Xerostomia Management
Patients have a variety of options when it comes to managing the symptoms of this common oral condition.
Normal salivary gland function is critical for the conservation of healthy oral mucosa. This is because saliva contains antimicrobial properties that help cleanse and lubricate the mouth.1 Xerostomia, or dry mouth, occurs when the quantity of saliva in the oral cavity diminishes by at least 50%.2 Symptoms include oral soreness,3 burning sensations, difficulty in mastication,4 trouble swallowing,5 hindered speech, and diminished taste acuity. Xerostomia can be caused by medication use, other diseases, or iatrogenic and idiopathic reasons.6
On average, the oral cavity yields approximately 500 mL of saliva every 24 hours. Unstimulated salivary flow rate is 0.3 mL/minute; sleep flow rate is 0.1 mL/minute; and flow rate increases to 4.0 mL/minute to 5.0 mL/minute during eating and chewing. Saliva, a multifaceted mix of proteins, glycoproteins, mucins, and ions, plays a significant role in oral homeostasis. This naturally occurring lubricant is vital to maintaining a healthy oral flora, and it aids in the prevention of caries; supports remineralization of early caries lesions; buffers acid produced by oral bacteria; and reduces the risk of other oral infections. Salivary mucins protect the teeth and mucosal surfaces from wear, while also possessing antifungal properties to minimize the growth of oral yeast. Antibodies found in saliva protect against cariogenic bacteria, while growth factors promote the epithelial growth required for healing.7 Saliva also aids in the neutralization of acid due to gastric reflux. Furthermore, the salivary glands’ B cells produce secretory immunoglobulin A and M.
DIAGNOSIS
The frequency of dry mouth symptoms is relevant to the diagnosis of xerostomia. For patients who experience dry mouth symptoms persistently, substantial salivary hypofunction and loss of protective saliva have occurred. A host of tests may be performed when xerostomia is suspected, including: blood work (for ESR and SS-A and SS-B antibodies); eye tests (Schirmer); urinalysis; salivary flow rate; salivary gland biopsy; and imaging (sialography, scintiscanning, ultrasound, and chest radiograph).
CAUSES
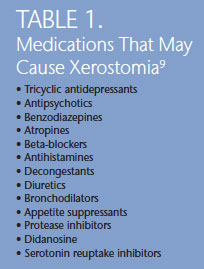 Xerostomia must be treated. Determining the root cause of this condition will help determine the course of treatment. Medication use, radiation, and other diseases are the most common causes. Dry mouth is a frequent side effect of prescription drug use. The primary cause of drug-induced xerostomia is an anticholinergic or sympathomimetic action. Medications used by those with chronic conditions also often cause dry mouth. For example, drugs used to treat the human immunodeficiency virus (HIV) are linked to xerostomia. Salivary gland disorders in patients with chronic hepatitis C have been considered oral extrahepatic manifestations. Table 1 lists the drugs most likely to cause xerostomia.8
Xerostomia must be treated. Determining the root cause of this condition will help determine the course of treatment. Medication use, radiation, and other diseases are the most common causes. Dry mouth is a frequent side effect of prescription drug use. The primary cause of drug-induced xerostomia is an anticholinergic or sympathomimetic action. Medications used by those with chronic conditions also often cause dry mouth. For example, drugs used to treat the human immunodeficiency virus (HIV) are linked to xerostomia. Salivary gland disorders in patients with chronic hepatitis C have been considered oral extrahepatic manifestations. Table 1 lists the drugs most likely to cause xerostomia.8
Salivary glands are highly susceptible to radiation injury—specifically the parotid glands. Even a single dose of radiation measuring less than 20 Gy may result in permanent termination of salivary flow. While doses of 60 Gy to 70 Gy are common in the treatment of oral carcinoma, doses as low as 52 Gy can cause severe salivary dysfunction. After radiation treatment, a 95% decrease in salivary flow may result. Fortunately, the unaffected salivary gland tissue often hypertrophies several months after treatment, providing relief and reduction in the perception of oral dryness. Partially radiated glands may have a greater flow rate compared to irradiated glands.9 Radiation to a salivary gland tumor may possibly circumvent the contralateral gland, thus xerostomia may not be as severe. Data reveal, however, that radiation to the nasopharynx results in damage to both parotid glands—thus, lifelong xerostomia. In some instances of oral cancer radiation, treatments can be positioned wholly or partially around the parotid gland to reduce the severity of resultant xerostomia.10,11 New techniques, such as cone radiation, mitigate the damage by ensuring the treatment affects only one gland.12
Viral and bacterial infections may also hinder salivary gland function, with sialadenitis and obstruction most often reported.13 Sjögren’s syndrome, an autoimmune disease involving the salivary and lacrimal glands,14 is another cause of dry mouth—with many studies implicating type 1 IFN-alpha and lymphotoxin-alpha as main factors in this disease. Increased levels of IFN-alpha prompt myeloid dendritic cells and T helper cells, which contribute to increased autoantibody and cytotoxic T cell production, to damage salivary gland cells. Recent evidence demonstrates that the severity of secretory dysfunction is not necessarily related to the amount of lymphocytic infiltration and glandular destruction.15
Age in itself is not a risk factor for dry mouth, but older adults are more likely to develop xerostomia due to their increased use of medications, which often have synergistic effects. For 50% of older Americans, routine drug use is commonplace. The higher the number of prescriptions used, the greater the likelihood of decreased salivary flow.16,17 Furthermore, evidence suggests that older adults’ salivary glands are more susceptible to medication with anticholinergic effects.18
TREATMENT
Treatment methods to relieve xerostomia symptoms can be divided into four categories: prevention, symptomatic relief, local, or topical salivary stimulant. Prevention is important to mitigate the effects of decreased salivary function and to reduce its occurrence. For example, patients undergoing radiation treatment may benefit from stents to protect the glands during unilateral treatment. Another option is intensity-modulated irradiation, which targets only the lesion and frees major salivary glands from radiation.19 The use of amifostine, an oxygen scavenger, may provide protection for the salivary glands during radiation treatment. Amifostine use, however, requires intravenous administration and exerts negative side effects.20 Modification of medication use, altering the time of day medication is taken, and dividing single doses into two are also useful techniques in mitigating the effects of medication-induced xerostomia.
Symptomatic relief can be as simple as drinking water during the day. Caffeine, alcohol, and sugar-containing products should be avoided, as they can dry the mouth and increase caries susceptibility. Artificial saliva products and oral lubricants can improve patient comfort, but they do not reduce the risk of caries or other oral infections.21 Toothpastes, mouthrinses, and gels with a neutral pH also offer relief, while fluoride and calcium lactate aid in caries and calculus prevention. Aloe vera may help prevent mucositis following radiation therapy.22
Calcium phosphate technologies—including amorphous calcium phosphate (ACP), casein phosphopeptide-ACP (Recaldent®), calcium sodium phosphosilicate (NovaMin®), and tricalcium phosphate—are designed to boost remineralization by supplying the oral cavity with additional calcium and phosphate ions. For individuals with reduced salivary flow, these technologies may help reduce caries risk. The addition of the lubricant carboxymethylcellulose to mouthrinse and chewing gum can help relieve dry mouth symptoms.23 The use of fluoride and cetylpyridinium chloride mitigate caries and inhibit plaque formation and gingivitis.24
Secretagogues, such as pilocarpine and cevimeline, work by stimulating functional salivary gland tissue, increasing saliva flow. If no viable salivary gland tissue exists, however, improvement in symptoms cannot occur. Pilocarpine is a parasympathetic agent that acts as a general muscarinic agonist with beta-adrenergic activity. Side effects of its use include: gastrointestinal upset; sweating; tachycardia; bradycardia; increased pulmonary secretion; increased smooth muscle tone; and blurred vision. Cevimeline is a cholinergic agonist that acts on muscanaric receptors, which are the primary mediators of salivation.
Other methods of salivary stimulation include chewing xylitol gum, electrostimulation, and acupuncture. The long-term use of xylitol has been shown to reduce Streptococcus mutans levels and decrease caries risk.25 Acupuncture increases salivary flow when a weekly regimen of three treatments to four treatments is followed.26 A variety of dietary supplements may increase rates of unstimulated saliva.27 Bioengineering is another possibility, as Japanese scientists recently regenerated glands through orthotropic transplanted organ germs. The organ germs were able to mature into parotid, submandibular, and sublingual glands in gland-defective mice.28
CONCLUSION
Saliva flow is necessary for maintaining oral health. It protects both the hard and soft tissues through lubrication and the creation of the salivary pellicle, which shields against chemical and bacterial irritants. Xerostomia can result from a variety of factors and exerts negative effects on the oral cavity. Prevention and successful treatment depend on determining the root cause of the condition. Further research into potential protective and preventive treatment methods is advised.
REFERENCES
- Wolff A, Fox PC, Ship JA, Atkinson JC, Macynski AA, Baum BJ. Oral mucosal status and major salivary gland function. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1990;70:49–54.
- Dawes C. Physiological factors affecting salivary flow rate, oral sugar clearance and the sensation of dry mouth in man. J Den Res. 1987;66:648–653.
- Navazesh M, Christensen C, Brightman V. Clinical criteria for the diagnosis of salivary gland hypofunction. J Dent Res. 1992;71:1363–1369.
- Gerdin EW, Einarson S, Jonsson M, Aronsson K, Johansson I. Impact of dry mouth conditions on oral health-related quality of life in older people. Gerodontol. 2005;22;219–226.
- Rhodus NL, Moller K, Colby S, Bereuter J. Articulatory speech performance in patients with salivary gland dysfunction: a pilot study, Quintessence Int. 1995;26:805–812.
- Liu B, Dion MR, Jurasic MM, Gibson G, Jones JA. Xerostomia and salivary hypofunction in vulnerable elders: prevalence and etiology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:52–60.
- Atkinson JC, Grisius M, Massey W. Salivary hypofunction and xerostomia: diagnosis and treatment. Dent Clin North Am. 2005;49:309–326.
- Croog SH, Elias MF, Colton T, et al. Effects of antihypertensive medication on quality of life in elderly hypertensive woman. Am J Hypertens. 1994;7:329–339.
- Epstein JB, van der Meij EH, Lunn R, Stevenson-Moore P. Effects of compliance with fluoride gel application on caries and caries risk in patients after radiation therapy for head and neck cancer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:268–275.
- Scully C, Bagan JV, Hopper C, Epstein JB. Oral cancer: current and future diagnostic techniques. Am J Dent. 2008;21:199–209.
- Scully C, Epstein JB. Oral health care for the cancer patient. Eur J Cancer B Oral Oncol. 1996;32B:281–292.
- Singh N, Scully C, Joyston-Bechal S. Oral complications of cancer therapies: prevention and management. Clin Oncol (R Coll Radiol). 1996;8:15–24.
- Chuangqi Y, Chi Y, Lingyan Z. Sialendoscopic findings in patients with obstructive sialadenitis: long-term experience. Br J Oral Maxillofac Surg. 2013;51:337–341.
- Fox RI, Howell FV, Bone RC, Michelson P. Primary Sjögren’s syndrome: clinical and immunopathologic features. Semin Arthritis Rheum. 1984;14:77–105.
- Dawson IJ, Fox PC, Smith Sjögren’s syndrome-the non-apoptotic model of glandular hypofunction. Rheumatology (Oxford). 2006;45;792–798.
- Navazesh M, Brightman VJ, Pogoda JM. Relationship of medical status, medications, and salivary flow rates in adults of different ages. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:172–176.
- Wu AJ, Ship JA. A characterization of major salivary gland flow rates in the presence of medications and systemic diseases. Oral Surg Oral Med Oral Pathol. 1993;76:301–306.
- Ghezzi EM, Ship JA. Aging and secretory reserve capacity of major salivary glands. J Dent Res. 2003;82:844–848.
- Eisbruch A, Ship JA, Dawson LA, et al. Salivary gland sparing and improved target irradiation by conformal and intensity modulated irradiation of head and neck cancer. World J Surg. 2003;27:832–837.
- Rades D, Fehlauer F, Bajrovic A, Mahlmann B, Richter E, Alberti W. Serious adverse effects of amifostine during radiotherapy in head and neck cancer patients. Radiother Oncol. 2004 Mar;70(3):261-264.
- Alves MB, Motta AC, Messina WC, Migliari DA. Saliva substitute in xerostomic patients with primary Sjögren’s syndrome: a single-blind trial. Quintessence Int. 2004;35:392–396.
- Ahmadi A. Potential prevention: Aloe vera mouthwash may reduce radiation-induced oral mucositis in head and neck cancer patients.Chin J Integr Med. 2012;18:635–640.
- Oh DJ, Lee JY, Kim YK, Kho HS. Effects of carboxymethylcellulose (CMC)-based artificial saliva in patients with xerostomia. Int J Oral Maxillofac Surg. 2008;37:1027–131.
- Sreenivasan PK1, Haraszthy VI, Zambon JJ. Antimicrobial efficacy of 0·05% cetylpyridinium chloride mouthrinses. Lett Appl Microbiol. 2013;56:14–20.
- Ly KA, Milgrom P, Rothen M. The potential of dental-protective chewing gum in oral health interventions. J Am Dent Assoc. 2008;139:553–563.
- Johnstone PA, Niemtzow RC, Riffenburgh RH. Acupuncture for xerostomia: clinical update. Cancer. 200215;94:1151–1156.
- Pedersen A, Gerner N, Palmvang I, Høier-Madsen M. LongoVital in the treatment of Sjögren’s syndrome. Clin Exp Rheumatol. 1999;17:533–538.
- Ogawa M, Oshima M, Imamura A, et al. Functional salivary gland regeneration by transplantation of a bioengineered organ germ. Nat Commun. 2013;4:2498.
From Dimensions of Dental Hygiene. March 2014;12(3):34,36;39.

