Addressing the Silent Epidemic
Advancements in early caries detection and risk assessment can make a difference in the fight against tooth decay.
This course was published in the September 2012 issue and expires September 2015. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss current caries detection strategies.
- Define sensitivity, specificity, and reliability in the context of caries detection devices.
- Explain the tenets of caries risk assessment.
- Identify current caries intervention methods.
CURRENT ARMAMENTARIUM
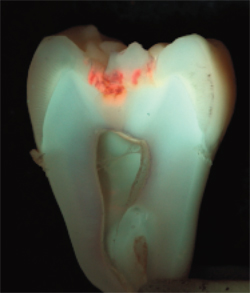
The caries detection strategies in use today are extremely insensitive. Visual examination using an explorer and/or mirror can typically identify caries lesions only when restorative intervention is needed.2 Radiography also leaves much to be desired in specificity. Caries lesions can be seen interproximally on bitewing radiographs only when they are at least half-way through the enamel, histologically.3 This limitation results in missing many lesions at the earliest stages when remineralization techniques might be effective. Transillumination is used to detect caries lesions in anterior teeth, but this technique is limited to identifying lesions that have already progressed through the enamel and are on their way to cavitation.4
SENSITIVITY, SPECIFICITY, AND RELIABILITY
Sensitivity refers to the ability of the device to identify the presence of the condition when it does indeed exist. In other words, does it produce false negatives? By this measure, traditional caries detection tools—including visual examination, radiography, and unaided transillumination—are insensitive.5 Specificity refers to the tool’s ability to accurately identify a condition during detection, ie, does it produce false positives? There are two parts of the specificity equation to consider. The first is what has been detected. If a radiograph or visual examination detects a caries lesion, how certain is the diagnosis?6 The second important part of specificity is whether the detected lesion will progress if left untreated. This is, perhaps, the more difficult challenge of detecting lesions early. The earlier caries lesions are detected, the greater the risk that they may not ever progress to a stage requiring surgical restorative intervention. The naturally- occurring remineralization process might allow routine “reversal” of very small lesions.7 Many experts agree that the risk of employing remineralization techniques on early detected small lesions, some of which may never have progressed, is minimal.8 The greater concern is whether these early lesions are treated with surgical restorative interventions without warrant.
LESION-SPECIFIC DETECTION VS CARIES RISK ASSESSMENT
There are two distinct aspects to caries management.9 The first is the detection, diagnosis, and management of individual caries lesions. This is accomplished with visual examination, radiography, or other means. The lesion is detected, a diagnosis is made, and the lesion is charted as part of the treatment plan for restorative intervention. Separate from this endeavor, each patient must undergo caries risk assessment. This is a much more complex process, yet a very important one. Although only a small percentage of children fall within the highest risk group, they must be identified at a very early stage. By isolating and carefully managing “the caries balance” in high-risk children at a very early stage, the progression of decay can be mitigated.1
CARIES DETECTION VS CARIES DIAGNOSIS
Caries detection must be distinguished from caries diagnosis. With the implementation of new technologies that detect caries lesions at earlier stages, and with technologies that help dental professionals see caries lesions even at currently detectable stages, it is critical to understand that these devices detect, but they do not diagnose. Clinicians make a diagnosis. Information must be gathered from a variety of sources,10 including some of the new technologies that provide important assistance, however, only clinicians make the decision, based on all available data, that caries is present.
A variety of technologies are used in today’s caries detection devices, including light-induced fluorescence (Figure 1), infrared fluorescence, infrared fluorescence combined with photo-thermal radiometry, and AC impedance spectroscopy. Many of these tools use light because the demineralization process changes the visual appearance of enamel. Some fluoresce the enamel in order to collect the emitted frequency, which is then used to determine the level of demineralization. Others calculate the luminescence and heat exhibited after the area is illuminated with a laser light. Measuring the reflectance of light off of the tooth surface is another technique employed. Still others use light transmission and electrical impedance.
The evidence supporting these caries detection devices is mixed.11–13 Many are quite sensitive in their detection abilities, yet are also prone to producing false positives. Some are not able to detect early caries lesions, while others miss caries present around restorations. All of these devices can be successfully used in caries detection but only as adjuncts to other techniques, such as visual examination.
RISK ASSESSMENT TOOLS
A variety of tools are available to assess children’s risk of dental caries. Some gather historical and environmental data and then determine a risk level. Other types employ various forms of technology by assessing one or more distinct outcome measures as validated determinants of risk.14,15
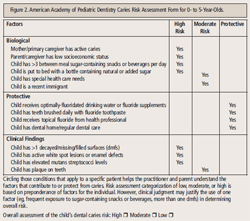
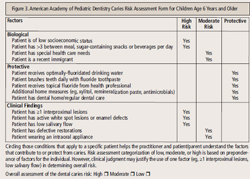
Featherstone1,7,16 and others have developed a risk assessment tool that offers separate sections for adults and children. It uses historical and environmental factors, as well as technology, to assess contributors, such as bacterial counts and salivary flow rates. There is little information validating the use of bacterial counts, salivary flow rates, and buffering capacities in children.8 The American Academy of Pediatric Dentistry (AAPD) has recently published a caries assessment tool (CAT)8 that allows clinicians to assign a relative risk to children by virtue of historical and environmental data collection. Separate forms are available at www.aapd.org for children age 0 to 3 years and 0 to 5 years (Figure 2), as well as those age 6 and older ( Figure 3).
The greatest risk factor for caries is a history of caries. Even if a child has had a single surface caries lesion, the risk for future caries is significantly increased.17 Additionally, a history of caries in the family, particularly in the mother, will increase the child’s caries risk. CAT is a very useful tool in caries risk assessment for children, although it does require time to gather the necessary data.
ACID PRODUCTION DETECTION
Regardless of the quantity or strain of organisms within a plaque biofilm, the biofilm must produce acid when challenged with sucrose in order for the caries process to progress. Therefore, any device that uses technology to assess the acid production potential of the biofilm as an in vitro diagnostic tool might be useful in pediatric dentistry.18
A tool that assesses the acid production potential of biofilm is currently available in Japan. Shimono and his colleagues at Okayama University in Okayama City, Japan, have studied this interesting risk assessment tool and have been able to reliably predict caries risk as measured by the decayed and filled surfaces (df) outcome measure.19–21 The test has successfully forecasted caries experience among toddlers by sampling the biofilm of children as young as 3 and predicting df outcomes in children up to age 10. Additionally, Shimono’s team has shown that aggressive intervention can prevent subsequent caries experience in high-risk children.22,23
Other technologies are currently being developed in the acid production category. When these technologies are validated via caries outcome measures, they may be extremely useful in a variety of environments in the dental office and beyond.24 Pediatricians are now required to perform an oral health assessment of infants at age 6 months.25 Because they see children so often at a very young age (15 times or more before age 3), pediatricians can be important partners in the fight against caries. If technology can provide them with a reliable and rapid screening tool, determining which of the millions of children they see each year need a more immediate referral for intervention and prevention of dental caries can be accomplished.
INTERVENTIONS
There are a variety of intervention measures currently available, and many more are in development.26–28 Fluoride is key to caries intervention. Fluoride varnish, a new member of the preventive armamentarium, might be the precursor to new types of varnish interventions employing other agents instead of or in addition to fluoride.29 Lesion-specific treatments may become available that are professionally applied, in combination with individually tailored self-care programs for the parents and the child.2,18,30–38 By detecting caries lesions and/or caries risk at the earliest stages, families will be better able to manage their children’s oral health in concert with the professional dental team. When technology routinely allows clinicians to inform parents of their child’s risk level, as well as pinpoint specific locations where early caries activity is occurring, families will feel a greater sense of obligation to take part in preventing progression of disease.
Pit and fissure sealants continue to be the most underused preventive measure for children.29 Given that the strong majority of caries lesions occur on the pit and fissure surfaces (vs smooth surfaces), there is a great need to seal out decay in as many children as possible. Because of the variety of excellent materials and techniques available today, it is essential that more practitioners make sealant placement a routine part of caring for children.
CONCLUSION
Dental caries in children was deemed the “silent epidemic” in Oral Health in America: A Report of the Surgeon General published in 2000.29 This epidemic continues in this country as access to care problems remain. In the United States, 80% of dental disease occurs in 25% of the population, and it is this segment that is most often without access to professional dental care. As such, general practitioners and pediatric dental professionals must join forces in providing access to care for all children. With the growing number of courses, educational materials, and efforts to train general dental professionals in the care of pediatric populations, more children should be gaining access to dental care, thus, addressing the “silent epidemic.” Exciting times are ahead in dentistry and in particular, in caring for children. Managing caries as a disease and not merely treating its results is a significant breakthrough. Better and more powerful caries risk assessment tools and detection devices are on the horizon, which should provide more effective therapeutic interventions.
REFERENCES
- Featherstone JD, Adair SM, Anderson MH, et al. Cariesmanagement by risk assessment: consensus statement, April2002. J Calif Dent Assoc. 2003;31:257–269.
- Anusavice KJ. Management of dental caries as a chronicinfectious disease. J Dent Educ. 1998;62:791–802.
- Bottenberg P, Jacquet W, Stachniss V, Wellnitz J, SchulteAG. Detection of cavitated or non-cavitated approximalenamel caries lesions using CMOS and CCD digital X-raysensors and conventional D and F-speed films at differentexposure conditions. Am J Dent. 2011;24:74–78.
- Mitropoulos P, Rahiotis C, Stamatakis H, Kakaboura A.Diagnostic performance of the visual caries classificationsystem ICDAS II versus radiography and micro-computedtomography for proximal caries detection: an in vitro study. JDent. 2010;38:859–867.
- Ekstrand KR, Luna LE, Promisiero L, et al. The reliability andaccuracy of two methods for proximal caries detection anddepth on directly visible proximal surfaces: an in vitro study.Caries Res. 2011;45:93–99.
- Cheng JG, Zhang ZL, Wang XY, Zhang ZY, Ma XC, Li G.Detection accuracy of proximal caries by phosphor plate andcone-beam computerized tomography images scanned withdifferent resolutions. Clin Oral Investig. 2012;16:1015–1021.
- Featherstone JD. The caries balance: contributing factorsand early detection. J Calif Dent Assoc. 2003;31:129–133.
- American Academy of Pediatric Dentistry. Guideline oncaries-risk assessment and management for infants, childrenand adolescents. Chicago: American Academy of PediatricDentistry; 2011.
- Ismail AI. Determinants of health in children and theproblem of early childhood caries. Pediatr Dent.2003;25:328–333.
- Tinanoff N. Caries management in children: decisionmakingand therapies. Compend Contin Educ Dent.2002;23(Suppl):9–13.
- Braga MM, Ekstrand KR, Martignon S, Imparato JC,Ricketts DN, Mendes FM. Clinical performance of two visualscoring systems in detecting and assessing activity status ofocclusal caries in primary teeth. Caries Res. 2010;44:300-308.
- Ferreira Zandona A, Zero DT. Diagnostic tools for earlycaries detection. J Am Dent Assoc. 2006;137:1675-1684.
- Pretty IA. Caries detection and diagnosis: noveltechnologies. J Dent. 2006;34:727-739.
- Barber LR, Wilkins EM. Evidence-based prevention,management, and monitoring of dental caries. J Dent Hyg.2002;76:270–275.
- Tinanoff N, Douglass JM. Clinical decision making forcaries management in children. Pediatr Dent.2002;24:386–392.
- Ching B, Fujioka C. Comprehensive approach to themanagement and prevention of early childhood caries. HawaiiMed J. 2003;62:33–34.
- Pienihakkinen K, Jokela J. Clinical outcomes of risk-basedcaries prevention in preschool-aged children. CommunityDent Oral Epidemiol. 2002;30:143–150.
- Milgrom P, Riedy CA, Weinstein P, Tanner AC, ManibusanL, Bruss J. Dental caries and its relationship to bacterialinfection, hypoplasia, diet,and oral hygiene in 6- to 36-montholdchildren. Community Dent Oral Epidemiol.2000;28:295–306.
- Akyuz S, Kadir T, Erdem H. Dental caries and Cariostat testin preschool children. J Marmara Univ Dent Fac.1997;2:616–620.
- Nishimura M, Bhuiyan MM, Matsumura S, Shimono T.Assessment of the caries activity test (Cariostat) based on theinfection levels of mutans streptococci and lactobacilli in 2- to13-year-old children’s dental plaque. ASDC J Dent Child.1998;65:248–251.
- Tsubouchi J, Yamamoto S, Shimono T, Domoto PK. Alongitudinal assessment of predictive value of a caries activitytest in young children. ASDC J Dent Child. 1995;62:34–37.
- Nishimura M, Oda T, Kariya N, Matsumura S, Shimono T.Using a caries activity test to predict caries risk in earlychildhood. J Am Dent Assoc. 2008;139:63–71.
- Rodis OM, Shimono T, Matsumura S, et al. Cariogenicbacteria and caries risk in elderly Japanese aged 80 and olderwith at least 20 teeth. J Am Geriatr Soc.2006;54:1573–1577.
- Weinstein P, Smith WF, Fraser-Lee N, Shimono T, TsubouchiJ. Epidemiologic study of 19-month-old Edmonton, Albertachildren: caries rates and risk factors. ASDC J Dent Child.1996;63:426–433.
- Hale KJ, American Academy of Pediatrics Section onPediatric Dentistry. Oral health risk assessment timing andestablishment of the dental home. Pediatrics.2003;11:1113–1116.
- Amin MS, Harrison RL, Benton TS, Roberts M, Weinstein P.Effect of povidone-iodine on Streptococcus mutans in childrenwith extensive dental caries. Pediatr Dent. 2004;26:5–10.
- Fadavi S. Management of early childhood caries. GenDent. 2003;51:38–40.
- Ching B, Fujioka C. Comprehensive approach to the management and prevention of early childhood caries. HawaiiDent J. 2003;34:11–12.
- US Department of Health and Human Services. OralHealth in America: A Report of the Surgeon General.Rockville, Md: US Department of Health and Human Services,National Institute of Dental and Craniofacial Research,National Institutes of Health; 2000.
- Caufield PW, Dasanayake AP, Li Y. The antimicrobial approach to caries management. J Dent Educ.2001;65:1091–1095.
- Caufield PW, Griffen AL. Dental caries. An infectious and transmissible disease. Pediatr Clin North Am.2000;47:1001–1019.
- Caufield PW, Dasanayake AP, Li Y, Pan Y, Hsu J, HardinJM. Natural history of Streptococcus sanguinis in the oral cavity of infants: evidence for a discrete window of infectivity.Infect Immun. 2000;68:4018–4023.
- Li Y, Wang W, Caufield PW. The fidelity of mutans streptococci transmission and caries status correlate with breast-feeding experience among Chinese families. CariesRes. 2000;34:123–132.
- Caufield PW. Dental caries—a transmissible and infectious disease revisited: a position paper. Pediatr Dent.1997;19:491–498.
- Li Y, Caufield PW. The fidelity of initial acquisition of mutans streptococci by infants from their mothers. J DentRes. 1995;74:681–685.
- Dasanayake AP, Caufield PW, Cutter GR, Stiles HM.Transmission of mutans streptococci to infants following shortterm application of an iodine-NaF solution to mothers’dentition. Community Dent Oral Epidemiol.1993;21:136–142.
- Caufield PW, Cutter GR, Dasanayake AP. Initial acquisitionof mutans streptococci by infants: evidence for a discrete window of infectivity. J Dent Res. 1993;72:37–45.
- Caufield PW, Walker TM. Genetic diversity withinStreptococcus mutans evident from chromosomal DNA restriction fragment polymorphisms. J Clin Microbiol.1989;27:274–278.
From Dimensions of Dental Hygiene. September 2012; 10(9): 42-45.