Manage the Threat
Oral health professionals need to be well informed about emerging infectious diseases in order to reduce their associated risks.
Disease outbreaks are in the news every day. Most recently, reports of Ebola, Middle East respiratory syndrome (MERS), and enterovirus D68 have made headlines. Oral health professionals must be diligent in understanding the signs and symptoms of emerging infectious diseases, how they are spread, and how to prevent the further dispersal of these diseases.
Several factors impact the emergence of infectious diseases, such as population density, agricultural practices, the human immunodeficiency virus/acquired immune deficiency syndrome pandemic, improper antibiotic use, and environmental factors.1 Jones et al1 hypothesized that weather conditions, climate changes, higher temperatures, and precipitation in regions close to the equator help to promote the growth and spread of pathogens. Many developing countries are prime “hot spots” for the emergence and spread of infectious diseases due to poor water and sanitation practices, population density, lack of adequate health resources, and living in close proximity to animals, which are disease reservoirs. In fact, the majority of infectious disease are caused by zoonotic pathogens that originate in wildlife, such as severe acute respiratory syndrome (SARS) and Ebola.1
EBOLA VIRUS
As of November 12, 2014, the World Health Organization (WHO) reports 14,098 cases of Ebola with 5,160 deaths and a case fatality rate (CFR) of 37%.2 This number may be a significant underestimate, as calculations are based on the number of deaths reported divided by the total number of cases. As such, the current CFR is estimated to be 70% or higher; it could be calculated more precisely if individual patient data could be gathered.2
Hemorrhagic fevers, such as the Ebola virus (Figure 1) and Marburg virus, belong to the virus family Filoviridae, which was first reported in 1967 in Yugoslavia.3–5 Outbreaks of hemorrhagic fever were reported in Sudan and Zaire (now the Democratic Republic of the Congo) in 1976. There are five known strains of the Ebola virus, named after the region in which they were discovered: Zaire, Sudan, Tai Forest, Bundibugyo, and Reston.3–5 Four of the five strains originate in Africa and are known to cause disease in humans. The Reston strain, originating in the Philippines, appears to be nonpathogenic in humans.3,4 Of the African strains, Ebola Zaire appears to be the most deadly with a 60% to 90% CFR, while the Ebola Sudan has a 40% to 60% CFR.3 The Bundibugyo strain carries a 25% CFR. Only one documented case of Ebola Tai Forest exists, and the individual survived.3
Strides have been made in understanding Ebola virus disease (EVD) in recent years, but accessing remote villages in equatorial Africa is challenging. Outbreaks of EVD have been frequent in several equatorial African countries over the past two decades, but they were generally contained to remote areas. Limited access and travel to these regions kept the outbreaks isolated.1 In contrast, the 2014 outbreak migrated into well-populated countries, such as Liberia and Sierra Leone, where the outbreak has spread rapidly in densely populated cities with poor isolation and containment measures.
The Zaire strain of the Ebola virus is a zoonotic pathogen that is thought to originate in the African fruit bat.3 Infection with EVD is transmitted via direct contact with an infected person’s blood and bodily fluids (urine, feces, saliva, vomit, and semen) through breaks in the skin and via accidental injection.3 Direct contact with infected cadavers or the ingestion of bush meat (chimpanzees and bats) are also documented routes of transmission.3 Ebola is not spread through airborne transmission or drinking water.3
Once infected, EVD moves to the lymph nodes and then to the liver, spleen, and adrenal glands. Blood clotting mechanisms are broken down, resulting in acute liver failure, which leads to multiorgan failure and death. EVD’s incubation period can range from 2 days to 21 days, with an average of 4 days to 10 days. The early clinical manifestations of EVD encompass a rapid onset of symptoms, including fever higher than 100.4°, chills, malaise, muscle weakness, and pain. Eventually, multiple body systems become involved, and additional symptoms present that affect the gastrointestinal system (nausea, vomiting, abdominal pain, diarrhea); respiratory system (chest pain, shortness of breath, cough, nasal discharge); vascular system; and neurological system (headache, confusion, coma). Rashes around the face, neck, arms, and body may also be evident. Classic hemorrhagic signs occur at the peak of infection, characterized by oozing at intravenous and injection sites and bleeding out of mucosal sites. Initial symptoms progress systemically after approximately 5 days, with death occurring typically between day 6 and day 16. Death usually occurs from multiorgan failure and septic shock. Patients who survive begin to see symptom improvement from day 6 to day 11 and endure a long period of recovery.3,5,6
EVD is easily confused with other infections, such as malaria, typhoid fever, pneumonia, and other diseases endemic to tropical Africa. Patients exhibiting early signs of EVD must be thoroughly questioned about epidemiological risk factors, such as travel to an active EVD country, participation in death rituals, handling or ingestion of bush meat, and contact with patients suspected or known to have EVD. Patients suspected of having EVD should be isolated as soon as possible to prevent the spread of the disease. Strict barrier protection must be used, including respirators and protective clothing. There is no treatment for EVD, but vaccines are currently under investigation. Clinical management should include electrolyte replacement, administration of fluids, use of vasopressors, oxygen supplementation, keeping the patient comfortable, fever reduction, use of antibiotics for secondary infections, control of bleeding, and nutritional support.3,6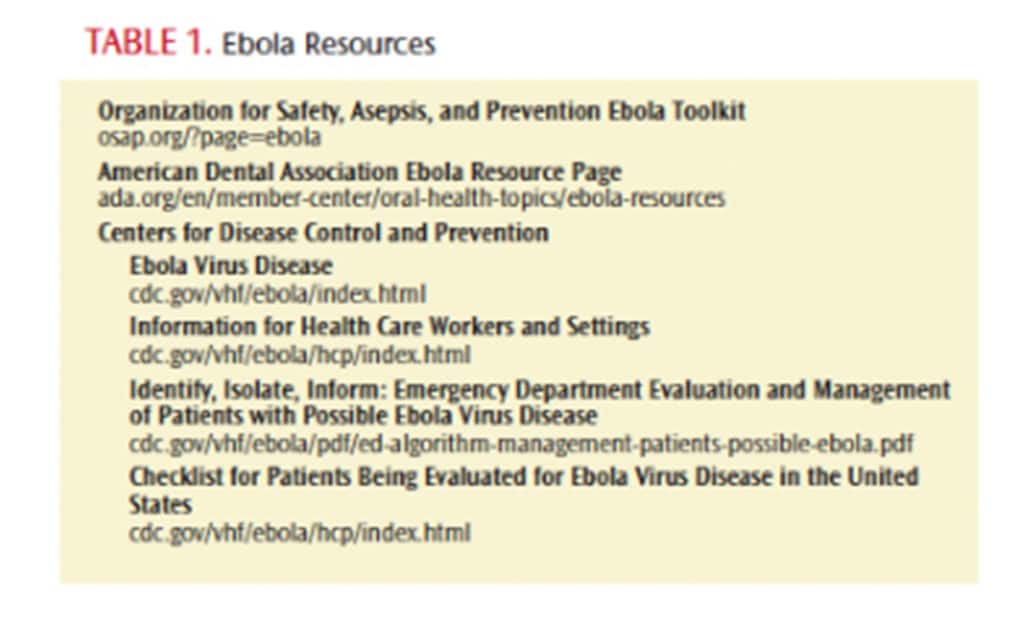
The United States Centers for Disease Control and Prevention (CDC) states that EVD is contagious only when patients are symptomatic. EVD is not contagious in the absence of symptoms, so casual contact poses no risk. The CDC encourages stringent infection control measures for all health care workers and has been preparing for disease outbreaks by providing guidance for health professionals, emergency medical personnel, flight crews, and customs agents. Timely updates have been provided by the CDC (Table 1) to the public, international travelers, and public health partners.7–9
The CDC has provided specific guidance for health care workers. A flow chart can be found at cdc.gov/vhf/ebola/pdf/ed-algorithm-management-patients-possible-ebola.pdf. This algorithm is an easy way for health care workers to quickly address and triage a patient suspected of having EVD. The first step in assessing a patient includes identifying exposure history by questioning about travel habits to West Africa and/or contact with a person known to have a confirmed case of EVD in the past 21 days. The second step is to identify the signs and symptoms. If EVD is suspected, the patient should be isolated, the case should be immediately reported to the hospital infection control department and the health department, and appropriate personal protective equipment (PPE) should be donned. At a minimum, PPE should include a full face shield and a surgical mask, impermeable gown, and two pair of gloves. PPE must be reevaluated if the patient’s condition changes.8
The risk for transmission of EVD in dentistry is low.10 It is unlikely patients with EVD symptoms will present for routine dental treatment; however, oral health professionals should be aware of the signs and symptoms of EVD and the appropriate screening questions to ask. The American Dental Association (ADA) Division of Science advises dental professionals to take a medical history, including a travel history from their patients with symptoms or signs in which a viral infection is suspected, in addition to adding the following questions to the practice’s health questionnaire: Have you traveled to Liberia, Sierra Leone, or Guinea in the past 21 days? and Are you feeling feverish? If the patient answers yes to both questions, he or she may be at risk of EVD. Dental professionals and staff should immediately protect themselves by using standard precautions with PPE; call 911; notify the appropriate state or local health department authorities; and ask the health department to provide guidance on removing and disposing of potentially contaminated materials and equipment, including the physical barriers.10
MIDDLE EAST RESPIRATORY SYNDROME
As of November 7, 2014, the WHO reports 909 laboratory confirmed cases of infection with MERS coronavirus (MERS-CoV), with at least 331 related deaths for an approximate death rate of 36%.11 The emergence of MERS was first reported in 2012 in the Arabian Peninsula.12 Coronaviruses are common and can cause mild to moderate upper respiratory symptoms.11,12
MERS-CoV is a zoonotic pathogen that originates in dromedary camels.13,14 The route of MERS transmission from camels to humans and from human to human is not fully understood. Infection with MERS is thought to be transmitted via direct contact with camels infected with MERS-CoV.11,13,14 Camels have historically been an important part of the culture of the Arabian Peninsula. The ingestion of infected camel products, prolonged contact with infected camels, and contact with infected camel saliva are likely sources of infection in humans.11,13,14
The incubation period of MERS is generally 2 days to 14 days, and symptoms include fever, cough, and shortness of breath. Some have reported gastrointestinal symptoms, including diarrhea, nausea, and vomiting. Some cases of MERS included more severe complications (pneumonia and kidney failure), while others exert very mild symptoms or no symptoms at all.15 People with impaired immune systems are at increased risk for acquiring MERS and enduring a more severe case. MERS poses a low risk to the public, as it does not spread easily from human to human.16
Currently, there is no vaccine to prevent MERS. To protect against respiratory illnesses, the CDC recommends the use of routine infection prevention measures, such as regular hand washing, frequent disinfection of surfaces, avoiding sick people, use of hand sanitizers, practicing good respiratory hygiene (Table 2),17 and refraining from touching the eyes, nose, and mouth.15 The WHO recommends avoiding close contact with animals, particularly camels, as well as abstaining from consuming raw camel milk or eating camel meat that has not been properly cooked.11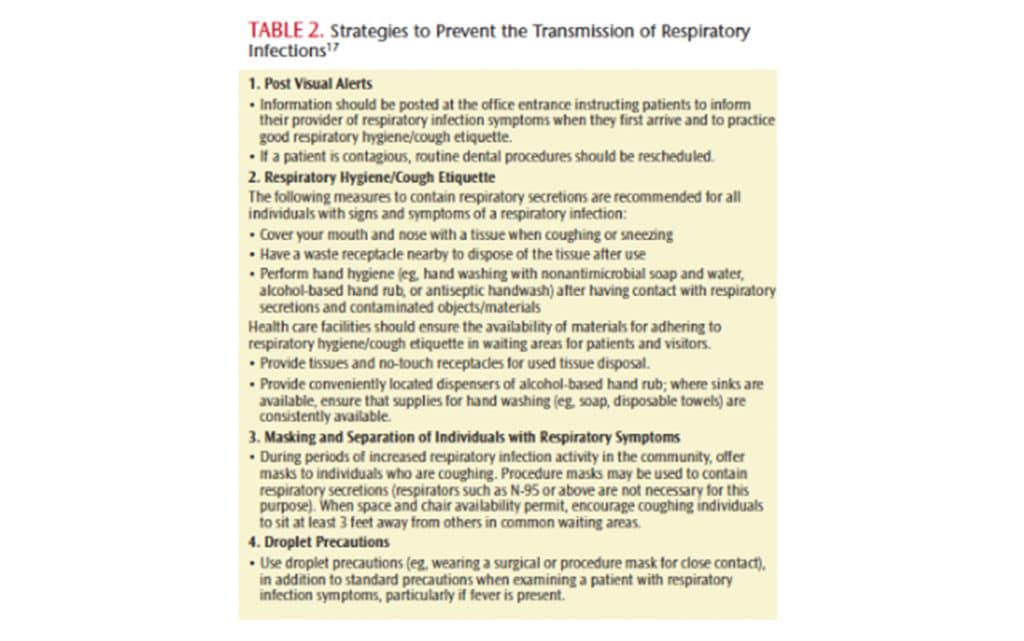
Health care workers should adhere to meticulous infection control practices to prevent the possible spread of MERS. The signs and symptoms of MERS appear nonspecific and are similar to many other illnesses, so the use of standard precautions is necessary. Care should be taken when handling patients with respiratory symptoms. The use of eye protection and respirators are airborne precautions that should be used during aerosol-generating procedures.
ENTEROVIRUS D68
As of November 20, 2014, the CDC has reported 1,121 confirmed cases of enterovirus D68 (EV-D68) in 43 states.18 EV-D68 is a common virus that manifests as a severe respiratory illness and is usually seen in late summer and early fall. The 2014 outbreak has primarily affected children and those with weakened immune systems. Symptoms typically include mild fever, runny nose, cough, sneezing, and body aches. In more severe cases, EV-D68 has been associated with asthma and wheezing.18
EV-D68 can be found in bodily fluids, such as saliva, mucous, sputum, and feces. It is transmitted through direct contact, including shaking hands; touching contaminated objects or surfaces; changing diapers of an infected person; or drinking water containing the virus. Following infection, the virus can be shed in stools for several weeks and in the respiratory tract for up to 3 weeks. Shedding of EV-D68 can occur even in the absence of symptoms.
INFLUENZA
Influenza is a severe respiratory illness that causes more than 200,000 hospitalizations each year, with 3,000 deaths to 49,000 deaths annually in the US.19 Severe illness related to influenza occurs in those with weak immune systems, such as young children and older adults. Symptoms of influenza include fever, cough, sore throat, muscle aches, and fatigue. It is spread by droplets when a person sneezes or coughs, and can also be spread via contaminated surfaces. The incubation period can be 1 day to 4 days, so individuals can be contagious before the onset of symptoms.20 The Advisory Committee on Immunization Practices strongly recommends annual influenza vaccination for all health care workers, as they might transmit influenza to patients.21 Mandatory health care worker vaccination may be beneficial, but evidence is lacking on patient outcomes related to mandated vaccination.22
STEPS FOR ORAL HEALTH PROFESSIONALS
Oral health professionals must understand how to identify the signs and symptoms of emerging infectious diseases. Quickly identifying patients with infectious diseases is key to preventing transmission. Ensuring thorough questioning of patients through the health history interview, as well as taking vital signs (blood pressure, pulse, respirations, and temperature) are key in the treatment and prevention of infectious diseases. In addition, dental professionals should ensure their vaccinations are up-to-date.21 Lastly, oral health professionals should follow strict infection control procedures with all patients (universal/standard precautions). Frequent hand washing, proper PPE, and safe work practices must be employed at all times to prevent infection. Educating patients about disease transmission is also important. Teaching patients about proper respiratory hygiene, hand washing, disinfection of objects and surfaces, as well as avoiding sick people is another key to disease prevention. The CDC has many resources available such as toolkits, resources, posters, and fact sheets that can be printed and posted in the dental office. Clinicians play a vital role in staying healthy and preventing the spread of infectious diseases.
REFERENCES
- Jones K, Patel N, Levy M, et al. Global trends in emerging disease. Nature. 2008;45:990–994.
- World Health Organization. When Ebola Came Calling: How Communities in Sierra Leone Faced the Challenge. Available at: who.int/csr/disease/ebola/en. Accessed November 22, 2014.
- Feldman H, Geisbert T. Ebola haemorrhagic fever. Lancet. 2011;377:849–862.
- Centers for Disease Control and Prevention. About Ebola. Available at: cdc.gov/vhf/ebola/about.html. Accessed November 22, 2014.
- Streinu-Cercel A. Ebola virus disease—a global threat. Germs. 2014;4:58.
- Centers for Disease Control and Prevention. Ebola Virus Disease Information for Clinicians in U.S. Healthcare Settings. Available at: cdc.gov/vhf/ebola/hcp/clinician-information-us-healthcare-settings.html. Accessed November 22, 2014.
- Centers for Disease Control and Prevention. Checklist for Patients Being Evaluated for EVD in the United States. Available at: cdc.gov/vhf/ebola/hcp/index.html. Accessed November 22, 2014.
- Centers for Disease Control and Prevention. Identify, Isolate, Inform: Emergency Department Evaluation and Management for Patients Who Present with Possible Ebola Virus Disease. Available at: cdc.gov/vhf/ebola/pdf/ed-algorithm-management-patients-possible-ebola.pdf. Accessed November 22, 2014.
- Centers for Disease Control and Prevention. First Ebola Case Diagnosed in the U.S. Available at: cdc.gov/media/release/2014/s930-ebola-confirmed-case.html. Accessed November 22, 2014.
- American Dental Association. Ebola Resources. Available at: ada.org/en/member-center/oral-health-topics/ebola-resources?nav=rotator. Accessed November 22, 2014.
- World Health Organization. Middle East Respiratory Syndrome Coronavirus (MERS-CoV)—Saudi Arabia. Available at: who.int/csr/don/21-november-2014-mers/en/. Accessed November 22, 2014.
- Centers for Disease Control and Prevention. Middle East Respiratory Syndrome (MERS). Available at: cdc.gov/coronavirus/mers/index.html. Accessed November 22, 2014.
- Reusken C, Messadi L, Feyisa A, et al. Geographic distribution of MERS coronavirus among dromedary camels, Africa. Emerg Infect Dis. 2014;20;1370–1374.
- Corman V, Jores J, Meyer B, et al. Antibodies against MERS coronavirus in dromedary camel, Kenya, 1999-2013. Emerg Infect Dis. 2014;20:1319–1322.
- Centers for Disease Control and Prevention. Middle East Respiratory Syndrome (MERS), About MERS. Available at: cdc.gov/coronavirus/mers/about/. Accessed November 22, 2014.
- Centers for Disease Control and Prevention. MERS Transmission. Available at: cdc.gov/coronavirus/MERS/about/transmission.html. Accessed November 22, 2014.
- Centers for Disease Control and Prevention. Respiratory Hygiene/Cough Etiquette in Healthcare Settings Available at: cdc.gov/flu/professionals/infectioncontrol/resphygiene.htm. Accessed November 22, 2014.
- Centers for Disease Control and Prevention. Enterovirus D68. Available at: cdc.gov/non-polio-enterovirus/outbreaks/EV-D68-outbreaks.html. Accessed November 22, 2014.
- Centers for Disease Control and Prevention (CDC). Estimates of deaths associated with seasonal influenza—United States, 1976-2007. MMWR Morb Mortal Wkly Rep. 2010;59;1057–1062.
- Centers for Disease Control and Prevention. Seasonal Influenza (Flu). Available at: cdc.gov/flu/about/disease/spread.htm. Accessed November 22, 2014.
- Advisory Committee on Immunization Practices; Centers for Disease Control and Prevention (CDC). Immunization of health-care personnel recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep. 2011;60:1–45.
- Pitts S, Maruthur N, Millar K, Perl T, Segal J. A systematic review of mandatory influenza vaccination in healthcare personnel. Am J Prev Med. 2014;47:330–340.
From Dimensions of Dental Hygiene. December 2014;12(12):30,32–34.

