Dental Unit Waterline Safety
Poorly managed dental unit waterlines can have deadly consequences for patients. Read on for tips on how you can ensure the safety of the water in your office.

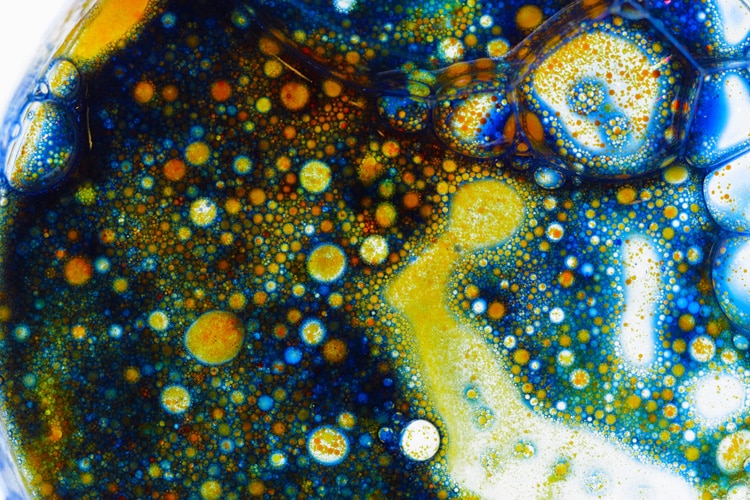
Due in part to headline-making infection control breaches involving dental treatment water, patients and the profession are placing increased scrutiny on dental waterline asepsis. The provision of safe care demands that offices follow recommended infection prevention protocols, and managing dental unit waterlines (DUWLs) is a foundational element of any successful program. Due to intermittent water flow through long, complex and narrow-bore tubing systems, DUWLs encourage, and even amplify, the formation of waterline biofilms that may contain pathogens, including Pseudomonas aeruginosa, nontuberculous mycobacteria, and Legionella species that can be released into treatment water.
Photo Credit: microgen / iStock / Getty Images Plus
Compliance Is Key
The United States Centers for Disease Control and Prevention (CDC), professional organizations, such as the Organization for Safety, Asepsis and Prevention (OSAP), and dental companies offer recommendations and resources to help offices comply with the CDC’s suggested dental water standard. For routine dental treatment, the CDC limits DUWLs to ≤ 500 colony forming units of heterotrophic (noncoliform) water bacteria per milliliter (CFU/ml). This matches the federal Environmental Protection Agency (EPA) standard for drinking water
Photo Credit: Luyali / iStock / Getty Images Plus

Management Protocol
A dental waterline management protocol should be included in every facility’s written safety program and should contain relevant laws and formal recommendations, along with specific information regarding the equipment used, procedures performed, and the germicidal products and processes employed in DUWL maintenance. Instructions for use for all equipment and products should be available and followed. The protocol must stipulate regular DUWL testing to ensure compliance with water standards. If surgical care is provided, written and physical methods for complying with the sterile irrigation standards must be available. Patient records should document sterile fluids used for surgery.
Photo Credit: Ralf Geithe / iStock / Getty Images Plus
Waterline Cleaners
Waterline cleaners and germicides fall under two main categories. Shock treatment products are used to remove established, attached DUWL biofilms. (Note: These products are caustic and clinicians should avoid contact with skin or mucosal tissues.) Low-level germicides are used to reduce planktonic biofilm and retard its attachment and growth. These agents should be continuously present within the dental water system, and are safe for patient treatment.
Photo Credit: Luyali / iStock / Getty Images Plus

Reservoir Option
Practices can also choose independent water reservoirs that isolate dental units from municipal water systems and provide immediate access to dental waterlines for intermittent- or continuously present cleaners or germicides. Manufacturers now offer equipment with separate water bottles due to the well-established criteria for water maintenance. Older units without separate reservoirs can be retrofitted with bottles to provide access for treating irrigation water. These should be filled with high-quality treatment fluid and cleaned and maintained aseptically, according to the equipment and water germicide manufacturers’ directions.
Photo Credit: amesBrey / E+
Germicide Monitoring
Automated germicide metering or slow-release devices, which may include filtration technology that can be used with independent reservoirs or municipal water connections, are another option for DUWL management. Cartridges that may filter the water—as well as release antimicrobials into DUWLs—may be located in the reservoir as an uptake “straw” or installed at other locations, such as the junction box of each dental chair or at a central location to treat multiple chairs simultaneously.
Photo Credit: Dr_Microbe / iStock / Getty Images Plus

Sterile Water
Sterile water delivery systems, which employ sterile, disposable, or heat-sterilized reusable components independent of the dental unit water supply, are indicated for surgical procedures. Peristaltic pumps, bulb syringes, other syringe types, and removable, sterilizable devices bypass the DUWL and are indicated when use of a sterile standard is appropriate.
Photo Credit: LightFieldStudios / iStock / Getty Images Plus

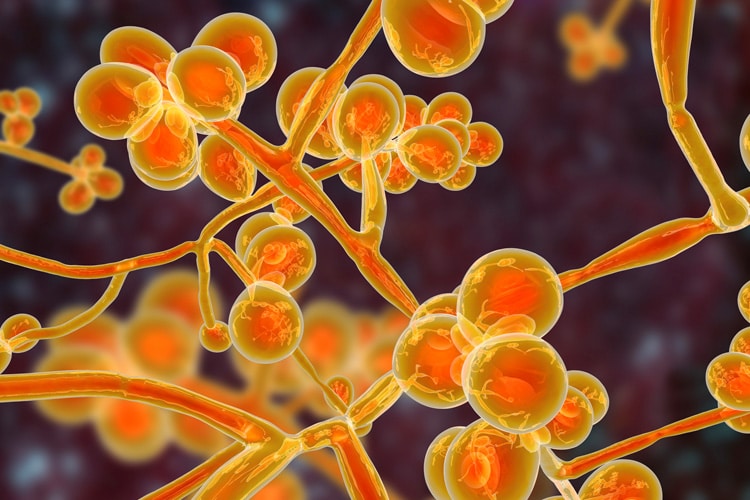
Device Alternatives
Distillers, reverse osmosis, and microfiltration devices can remove microorganisms from procedural water entering the dental unit, but do not limit the growth of biofilm after water enters the DUWL or reservoirs. These devices and processes may also produce water with high bacterial counts due to hidden and undetected biofilms. Strict protocol for preventing biofilm contamination in the devices or in stored water supplies must be followed. Studies show that samples of treated dental water may contain higher CFU/ml than tap water due to the residual levels of chlorine, more rapid water flow, and larger plumbing size of tap-water lines. Because water filters trap particulates, chemicals, and organisms, filters are potential sources of water contamination and must be regularly maintained. In addition, dental units may contain hidden or difficult-to-access filters that cultivate bacteria and fungi.
Photo Credit: RyanKing999 / iStock / Getty Images Plus

Monitoring Waterlines
Dental water systems should be regularly monitored (ie, tested) to validate management protocols or identify potential contamination. The CDC and OSAP recommend using DUWL tests as action limits that help prompt maintenance procedures, such as shocking. Monitoring methods include in-office sampling and laboratory testing. All methods of waterline testing are limited, however, as they capture only representative heterotrophic organisms used to estimate levels of noncoliform bacterial contamination. Routine testing reveals the range of CFU/ml of noncoliform organisms in water (potability), while specific tests to identify individual species are expensive and typically only done to investigate cases of suspected exposure. While in-office monitoring is simple, convenient, and costs less than laboratory testing, it provides more limited and less reliable results. In clinical practice, in-office tests may be useful as quick checks for well-managed waterlines between more reliable lab tests to provide early warning of potential contamination.

