5 Myths About Periodontal Instrumentation
Magnified viewing of subgingival and root areas debunks some common theories about root instrumentation technique.
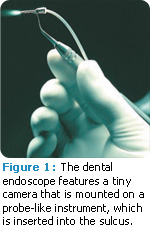
The use of the dental endoscope has allowed dental professionals to actually see what they are instrumenting for the first time. What is revealed by the dental endoscope challenges many of the current beliefs held in modern periodontal instrumentation.
Myth #1
The first myth is that flap surgery is always necessary to gain access for removal of subgingival calculus deeper than 4 mm or 5 mm. Many articles discuss the limitations of nonsurgical therapy in the removal of subgingival calculus.2-16 Dental hygienists often believe they are limited by how deep they can insert an instrument into the pocket and by their ability to access furcations and concavities, and around line angles. The dental endoscope, however, demonstrates that these areas can be reached. Clinicians are hampered by the diameter of the space being instrumented (eg, narrow furcations), and instrument design. Thin ultrasonic inserts/tips (UITs) or micro mini curets are sometimes the only choice for instrumenting these tight root areas.
The dental endoscope’s high magnification ensures that even miniscule pieces of embedded calculus can be seen and removed. At times, the camera must be removed from the pocket to allow for insertion of the scaling instrument. Using this “view, instrument, view” technique does not allow for observation while working, but the ability to insert the camera to see the area after instrumentation allows for the thorough removal of subgingival calculus—and, in some cases, may eliminate the need for flap surgery.
Myth #2
The second misconception is that root planing is not necessary to achieve complete removal of calculus. The philosophy of using root planing to achieve glassy, smooth roots came into question during the late 1990s.
Some currently used dental hygiene textbooks advise abandoning root planing in favor of the less invasive root debridement.17 More emphasis is placed on saving cementum than in removing calculus, even though most pocket closure, following post-nonsurgical therapy, is accomplished by long junctional epithelial attachment, and not through direct fibers into cementum.18
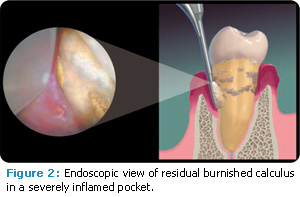
The dental endoscope reveals that significant calculus remains on the root after closed debridement that is not detectable with an explorer (Figure 2). This calculus contains lacuna that harbor microorganisms, including bacteria that initiate periodontal infections.19 Removal of bacteria-laden calculus is conducive to healing and should remain the primary goal of periodontal instrumentation. Failure to remove undetected calculus impedes healing of the pocket, resulting in the need for further root planing or periodontal surgery.20
In my opinion, dental hygienists must remove as much calculus as possible because it is key to pocket reduction and healing. Roughness remaining on the root should be regarded as potential calculus.
When residual calculus is left on the root, the healing phase is greatly affected. In many instances, pocket depths will persist, and unfortunately, these areas are often not reevaluated or the bleeding on probing is mistakenly blamed on inadequate oral hygiene. Dental hygienists who work without an endoscope must assume that calculus remains even if it is undetectable with an explorer. Retreating the area with additional instrumentation is a prudent next step.
Myth #3
Another common myth is that the smoothness of roots (felt with an explorer, probe, or curet) means they are calculus free. The dental endoscope clearly illustrates that calculus is missed following closed procedure scaling. It can be microscopically embedded into the root and, therefore, undetectable by an explorer. Restorations, crown margins, cementoenamel junctions, grooves, and depressions are other areas that commonly harbor calculus dismissed as roughness.
The feeling of smoothness is not an accurate predictor of calculus removal.21 Dental hygienists who are root planing without a dental endoscope, however, are limited in their ability to evaluate calculus removal. While tactile smoothness and healing results, such as lack of bleeding on probing, are the most common factors used to evaluate initial periodontal therapy, they are not necessarily accurate when deciding whether calculus removal is complete.
Myth #4
This myth may be the most dangerous of all: Healing will occur even when calculus is still present on the root. Dental hygienists using the dental endoscope know that pockets heal when complete calculus remova has been achieved. Periodontal practices regularly receive referrals from general dental offices because of residual pocket depth with bleeding, following root planing procedures. With the use of a dental endoscope, the cause of these residual pockets, usually calculus, can be seen and removed. Pocket reduction occurs once calculus is thoroughly removed.22
Only two articles reported formation of a long junctional epithelial attachment on embedded calculus in a few sites on monkeys.23,24 There are no studies to date that demonstrate soft tissue attachment to residual calculus has ever occurred in humans. Studies of endoscopically treated teeth by Wilson25 and Checchi26 show that inflammation on the pocket wall and bleeding on probing are present when calculus is left on the root surface.
Myth #5
The widely held belief that ultrasonic scaling of subgingival calculus is more efficient than using hand instruments is a myth. Studies show that ultrasonic instrumentation can be completed more quickly than hand instrumentation in the initial treatment of periodontally-involved teeth.27,28 In order to compare efficiency, however, the actual finished root surfaces should be closely examined.
For clinicians experienced with hand instrumentation, using a sharp curet can be faster and more efficient for subgingival calculus removal than using a UIT. There are situations when using a fine UIT proves too tedious for tenacious calculus removal. For example, when instrumenting with an ultra thin UIT on medium power, it must be pressed against the outer edge of the calculus with a probe-like stroke until tiny crystalline fragments of the calculus break free. After removing this exterior portion of calculus, the embedded bottom layer is exposed and can be easily seen with the endoscope. This bottom section of calculus is interlocked into the root surface, and removing it can be an intricate and lengthy process. For some endoscopy clinicians, switching to a hand instrument and using the “view, instrument, view” technique saves time. However, this technique can remove more root structure than necessary, so caution must be used.
Diamond-coated ultrasonic tips can improve the speed of calculus removal, but the tip must be deactivated and quickly moved off the root once the calculus is gone or the surface might be gouged. Hand instruments can and do work efficiently, but are dependent on the clinician’s skill and experience.
Ultimately, a healthy intact periodontium is the goal of periodontal instrumentation. The dental endoscope increases the possibility of achieving completely clean root surfaces, whether hand or power instrumentation is used.
REFERENCES
- Stambaugh RV, Myers G, Ebling W, Beckman B, Stambaugh KA. Endoscope visualization of the subgingival dental sulcus and tooth root surface. J Periodontol. 2002;73:374–382.
- Adriaens PA, Adriaens LM. Effects of nonsurgical periodontal therapy on hard and soft tissues. Periodontol 2000. 2004;36:121–145.
- Claffey N, Polyzois I, Ziaka P. An overview of nonsurgical and surgical therapy. Periodontol 2000. 2004;36:35–44.
- Cobb CM. Non-surgical pocket therapy: mechanical. Ann Periodontol. 1996;1:443–490.
- Caffesse RG, Sweeney PL, Smith BA. Scaling and root planing with and without periodontal flap surgery. J Clin Periodontol. 1986;13:205–210.
- Brayer WK, Mellonig JT, Dunlap RM, et al. Scaling and root planing effectiveness: the effect of root surface access and operator experience. J Periodontol. 1989;60:67–72.
- Buchanan SA, Robertson PB. Calculus removal by scaling/root planing with and without surgical access. J Periodontol. 1987;58:159–163.
- Nagy RJ, Otomo-Corgel J, Stambaugh R. The effectiveness of scaling and root planing with curets designed for deep pockets. J Periodontol. 1992;63:954–959.
- Otero-Cagide FJ, Long BA. Comparative in vitro effectiveness of closed root debridement with fine instruments on specific areas of mandibular first molar furcations. II. Furcation area. J Periodontol. 1997;68:1098–1101.
- Waerhaug J. Healing of the dento-epithelial junction following subgingival plaque control. II. As observed on extracted teeth. J Periodontol. 1978;49:119–134.
- Wylam JM, Mealey BL, Mills MP, et al. The clinical effectiveness of open versus closed scaling and root planing on multi-rooted teeth. J Periodontol. 1993:64:1023–1028.
- Rabbani GM, Ash MM Jr, Caffesse RG. The effectiveness of subgingival scaling and root planing in calculus removal. J Periodontol. 1981;52:119–123.
- Rateitschak-Plüss EM, Schwarz JP, Guggenheim R, et al. Non-surgical periodontal treatment: where are the limits? An SEM study. J Clin Periodontol. 1992;19:240–244.
- Sherman PR, Hutchens LH Jr, Jewson LG, et al. The effectiveness of subgingival scaling and root planing. I. Clinical detection of residual calculus. J Periodontol. 1990;61:3–8.
- Matia JI, Bissada NF, Maybury JE, Ricchetti P. Efficiency of scaling of the molar furcation area with and without surgical access. Int J Periodontics Restorative Dent. 1986;6:24–35.
- Stambaugh RV, Dragoo M, Smith DM, Carasali L. The limits of subgingival scaling. Int J Periodontics Restorative Dent. 1981;1:30–41.
- Neild-Gehrig JS. Fundamentals of Periodontal Instrumentation and Advanced Root Instrumentation. 6th ed. Baltimore: Lippincott Williams & Wilkins; 2007.
- Polson AM, Caton J. Factors influencing periodontal repair and regeneration. J Periodontol. 1982;53:617–625.
- Moolya NN, Thakur S, Ravindra S, Setty SB, Kulkarni R, Hallikeri K. Viability of bacteria in dental calculus—A microbiological study. J Indian Soc Periodontal. 2010;14:222–226.
- Wilson TG Jr, Carnio J, Schenk R, Myers G. Absence of histologic signs of chronic inflammation following closed subgingival scaling and root planing using the dental endoscope: human biopsies—a pilot study. J Periodontol. 2008;79:2036–2041.
- Sherman PR, Hutchens LH Jr, Jewson LG, Moriarty JM, Greco GW, McFall WT Jr. The effectiveness of subgingival scaling and root planning. I. Clinical detection of residual calculus. J Periodontol. 1990;61:3-8.
- Stambaugh RV. A clinician’s 3-year experience with perioscopy. Compend Contin Educ Dent. 2002;23:1061–1070.
- Blomlöf L, Friskopp J, Appelgren R, Lindskog S, Hammarström L. Influence of granulation tissue, dental calculus and contaminated root cementum on periodontal wound healing. An experimental study in monkeys. J Clin Periodontol. 1989 Jan;16(1):27-32.
- Listgarten MA, Ellegaard B. Electron microscopic evidence of a cellular attachment between junctional epithelium and dental calculus. J Periodontal Res. 1973;8:143–150.
- Wilson TG, Harrel SK, Nunn ME, Francis B, Webb K. The relationship between the presence of tooth-borne subgingival deposits and inflammation found with a dental endoscope. J Periodontol. 2008;79:2029–2035.
- Checchi L, Montevecchi M, Checchi V, Zappulla F. The relationship between bleeding on probing and subgingival deposits. An endoscopical evaluation. Open Dent J. 2009;3:154–160.
- Wennström JL, Tomasi C, Bertelle A, Dellasega E. Full-mouth ultrasonic debridement versus quadrant scaling and root planing as an initial approach in the treatment of chronic periodontitis. J Clin Periodontol. 2005;32:851–859
- Yukna RA, Scott JB, Aichelmann-Reidy ME, LeBlanc DM, Mayer ET. Clinical evaluation of the speed and effectiveness of subgingival calculus removal on single-rooted teeth with diamond-coated ultrasonic tips. J Periodontol. 1997;68:436–42
From Dimensions of Dental Hygiene. November 2011; 9(11): 68, 70.

