January 2015 issue and expires January 31, 2018. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES</strong
After reading this course, the participant should be able to:
- Discuss the potential for medical emergencies in the dental office.
- Identify the key components of a comprehensive medical emergency kit.
- Explain management strategies for the most common emergencies encountered in dental practice.
Advances in dentistry and medicine have increased the number of patients with complicated medical histories who present to the dental office for treatment. It is not uncommon to encounter patients who have undergone organ transplants, artificial joint replacements, complex surgical heart valve repairs, and coronary artery revascularization. Additionally, the introduction of a wide range of therapeutic options used in dental treatment can increase the likelihood of potential drug interactions. Moreover, comprehensive dental care and advances, such as implants and extensive restorative treatment, are leading to long-term dental treatment needs that attract a stabilized, yet chronically ill and aging patient population. These factors increase the likelihood of a medical emergency in the dental office.
Older adults and patients with special needs, in particular, are at increased risk for adverse drug reactions and medical emergencies in the dental office. There are many physiologic and pathologic changes that occur over time, combined with the deterioration of major organs and systems that make this population more prone to acute exacerbation of chronic conditions. In addition, aging alters the pharmacokinetics of many drugs, which increases sensitivity, especially central nervous system depressants. On the other hand, the increased incidence of obesity and adult-onset diabetes among all age groups may increase risk, as well.1
Preparing for a medical emergency in the dental office requires organization, preparation, and continual training and review for all clinical office staff. Although keeping the appropriate emergency equipment and drugs on hand is important, it is the training and expertise of the dental team that makes the difference when responding to a medical emergency. Obtaining an appropriate medical history, with an emphasis on review of systems, medications, and allergies, is essential.2
A team approach to treating medical emergencies in the office is the foundation of successful care. Early diagnosis and management are the hallmarks for successful outcomes. An organized response and a designated role for each caregiver are mandatory to ensure a proper response and management. Conducting mock drills and rehearsing emergency situations regularly, in addition to certification in Basic Life Support for Healthcare Providers (BLS-HCP), will hone the skills of the entire team. Creating a planned protocol of whom to call for help and what information should be transmitted is imperative to ensure that this important component of any emergency algorithm is appropriate.3
PREPARING FOR EMERGENCIES
Every dental office should have a basic emergency kit with drugs and equipment appropriate to its training level, state regulations, type of patients treated, location, and whether sedation is administered.4
Oxygen must be available in a portable “E” cylinder that can be easily transported and holds more than 600 liters. Oxygen delivery systems for the spontaneously breathing patient include nasal cannula, face mask, nonrebreathing mask with an oxygen reservoir, or the nitrous oxide-oxygen nasal hood. Every office must be able to deliver oxygen under positive pressure for the unconscious, apneic patient. The most effective method is a bag-valve-mask device connected to an oxygen source.
Magill forceps are useful in retrieving foreign objects from the hypopharynx. An automated external defibrillator (AED) is key to providing early defibrillation for patients experiencing ventricular tachycardia. An AED that is easy to use and helps convert arrhythmias to normal sinus rhythm will ensure proper perfusion of vital organs.
A manual aneroid sphygmomanometer with a variety of cuff sizes should be available. Many offices have an automated vital sign monitor that can easily obtain systolic/diastolic blood pressure, mean arterial pressure, heart rate, and oxygen saturation. A clock with a second hand is invaluable in determining heart rate and documenting the sequence of events.
Emergency drug kits can either be organized by the dental team or purchased commercially. The composition of these kits will vary according to the needs of the practice. There are critical drugs, however, that should be in every dental office, such as oxygen and epinephrine. Oxygen is the primary drug used during any medical emergency. Increasing arterial oxygen tension improves the perfusion of the peripheral tissues and ensures adequate oxygen delivery to the brain.
Epinephrine is the single most important injectable drug in the emergency kit and is the drug of choice in managing cardiovascular and respiratory manifestations of acute anaphylaxis and treating acute asthma attacks that are nonresponsive to inhalers. Epinephrine is a potent bronchodilator that also increases systemic vascular resistance, arterial blood pressure, heart rate, heart contractility, and coronary and cerebral blood flow.
For the emergency treatment of severe allergic reactions or refractory bronchospasm, epinephrine can be injected intramuscularly as 0.3 ml to 0.5 ml of 1:1,000 solution. For offices trained in advanced cardiac life support, epinephrine 1 mg of 10:000 solution intravenously is part of the cardiac arrest algorithm.
Diphenhydramine HCl is an antihistamine and is used to treat mild to moderate or delayed onset allergic reactions. It can be administered intravenously (25 mg to 50 mg) to treat a moderate skin reaction, or orally (25 mg to 50 mg) for mild, less severe reactions.
Nitroglycerin is indicated in cases of the acute onset of chest pain caused by angina pectoris or myocardial infarction (MI). It acts by relaxing vascular smooth muscle walls, and causes dilation of veins and arteries. For emergency use, nitroglycerin comes in sublingual tablets and as an aerosol in a liquid pump spray. Pain relief usually occurs within 1 minute to 2 minutes. If symptoms persist, a diagnosis of MI should be suspected. Systolic blood pressure below 90 mmHg is a contraindication to the administration of nitroglycerin. For patients taking erectile dysfunction medications, nitroglycerin should be administered cautiously due to the possibility of hypotension.
Bronchodilators are used in the treatment of acute bronchospasms caused by asthma attacks. They relax the bronchial smooth muscle walls and inhibit the chemical mediators that are usually released during hypersensitivity reactions. Albuterol is the preferred choice, as it has fewer cardiovascular side effects. Patients with asthmatic histories usually present with their own inhalers, which should be used first.
Aspirin is of paramount importance if an acute MI is suspected. It helps prevent the enlargement of clots in the coronary arteries and, thus, helps decrease mortality due to its immediate antiplatelet actions. Nonenteric coated aspirin, either a 325 mg dose or four 81 mg tablets, should be chewed and swallowed when a case of MI is suspected.
Hypoglycemia can result from fasting or an insulin/carbohydrate imbalance in patients with diabetes. Glucose in an oral carbohydrate form (eg, orange juice, chocolate, nondiet soft drink) can be administered only if the patient is conscious. Oral preparations should not be administered to unconscious patients, as they could lead to airway obstruction and aspiration. There is no place for insulin as an emergency drug in the dental office.
Aromatic ammonia is an irritating respiratory stimulant used to arouse an unconscious syncopal patient. It is available as a vaporole. Additional drugs may be added to emergency kits, but these should dictated by the training and educational qualifications of the dental team. These parenteral administered drugs may include the following:
- Glucagon: a drug that addresses hypoglycemia in the unconscious patient
- Ephedrine: a vasopressor that treats hypotension
- Atropine: an antimuscarinic and anticholinergic drug that elevates heart rate and, thus, raises blood pressure
- Corticosteroid: used as a secondary drug in the treatment of anaphylaxis
- Opioids: such as morphine or fentanyl for the treatment of pain associated with MI
- Reversal drugs for sedation/anesthesia: naloxone to reverse the respiratory depressant effects of opioids and flumazenil to reverse the effects of benzodiazepines
- Injectable benzodiazepine: for the management of intractable or prolonged seizures
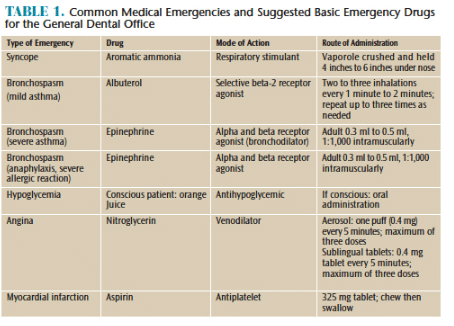
Crisis management education may include assisting with bag-valve-mask ventilation, anticipating drug and equipment needs, monitoring vital signs, and being prepared to take over chest compressions. Creating planned protocols and reviewing medical emergency scenarios as an office are the key for preparedness.5–7 Table 1 provides drug suggestions for the most common medical emergencies experienced in the dental office.
![Medical Emergencies]() EMERGENCY MANAGEMENT
EMERGENCY MANAGEMENT
Asthma is a common disorder characterized by a hyperreactive airway. The result is a narrowing of the bronchial smooth muscle walls and an increase in airflow resistance. Hence, the acute asthmatic reaction results in bronchospasm that can be fatal if not properly managed. Taking a thorough medical history that specifies whether the asthma is allergic is helpful in predicting its occurrence. If nonallergic, anxiety and fear may be predisposing factors. Knowledge of any allergies and the patient’s medication usage, in addition to history of hospitalization, is essential to the successful management of an asthmatic episode.8–10
Management starts by evaluating the severity and urgency of the situation. In cases of mild asthma, beta 2 aerosol agonists, such as albuterol, can be administered, in addition to supplemental oxygen. Dosage is usually two puffs of either the patient’s own inhaler or an albuterol inhaler from the emergency kit. Symptoms usually subside in 15 seconds to 30 seconds. In severe asthmatic reactions not alleviated by inhalers, emergency medical services (EMS) should be immediately contacted. If the patient continues to deteriorate, intramuscular epinephrine should be injected.8–10
Angina pectoris is usually described as a heaviness in the chest and may present with pain radiation to the left shoulder/arm, jaw, or back. Pain usually occurs due to atherosclerosis or narrowing of major heart vessels. Many patients with a history of stable angina can be precipitated by stress, anxiety, or pain. Episodes usually last between 5 minutes and 15 minutes. Symptoms can usually be relieved with nitroglycerin in the form of sublingual fast-absorbing tablets or sublingual spray. Expiration dates should be checked periodically, as nitrites have a short shelf life. Patients sometimes present with their own nitroglycerin, which should be used first. The usual dose is one tablet to two tablets or two sprays every 5 minutes not exceeding three doses. Oxygen can also be given during the attack.8–10
MI or acute coronary syndrome usually is the result of atherosclerosis in coronary arteries and ischemia in the heart muscle. It can lead to irregular heartbeat or cardiac arrest. Patients present with similar symptoms to angina, but typically symptoms persist for longer than 20 minutes, or the pain is unresponsive to nitroglycerin. If pain is unrelieved by nitroglycerin or if the onset of symptoms is new, 911 should be called immediately. Managing the patient with MI until EMS arrives consists of administering oxygen and nitroglycerin, and having the patient chew, then swallow one adult 325 mg tablet of nonenteric-coated aspirin.8–10
If the patient loses consciousness due to an evolving MI and experiences cardiac arrest, BLS-HCP protocol should immediately begin until help arrives. Chest compressions at a rate of 100 per minute at a ratio of 30 compressions to two ventilations with the use of a bag-valve-mask system connected to a 100% oxygen source must commence. After five cycles of chest compressions, a new rescuer should take over. The presence of an AED for defibrillation can significantly improve survival rates.11
Vasovagal syncope is common in the dental setting among healthy individuals. It usually is precipitated by stressful or anxiety-provoking situations. It may be associated with prodromal symptoms, such as nausea, lightheadedness, increased heart rate, blurred vision, confusion, and abdominal pain. Often, repositioning the patient in a supine position, in which the head is at the same level as the heart and the legs are slightly elevated, prevents loss of consciousness. If transient loss of consciousness occurs, urgent assessment of the airway to confirm air exchange and patency of the airway is essential. The basic airway maneuvers of head tilt, chin lift are employed if necessary. Aromatic ammonia—a respiratory stimulant—can also be used to arouse patients.
A detailed history of preexisting seizure disorder is important, as it provides information regarding type, severity, duration, and medication effectiveness in controlling seizure disorders. Some patients experience a prodromal event, such as an aura that can be visual or olfactory. Some seizures can be initiated with toxic or intravascular doses of local anesthetics. Management is directed at preventing injury and assuring air exchange. If a seizure occurs during treatment, the patient should be repositioned away from any sharp objects. Gently holding the patient’s arms and legs can also help prevent injury. Patients may lose consciousness during and after the episode. Seizures related to local anesthetic issues are usually self-limiting. No matter what their etiology, seizures lasting more than 5 minutes are dangerous and require activation of emergency response. Patients may be disoriented and fatigued, and must be carefully assessed prior to leaving the dental office.
Allergic reactions can vary from mild to severe, and may develop a few seconds or hours after exposure to an allergen. In dentistry, the most common allergens are latex and antibiotics. If the reaction is mild, occurs over time, and only itching and/or rash are seen, an antihistamine may be appropriate. If the reaction is immediate and cascades into respiratory and cardiovascular involvement, then it is life-threatening. Epinephrine is the sole treatment in this situation, and successful outcome is determined by early diagnosis and the immediate administration of epinephrine. Epinephrine, via autoinjector, should be administered into the vastus lateralis muscle on the lateral side of the thigh.
During a major allergic reaction, loss of consciousness is common and the airway must be monitored and assisted if necessary. On the diagnosis of an acute and serious allergic response, 911 should be called immediately.12
CONCLUSION
Anticipation of medical emergencies is an important aspect of practicing safe dentistry, and clinical dental team members should be trained to immediately diagnose and assist in managing medical emergencies. They should be familiar with basic equipment and critical drugs. Dentists and dental hygienists should always actively monitor their patients for acute changes in their medical conditions, especially patients with complex medical histories. An emergency preparedness plan should be present in each office where the roles of the dentist, dental hygienists, dental assistants, chairside assistants, and front office staff are continually reviewed and updated. Routinely rehearsing medical emergency scenarios and incorporating a team approach into their management will increase the effectiveness of treatment and the safety of patients.
REFERENCES
- Reed KL. Basic management of medical emergencies: recognizing a patient’s distress. J Am Dent Assoc. 2010;141(Suppl 1):20S–24S.
- Haas DA. Preparing dental office staff members for emergencies. J Am Dent Assoc. 2010;141:8S–13S.
- Fast TB, Martin MD, Ellis TM. Emergency preparedness: a survey of dental practitioners. J Am Dent Assoc. 1986;112:499–501.
- Rosenberg MB. Preparing for medical emergencies. J Am Dent Assoc. 2010;141(Suppl 1):14S–19S.
- Part 3: effective resuscitation team dynamics. In: Advanced Cardiac Life Support: Professional Provider Manual. Dallas: American Heart Association; 2006:11–17.
- Gaba DM, Fish KJ, Howard SK. Principles of anesthesia crisis resource management. In: Crisis Management in Anesthesiology. Philadelphia: Churchill Livingston; 1994:31–52.
- Haas DA. Management of medical emergencies in the dental office: conditions in each country, the extent of treatment by the dentist. Anesth Prog Spring. 2006;53:20–24.
- Saef SN, Bennett JD. Basic principles in resuscitation. In: Bennett JD, Rosenberg MB, eds. Medical Emergencies in Dentistry. Philadelphia: Saunders; 2002:53–59.
- Malamed SF. Managing medical emergencies. J Am Dent Assoc. 1993;124:40–53.
- Becker DE, Rosenberg MB, Phero JC. Essentials of airway management, oxygenation, and ventilation. Anesth Prog. 2014;61:78–83.
- Advanced cardiac life support. In: Advanced Cardiac Life Support: Professional Provider Manual. Dallas: American Heart Association; 2011.
- Rosenberg MB, Phero JC, Giovannitti JA. Management of allergy and anaphylaxis during oral surgery. Oral Maxillofac Surg Clin North Am. 2013;25:401–406.
From Dimensions of Dental Hygiene. January 2015;13(1):52–55.


 EMERGENCY MANAGEMENT
EMERGENCY MANAGEMENT
