 PORTRA/E+/GETTY IMAGES PLUS
PORTRA/E+/GETTY IMAGES PLUS
Moving Toward Patient Concordance With Shared Decision Making
When the patient-clinician relationship is established and shared decision making is incorporated, patients are well prepared to meet their oral healthcare goals.
The evidence supporting patient-centered care encourages a shift in oral health professionals’ thinking and methods. Healthcare systems are moving toward value-based healthcare models focused on patient-centered care and improved patient outcomes and satisfaction.1,2 The movement toward evaluating improved patient outcomes signifies that now, more than ever, dental hygienists play an important role in improving patients’ oral health outcomes.
Patient compliance is also critical to improving patient outcomes. Defined as “the extent to which the patient’s behavior matches the healthcare professional’s recommendations,” patient compliance is always the goal but can be difficult to achieve.3–5 Oral health professionals have limited control over most factors that affect compliance. Lee et al4 estimate that half of dental patients are unsuccessful at completing recommended treatment.
OVERCOMING COMPLIANCE CHALLENGES
To effectively address the factors affecting patient compliance, there must be a shift from patient compliance to patient concordance. Patient compliance insinuates that the oral health professional recommends treatment or behavior change and patients are “compliant” if they follow through with the recommendations.
Concordance, on the other hand, refers to an agreement between the healthcare professional and the patient after thorough discussion during which the healthcare professional respects and regards the patient’s feelings, beliefs, and abilities to carry out the treatment.3,6 To shift to a patient concordance mindset, the patient must be included in the care planning process.
Shared decision making (SDM) is considered the core of patient-centered care. Based on the premise of autonomy in which the patient is respected as the expert of his/her own life and the healthcare professional is the expert in the treatment options, SDM promotes the patient’s ownership and responsibility in improving his/her own health.7 The key concepts of SDM, as modified from Godolphin,8 are:
- Create a relationship with the patient.
- Discover the patient’s preferred method of receiving information.
- Determine the patient’s ability, confidence, and willingness to participate in the decision-making process.
- Confirm and acknowledge the patient’s goals, perceptions, standards, suggestions, and hesitations about all treatment options.
- Analyze the patient’s suggestions and knowledge of treatment options and assess current evidence regarding care specific to that patient.
- Provide evidential support and pros and cons for each treatment option during case presentation and consider how the delivery of the information may affect the patient’s decision. Compare and contrast the care options in relation to what is important to the patient in their life and goals.
- Openly discuss and debate choices to respectfully come to a joint or shared decision.
- Decide on an individualized treatment plan and continually check in and evaluate progress at each step of the plan completed.
Shared decision-making aids can assist both patients and providers in the communication process.
SHARED DECISIONS MAKING IN PATIENT-CENTERED CARE
Effective communication between the dental hygienist and the patient is the foundation of patient-centered care. Creating trust and rapport depends on empathetic and compassionate communication. A study that assessed empathy and patient satisfaction demonstrated that the perceived empathy of the healthcare provider was proportionally related to patient satisfaction and compliance.9 Getting to know patients’ attitudes, behaviors, beliefs, lifestyles, and experiences through open, nonjudgmental communication can support the development of a trusting, empathetic relationship between providers and patients.8–10
SHARED DECISIONS MAKING AIDS
SDM aids can assist both patients and providers in the communication process.11 Examples of SDM aids are treatment vs no treatment comparisons, visual images comparing treatment outcomes, decision boards, and detailed care plans in case presentation.12–15 A Cochrane review evaluated the existing evidence on the effectiveness of SDM use in healthcare.12 This systematic review included 87 studies; 15 measured SDM effectiveness through evaluations completed by both healthcare professionals and patients. The results confirmed that assessments provided by patients are most often utilized to determine the level of patient involvement in the decision-making process and outcomes are impacted by whether the evaluations are based on provider or patient perspectives. The review concluded that clinical indicators are poor representations of what patients truly value; therefore, the only way to assess the value of SDM and the patient’s ability to actively participate in SDM is to ask patients themselves.
SDM can be helpful with tobacco cessation, a common challenge for many healthcare professionals, including dental hygienists. A systematic review of studies on tobacco cessation measured abstinence, quit attempts, knowledge of cessation methods, and decision quality through the use of various SDM aids.14 Results showed that decisional aids can improve cessation knowledge and increase attempts to quit. Dental hygienists and dentists are well positioned to support patients’ cessation goals and should consider using SDM aids to facilitate concordance.
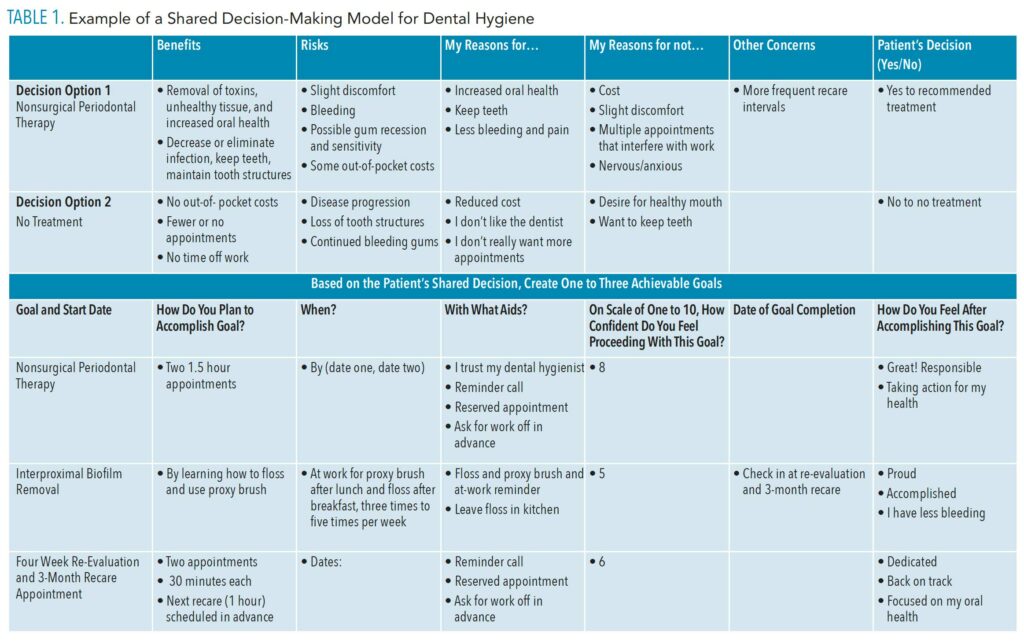
A randomized controlled trial looked at the use of a decision board as an SDM aid in endodontics.15 The experimental group was educated using a written decision board and visual aids that included pictures and diagrams outlining all treatment options, risks vs benefits, prognoses, and associated costs. The control group was educated through standard discussion. The study measured knowledge level, satisfaction, and anxiety in both groups through the administration of a brief questionnaire. The results demonstrated a statistically significant increase in knowledge level among the group that was educated with SDM. Table 1 (page 17) provides an example of a versatile aid that could be used for periodontal and self-care decision making.
CONCLUSION
Patient concordance requires a shift in dental hygiene care planning and case presentation to include SDM. This shift is well supported by patient-centered care and SDM literature. Although many factors affect patient concordance, if oral health professionals focus on the key characteristics of SDM, concordance is achievable. When the patient-clinician relationship is established and SDM is incorporated, the patient should feel empowered and capable of accomplishing his or her treatment and oral healthcare goals. Decision aids may assist in the implementation of SDM.
REFERENCES
- New England Journal of Medicine Catalyst. What is value-based healthcare? Available at: catalyst.nejm.org/doi/full/10.1056/CAT.17.0558#:~:text=Value%2Dbased%20healthcare%20is%20a,based%20on%20patient%20health%20outcomes. Accessed June 13, 2021.
- Ahmady EA, Pakkhesal M, Zafarmand AH, Lando HA. Patient satisfaction surveys in dental school clinics: a review and comparison. J Dent Ed. 2014;79:388–393.
- Horne R, Weinman J, Barber N, Elliott R, Morgan M. Concordance, adherence and compliance in medicine taking. Report for the National Co-ordinating Centre for NHS Service Delivery and Organisation R & D 2005. Available at: researchgate.net/publication/271443859_Concordance_ Adherence_and_Compliance_in_Medicine_Taking. Accessed June 13, 2021.
- Lee CT, Huang HY, Sun TC, Karimbux N. Impact of patient compliance on tooth loss during supportive periodontal therapy: a systematic review and meta-analysis. J Dent Res. 2015;94:777–786.
- Bugler ME, White KM, Robinson NG. The role of self-efficacy in dental patients’ brushing and flossing: testing an extended Health Belief Model. Patient Educ Couns. 2010;78:269–272.
- Dickinson D, Wilkie P, Harris M. Taking medicines: concordance is not compliance. Brit Med J. 1999;319:787.
- Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1:189–199.
- Godolphin W. Shared-decision-making. Healthc Q. 2009;12 Spec No Patient:e186–190.
- Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27:237–251.
- Freeman R. The determinants of dental health attitudes and behaviours. Brit Dent J. 1999;187:15–18.
- British Medical Journal, Drug and Therapeutics Bulletin. An introduction to patient decision aids. Available at: bmj.com/content/347/bmj.f4147. Accessed June 13, 2021.
- Légaré F, Adekpedjou R, Stacey D, et al. Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2018;7:CD006732.
- World Health Organization. Tobacco. Available at: who.int/news-room/fact-sheets/detail/tobacco. Accessed June 13, 2021.
- Moyo F, Archibald E, Slyer JT. Effectiveness of decision aids for smoking cessation in adults: a quantitative systematic review. JBI Database System Rev Implement Rep. 2018;16:1791–1822.
- Johnson BR, Schwartz A, Goldberg J, Koerber A. A chairside aid for shared-decision making in dentistry: a randomized controlled trial. J Dent Educ. 2006;70:133–141.
From Dimensions of Dental Hygiene. July 2021;19(7):16-18.

