
Improving the Nonsurgical Treatment of Periodontitis
Modifying risk factors, facilitating decisions about the use of antibiotics, and recommending appropriate oral hygiene measures are the keys to successful treatment.
This course was published in August 2019 and expires August 2022. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the goals of nonsurgical periodontal therapy (NSPT).
- Discuss the seven-step protocol for NSPT.
- List the challenges that may arise when implementing this protocol and note when a surgical approach should be considered.
Nonsurgical therapy is considered the gold standard for the initial treatment of inflammatory periodontal disease. Indeed, nonsurgical treatment involving meticulous scaling and root planing has been extensively documented and has been shown to be a highly predictable and successful therapy.1 The main goals of nonsurgical periodontal therapy (NSPT) are to remove and control supra- and subgingival microbial biofilms, eliminate and control inflammation, and eliminate and control systemic and local risk factors that contribute to disease development and progression. Depending on the degree of bony involvement, effective NSPT may minimize or eliminate the need for surgical intervention. Hence, the seven-step protocol described here (Figure 1) will enable clinicians to identify and modify local and systemic risk factors, facilitate decisions about the use of systemic or locally delivered antibiotics, and prescribe appropriate oral hygiene measures. However, not all periodontal diseases can be successfully managed with a nonsurgical approach.
THE SEVEN-STEP PROTOCOL
Step 1. Controlling Systemic Risk Factors. Several risk factors have well established associations with both periodontal and systemic diseases, such as diabetes, smoking, stress, immunodeficiency, medications, obesity, hormones, and nutrition. For optimal treatment results, systemic risk factors must be modified or eliminated. Some are under the patient’s control, and may, therefore, require lifestyle changes to achieve significant modification. Other more subtle systemic and environmental issues may also need to be addressed to achieve optimal results.
Diabetes: A bidirectional relationship between diabetes and periodontitis was proposed by Löe2 and has been confirmed repeatedly by other investigators.3 For a patient with diabetes or a patient suspected of prediabetes, it is imperative to know the individual’s glycosylated hemoglobin level (HbA1c) prior to initiating periodontal treatment. Patients with diabetes and HbA1c values less than 7% are considered well controlled and can be treated in similar fashion to the general population; however, even in these patients, the possibility of delayed healing and infection should be discussed prior to treatment. Patients with diabetes that is poorly controlled should be referred to a medical provider for better metabolic control prior to initiating periodontal therapy. Mutual management of both chronic diseases is vital to attaining stable periodontal health, as well as optimal metabolic control.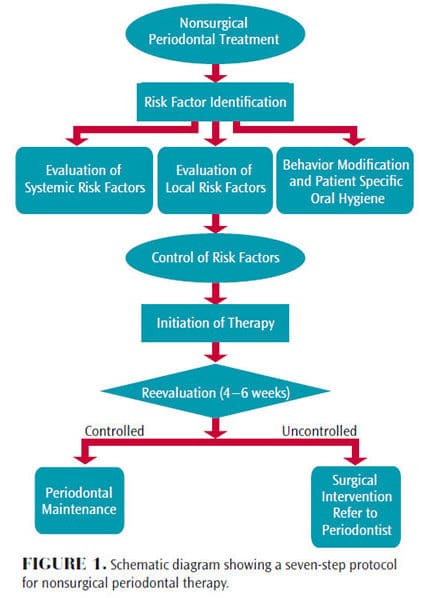
Smoking: Smokers have a twofold to fourfold greater risk of developing periodontitis.4 In clinical studies, patients are generally stratified based on the number of cigarettes smoked per day; for example, light (< 10 cigarettes/day), moderate (10 to 19 cigarettes/day), or heavy smokers (≥ 20 cigarettes/day). The risk of developing periodontitis is positively correlated to the number of cigarettes smoked. Prior to initiating nonsurgical periodontal therapy, patients who smoke should be educated about the effects of smoking and encouraged to quit. Studies have reported that smokers exhibit less reduction in subgingival microbial loads and probing depths during NSPT than nonsmoking patients.5,6
Medications: Roughly 6% to 15% of patients taking a calcium channel blocker, 25% to 30% receiving immunosuppressants, and 50% being treated with antiepileptic drugs will exhibit some degree of drug-induced gingival enlargement.7 Clinical symptoms of gingival overgrowth are generally seen 1 month to 3 months after initiating drug therapy. For these patients, the medical provider should be consulted to explore the possibility of changing to a different drug category to minimize gingival enlargement.8 In addition, thorough oral hygiene instruction and appropriate periodontal maintenance intervals need to be established.9
Obesity: The World Health Organization10 defines obesity as having a body mass index (BMI) ≥ 30 kg/m2. Obesity and BMI are positively correlated to an increased incidence of periodontitis. Further, it appears that obesity can adversely impact periodontal treatment outcomes.11 Gorman et al12 reported that as BMI increases by one unit, the rate of alveolar bone loss increases by 5%. Consequently, periodontal patients should be encouraged to adapt a healthy lifestyle to maintain an ideal BMI of < 25kg/m2. Calculation and recording of BMI needs to be incorporated in the comprehensive initial evaluation.
Nutrition: The role of nutrition is well documented in management of chronic systemic illnesses and should be extended to include periodontitis. A diet plan should include high fiber, low carbohydrate,13 high protein,13 Omega-3 fatty acids, micronutrients (such as vitamins D, C and B12), and antioxidants (eg, vitamin A, folic acid, and beta-carotene) to optimize periodontal health. Chapple et al14 demonstrated a statistically significant relationship between the prevalence of periodontal disease and low serum vitamin C levels. Levine et al15 reported that 200 mg of vitamin C per day could help maintain periodontal health. Compared to a control group, in a study of patients in a periodontal maintenance program, subjects taking ≥ 1,000 mg of calcium and ≥ 400 IU of vitamin D had more shallow probing depths and less gingival inflammation.16
Merchant et al17 noted that higher intake of whole grains is associated with a 23% decreased risk for developing periodontitis. Whole grains have a high fiber content that, in turn, may help decrease inflammation and improve host insulin sensitivity. Carbohydrates have the opposite effect in that high intake of carbohydrates is associated with increased gingival inflammation.18 According to Al-Zahrani et al,19 individuals with a normal BMI, habit of good exercise, and a healthy diet are 40% less likely to develop periodontitis than at-risk groups.
Step 2. Eliminating Local Risk Factors. A variety of tooth-related local risk factors can predispose a patient to developing an inflammatory periodontal lesion. These can be grouped into three general categories: anatomical, tooth position, and iatrogenic. While local risk factors are not considered to be a direct cause of periodontitis, they contribute to biofilm development, increased biofilm pathogenicity, and calculus retention. Local risk factors can be modified and/or eliminated—and, in fact, periodontal therapy should not be considered complete until all local risk factors have been addressed.
Anatomical risk factors may include cervical enamel projections and enamel pearls, furcations, root grooves and flutings, untreated caries, frenulum attachments, and gingival recession. Risk factors involving tooth position are likely to include malposition, crowding, tipping, and migration of teeth. Abnormal occlusal forces resulting from traumatic occlusal relationships and bruxism and clenching habits also fall into this category. Lastly, iatrogenic risk factors might involve an ill-fitting removable prostheses, temporary and permanent restorations with rough and inadequate contours, overhangs, open margins, and open contacts.20–22
Step 3. Behavior Modification. Effective plaque control is a requirement in nonsurgical and surgical periodontal therapy. Assessment, motivation, and reinforcement of oral hygiene should be performed at each appointment. Recent research evaluating the association between oral hygiene and periodontitis showed that the risk of periodontitis increased by twofold to fivefold in patients with poor oral hygiene.23 Self-care instructions need to be personalized and should be recommended based on the severity of the patient’s periodontal status.
For healthy patients or those with gingivitis, effective brushing, tongue cleaning, interdental cleaning, and use of an antiseptic mouthrinse should be sufficient (Table 1). Given the prodigious bacterial population of the dorsal tongue surface, daily cleaning of the tongue has received little attention in the literature. Matsui et al24 recommended the practice of toothbrushing and tongue cleaning to effectively decrease the oral microbial load. Tongue scraping reportedly produces a statistically significant reduction in oral malodor, as compared to mechanical brushing of the teeth.25 Patients with plaque-induced gingivitis should be counseled that good oral hygiene can restore gingival health without significant periodontal treatment. If plaque is not controlled, however, the inflammatory lesion may progress to a more severe stage of periodontal disease. Adjunctive use of a chlorhexidine oral rinse can be beneficial, as research has shown it contributes to an approximate 33% reduction in plaque and 26% reduction in gingivitis.26
Periodontitis is characterized by gingival inflammation and loss of alveolar bone. In moderate to severe stages, gingival recession, loss of interproximal papilla, tooth mobility, and furcation involvement may also be clinical features. For patients with moderate to severe disease, toothbrushing and flossing alone are inadequate to control biofilm (Table 1). When compared to flossing, interdental brushes have been shown to decrease gingival inflammation by 52% and to be more effective in controlling interproximal plaque accumulation in patients with periodontitis.27 In patients with moderate or severe periodontitis, flossing is less effective due to loss of papillary guidance. Oral irrigators are reported to be effective in reducing gingival inflammation.28 As with any oral hygiene device, recommendations should be based on the individual needs of the patient.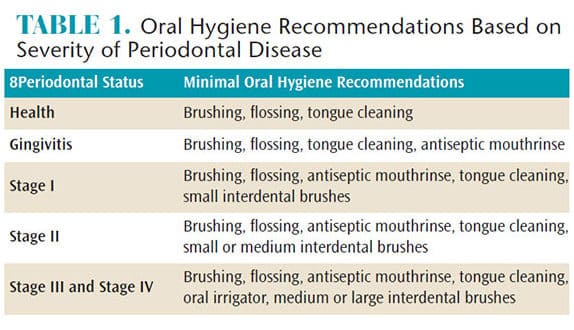
Step 4. Scaling and Root Planing. Meticulous scaling and root planing is the most critical component of initial periodontal therapy. The primary goals of scaling and root planing are to significantly reduce or eliminate subgingival microbial loads, remove subgingival calculus, remove soft and diseased cementum, and smooth roughened root surfaces.1,29 A systematic review1 reported that average improvement in probing depth following scaling and root planing was 1.29 mm in pockets that had an initial probing depths of 4 mm to 6 mm, and 2.16 mm in pockets of ≥ 7 mm. Gains in clinical attachment levels (CAL) averaged 0.55 mm and 1.19 mm for initial probing depths of 4 mm to 6 mm and ≥ 7 mm, respectively. In most forms of periodontitis, scaling and root planing is highly effective in controlling the signs of periodontal inflammation. However, surgical intervention may be required to definitively treat the bony defects often associated with the moderate and severe stages of periodontitis.
Step 5. Antimicrobials. The adjunctive use of systemic antibiotics with scaling and root planing is known to yield a statistical difference, but arguably not a clinically significant difference. In a consensus report, Sanz and Teughels30 suggested the following guidelines regarding the use of systemic antibiotics:
- Systemic antibiotics are not necessary for most patients with periodontitis
- Systemic antibiotics may benefit specific patient groups or defined conditions (eg, Stage III or Stage IV)
- If used as part of a treatment protocol for periodontitis, systemic antibiotics should be used in conjunction with scaling and root planing
- Indirect evidence suggests that for optimal clinical results, systemic antibiotics should be used at the time of scaling and root planing, and all treatment should be completed within 7 days
- The use of systemic antibiotics should be restricted
This cautionary note regarding restricted use of systemic antibiotics is supported by a 2015 American Dental Association statement of clinical guidelines and results noting the increasing emergence of microbial antibiotic resistance.31
Reporting on the potential benefits of topical antiseptic agents (such as 10% povidone iodine) as an adjunct to mechanical debridement, Slots32 noted that it is important to maintain a tissue contact time of 5 minutes to 7 minutes to obtain the optimal antimicrobial effect. Reported benefits from subgingival iodine application include significantly greater reductions in probing depth and putative periodontal pathogen counts, as well as gains in CAL.33,34
Studies that have evaluated the use of locally delivered antimicrobials—such as chlorhexidine chips, doxycycline hyclate gel and minocycline spheres—report modest clinical benefits. Whether the benefit is clinically significant depends chiefly on expert opinion and not statistical evidence.31,35 That noted, locally delivered antimicrobials have some use in medically compromised patients, such as individuals with brittle or marginally controlled diabetes, those undergoing kidney dialysis or active intravenous bisphosphonate therapy, and patients with mental disabilities that impair effective oral hygiene.
Step 6. Reevaluation. Clinicians are advised that reevaluation is not the end-point of active periodontal therapy—it is part of a decision matrix. Periodontal status should be thoroughly reassessed at 4 weeks to 6 weeks following the nonsurgical phase of treatment, as the greater part of healing is completed by 6 weeks, but collagen maturation might continue for up to 9 months.35 Post-therapy reevaluation is a critical step in determining the status of gingival inflammation, oral hygiene and healing. Ideal end points for nonsurgical therapy include a decreasing plaque index ≤ 10%, bleeding on probing ≤ 20%, probing depths ≤ 4 mm, mean gain and stability of CAL, maintenance of alveolar bone height, and preservation of form and function of dentition.36
Reevaluation provides an opportunity to determine if the patient’s periodontal health is stable enough for a periodontal maintenance program, or whether further therapy is required. Additional treatment may involve reinforcement of oral hygiene techniques, nonsurgical retreatment of teeth with no intrabony defects, or surgical intervention.
Step 7. Periodontal Maintenance. Achieving long-term periodontal stability requires an effective periodontal maintenance program and patient compliance. Maintenance generally includes a reevaluation to determine the patient’s periodontal status, evaluation of systemic and local risk factors, supragingival scaling and polishing, scaling and root planing of residual probing depths—particularly those that exhibit bleeding on probing. The interval between periodontal maintenance appointments should be customized for each patient, based on local and systemic risk factors, severity and extent of periodontal disease, rate of disease progression, and patient compliance. The standard of care for patients who have received definitive treatment for chronic or aggressive periodontitis is a 3-month maintenance interval; however, stable patients can be appointed for longer intervals.
CONCLUSION
Reevaluation of treatment response, determination of a patient-specific periodontal maintenance interval, and gaining patient compliance are necessary to maintain periodontal health. Even with optimal care, however, up to 10% of patients may not exhibit the expected response to nonsurgical therapy, and may thus require more aggressive treatment.
ACKNOWLEDGEMENT
Bharathi Devi Myneni, BDS, would like to thank Eugene C. Skourtes, DMD, and Kristen Simmons, RDH, MBA, of Willamette Dental Group for their help with this manuscript.
REFERENCES
- Cobb CM. Nonsurgical periodontal therapy: mechanical. Annals of Periodontol. 1996;1:443–490.
- Löe H. Periodontal disease. The sixth complication of diabetes mellitus. Diabetes Care. 1993;16: 329–334.
- Kumar M, Mishra L, Mohanty R, Nayak R. Diabetes and gum disease: the diabolic duo. Diabetes Metabo Syndr. 2014;8:255–258.
- Tomar SL, Asma S. Smoking-attributable periodontitis in the United States: findings from NHANES III. National Health and Nutrition Examination Survey. J Periodontol. 2000;71:743–751.
- Van der Velden U, Varoufaki A, Hutter JW, et al. Effect of smoking and periodontal treatment on the subgingival microflora. J Clin Periodontol. 2003;30:603–610.
- Garcia RI. Smokers have less reductions in probing depth than non-smokers following nonsurgical periodontal therapy. Evid Based Dent. 2005;6:37–38.
- Dongari-Bagtzoglou A, Research Science and Therapy Committee, American Academy of Periodontology. Drug-associated gingival enlargement. J Periodontol. 2004;75:1424–1431.
- Hernández G, Arriba L, Frías MC, et al. Conversion from cyclosporin a to tacrolimus as a nonsurgical alternative to reduce gingival enlargement: a preliminary case series. J Periodontol. 2003;74:1816–1823.
- Hall EE. Prevention and treatment considerations in patients with drug-induced gingival enlargement. Curr Opin Periodontol. 1997;4:59–63.
- Hein C, Batista EL Jr. Risk assessment for obesity and periodontal disease. Decisions in Dentistry. 2017;3(6):42–46.
- Suvan J, Petrie A, Moles DR, et al. Body mass index as a predictive factor of periodontal therapy outcomes. J Dent Res. 2014;93:49–54.
- Gorman A, Kaye EK, Apovian C, Fung TT, Nunn M, Garcia RI. Overweight and obesity predict time to periodontal disease progression in men. J Clin Periodontol. 2012;39:107–114.
- Hujoel PP, Lingström P. Nutrition, dental caries and periodontal disease: a narrative review. J Clin Periodontol. 2017;44(Suppl 18):S79–S84.
- Chapple IL, Milward MR, Dietrich T. The prevalence of inflammatory periodontitis is negatively associated with serum antioxidant concentrations. J Nutr. 2007;137:657–664.
- Levine M, Wang Y, Katz A, et al. Ideal vitamin C intake. Biofactors. 2001;15:71–74.
- Miley DD, Garcia MN, Hildebolt CF, et al. Cross-sectional study of vitamin D and calcium supplementation effects on chronic periodontitis. J Periodontol. 2009;80:1433–1439.
- Merchant AT, Pitiphat W, Franz M, Joshipura KJ. Whole-grain and fiber intakes and periodontitis risk in men. Am J Clin Nutr. 2006;83:1395–1400.
- Woelber JP, Bremer K, Vach K, et al. An oral health optimized diet can reduce gingival and periodontal inflammation in humans–a randomized controlled pilot study. BMC Oral Health. 2016;16:109.
- Al-Zahrani MS, Borawski EA, Bissada NF. Periodontitis and three health-enhancing behaviors: maintaining normal weight, engaging in recommended level of exercise, and consuming a high-quality diet. J Periodontol. 2005;76:1362–1366.
- Schätzle M, Lang NP, Ånerud A, Boysen H, Bürgin W, Löe H. The influence of margins of restoration on the periodontal tissues over 26 years. J Clin Periodontol. 2001;28:57–64.
- Matthews DC, Tabesh M. Detection of localized tooth-related factors that predispose to periodontal infections. Periodontol 2000. 2004;34:136–150.
- Zlatarić DK, Celebić A, Valentić-Peruzović M. The effect of removable partial dentures on periodontal health of abutment and non-abutment teeth. J Periodontol. 2002;73:137–144.
- Lertpimonchai A, Rattanasiri S, Arj-Ong Vallibhakara S, Attia J, Thakkinstian A. The association between oral hygiene and periodontitis: a systematic review and meta-analysis. Int Dent J. 2017;67:332–343.
- Matsui M, Chosa N, Shimoyama Y, Minami K, Kimura S, Kishi M. Effects of tongue cleaning on bacterial flora in tongue coating and dental plaque: a crossover study. BMC Oral Health. 2014;14:4.
- Outhouse TL, Al-Alawi R, Fedorowicz Z, Keenan JV. Tongue scraping for treating halitosis. Cochrane Database Syst Rev. 2006:CD005519.
- Herrera D. Chlorhexidine mouthwash reduces plaque and gingivitis. Evid Based Dent. 2013;14:17–18.
- Poklepovic T, Worthington HV, Johnson TM, et al. Interdental brushing for the prevention and control of periodontal diseases and dental caries in adults. Cochrane Database Syst Rev. 2013:CD009857.
- Barnes CM, Russell CM, Reinhardt RA, Payne JB, Lyle DM. Comparison of irrigation to floss as an adjunct to tooth brushing: effect on bleeding, gingivitis, and supragingival plaque. J Clin Dent. 2005;16:71–77.
- Apatzidou DA. Modern approaches to nonsurgical biofilm management. Front Oral Biol. 2012;15:99–116.
- Sanz M, Teughels W, Group A of European Workshop on Periodontology. Innovations in nonsurgical periodontal therapy: consensus report of the sixth european workshop on periodontology. J Clin Periodontol. 2008;35(8 Suppl):3–7.
- Smiley CJ, Tracy SL, Abt E, et al. Evidence-based clinical practice guideline on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J Am Dent Assoc. 2015;146:525–535.
- Slots J. Low-cost periodontal therapy. Periodontol 2000. 2012;60:110–137.
- Krück C, Eick S, Knöfler GU, Purschwitz RE, Jentsch HF. Clinical and microbiologic results 12 months after scaling and root planing with different irrigation solutions in patients with moderate chronic periodontitis: a pilot randomized trial. J Periodontol. 2012;83:312–320.
- Sahrmann P, Imfeld T, RonayV, Attin T, Schmidlin PR. Povidone-iodine gel and solution as adjunct to ultrasonic debridement in nonsurgical periodontitis treatment: an RCT pilot study. Quintessence Int. 2014;45:281–290.
- Greenstein G. Nonsurgical periodontal therapy in 2000: a literature review. J Am Dent Assoc. 2000; 131:1580–1592.
- Consensus report. Nonsurgical pocket therapy: mechanical, pharmacotherapeutics, and dental occlusion. Ann Periodontol. 1996;1:581–588.



