 MEGAFLOPP/ISTOCK/GETTY IMAGES PLUS
MEGAFLOPP/ISTOCK/GETTY IMAGES PLUS
An Update on Cardiovascular Disease
Educating patients on their risk for heart disease and strategies for prevention can help them maintain both their oral and overall health.
This course was published in the May 2021 issue and expires May 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the prevalence of cardiovascular disease in the United States.
- Discuss current issues, determinants, and trends related to heart disease.
- Note considerations for treating patients with heart disease in the dental setting.
In the United States, cardiovascular disease (CVD) is the leading cause of death among men and women and in most racial and ethnic groups.1,2 CVD refers to several types of heart conditions; the most common is coronary heart disease, also known as coronary artery disease or ischemic heart disease, which can cause acute myocardial infarction. Other heart conditions that may lead to heart failure include a past history of myocardial infarction, abnormal heart valves, heart muscle disease, or congenital heart muscle disease. In adults ages 65 and younger, approximately two in 10 deaths are caused by coronary artery disease, and about 18.2 million adults (6.7%) age 20 and older have the disease.3,4 CVD, along with stroke, are among the most preventable noncommunicable diseases.2
Peaking in the US in the mid-20th century, CVD-related deaths were associated with smoking and high cholesterol levels. By the mid-1960s, CVD-related deaths declined due to advances in treatment and preventive measures. By the late 20th century, deaths further decreased because of declining smoking rates and widespread use of cholesterol-lowering medications.5,6 Despite these advances, the CVD mortality rate has plateaued in recent years, and is beginning an upward trend due to the increasing prevalence of obesity and type 2 diabetes mellitus in younger people.7 Individuals with underlying medical conditions, such as CVD, are also at high risk of severe COVID-19 illness.8
Social Determinants of Health for Heart Disease
Social determinants of health for heart disease are the conditions in which people live, work, and play that impact quality of life and health outcomes.9 Imbalances in social determinants of health can exert negative effects on the health of individuals and communities. When considering factors that influence health, socioeconomic status is a strong predictor of a person’s morbidity and mortality.10 Socioeconomic status is a set of interrelated variables that influence health outcomes, such as education, race/ethnicity, and occupation. Following is a discussion of the most impactful socioeconomic factors on health.
Education
Education provides the most consistent results in relation to CVD outcomes. The Prospective Urban Rural Exchange—a large-scale prospective cohort study conducted from 2001 to 2014 among individuals aged 35 to 70 from high, middle, and low income countries—found that education rather than wealth was the most consistent risk indicator of CVD.11 A plausible hypothesis for this phenomenon is that education may protect against influencing factors, such as lifestyle behaviors, problem-solving abilities, and values. Higher education levels may lead to more positive psychological and economic skills, and provide insulation from adverse influences.10
![TABLE 1. Ways in Which Implicit Bias Can Be Expressed by Healthcare Providers]() Employment/Occupational Status
Employment/Occupational Status
Employment status is a more challenging predictor of CVD risk than education. Research shows that higher status occupations are associated with a lower risk of hypertension.12 However, a lack of data exists on the relationship between occupation and cardiovascular morbidity and mortality in the US. Studies do suggest a relationship between unemployment and CVD exists. Epidemiological studies are difficult because of the potential “effect-cause” relationship (ie, is an individual unemployed because of poor health, or is unemployment a contributing factor to poor health outcomes?).12 Research does show that, after adjusting for risk factors and sociodemographics, the hazard for myocardial infarction was highest during the first year of unemployment and subsequently increased with the number of jobs lost.12 Currently unemployment rates are higher due to the COVID-19 pandemic, possibly increasing the risk of myocardial infarction.
Early Life
A systematic review of 40 studies showed a strong association between poor childhood socioeconomic circumstances and CVD.13 Studies focused on childhood socioeconomic conditions in relation to their parents’ education and occupational status found consistent evidence of CVD risk factors, such as blood pressure, lipid levels, body mass index, smoking, physical activity, and alcohol consumption.
Race, Ethnicity, and Implicit Bias
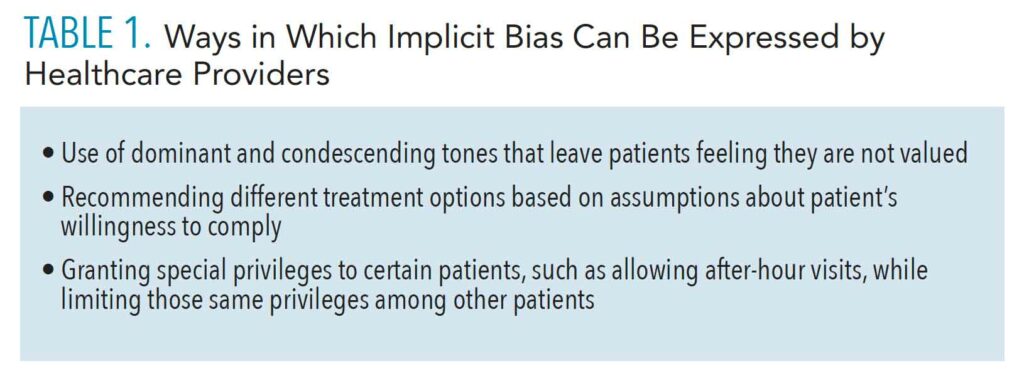
According to the American Heart Association, Black people are two times to three times more likely to die from heart disease than whites.12 Black populations and residents of the Southeastern US are also at the greatest risk for stroke.14 There is concern of implicit bias among healthcare providers that may influence medical treatment. Implicit attitudes are thoughts and feeling that exist outside of conscious awareness, and thus are difficult to consciously acknowledge and control.15 Table 1 lists ways in which implicit bias can be expressed by healthcare professionals.
A systematic review of the literature showed low levels of implicit bias among healthcare providers based on race/ethnicity against Black, Hispanic/Latino, and dark-skinned individuals.15 In addition to race and ethnicity, implicit bias can also be based on gender, socioeconomic status, age, weight, disability, mental illness, acquired immunodeficiency syndrome status, social circumstances, drug use, and brain injury.16 This is emerging research, and more is needed to understand the role of implicit bias in healthcare and how to provide interventions for healthcare providers.
Access to Care
The issue of access to care is complex and multifactorial. Research indicates that Black and Hispanic stroke survivors may have reduced access to preventive care because of lower median household income, lack of access to high-quality care, and lack of insurance.12 Lack of insurance is associated with a lower potential of adequate treatment of risk factors and an increased risk of stroke and cardiovascular death. Data show that only about half of the US population has timely access to a primary stroke center, and there is an uneven distribution of cardiologists in the country, with little access in rural areas.
The type of insurance a patient has is also a factor. Patients covered by Medicaid are twice as likely to encounter barriers to primary care, compared to those with private insurance. Low reimbursement rates make finding a physician difficult, as well as physician prejudices about patients covered by Medicaid, believing they are less likely to keep appointments and adhere to treatments.12
![]() Current Issues
Current Issues
Obesity is a major risk factor for CVD, type 2 diabetes, hypertension, stroke, and coronary artery disease. Hypertension is a risk factor for stroke, myocardial infarction, heart failure, and arterial aneurysm. From 1999 to 2018, the US experienced an increase in the prevalence of obesity in adults, with an estimated 70% of US adults classified as overweight or obese. The number of Americans with severe obesity almost doubled in the same timeframe.17,18 Those at greatest risk are non-Hispanic Black individuals, followed by Hispanic individuals, non-Hispanic whites, and non-Hispanic Asians.18 If rates keep rising, by 2030, approximately 86.3% of US adults will be overweight or obese.19,20
Childhood obesity increases the likelihood of experiencing obesity in adulthood. Furthermore, children are exhibiting earlier onset of hypertension and high cholesterol.20 Triglyceride levels have also risen with the increase of obesity, insulin resistance, and type 2 diabetes. Triglycerides are a type of fat found in the blood. It is unclear what impact triglyceride levels have on CVD.21,22 High triglycerides, in combination with high blood glucose and hypertension, can lead to CVD, stroke, as well as blindness, kidney failure, amputations of leg and feet, and even early death.22 In the US, 31% of the population has high levels of triglycerides, with the highest rates exhibited by Mexican Americans.
About 34 million Americans have diabetes, of those, 90% to 95% are diagnosed with type 2 diabetes.23 Type 2 diabetes is caused by an increase of sugar in the bloodstream. The increased production of insulin by the pancreas can make cells insulin resistant. However, the pancreas keeps producing in order to get the cells to respond. Eventually, the pancreas cannot keep up and blood sugar keeps rising.23,24 Diabetes is a risk factor for CVD in adults older than 45. Diabetes is also increasing in children, teens, and young adults.
CVD is the leading cause of morbidity and mortality (68%) among US individuals with type 2 diabetes. Native Americans and Alaska natives have the highest rate of diagnosed diabetes, followed by Hispanic and non-Hispanic Black populations.24 About 7.3 million Americans have undiagnosed diabetes.25
Prevention
There are many ways to inform and educate patients to help reduce and prevent CVD. Encouraging patients to keep their blood pressure, cholesterol, and blood sugar levels at healthy ranges can help lower their risk for CVD. If medication is taken to treat any of these issues, remind patients to follow the instructions and to avoid ceasing any medication regimen without first consulting their primary medical provider. Also, discussing tobacco cessation and referring patients to quitting resources will help reduce CVD risk. Oral health professionals can discuss choosing healthy foods and snacks and avoiding foods high in saturated and trans fats. Point out the importance of maintaining a healthy weight by exercising daily.
Implications for the Dental Appointment
Oral health professionals can play an important role in educating patients on the influence of oral health on systemic health. Some individuals with CVD are at a small risk of developing infective endocarditis.26,27 This group includes children, young adults, and adults with heart defects, adults with previous valve surgeries or heart transplant, calcium deposits in the mitral or aortic valves, and those with a history of endocarditis. Infective endocarditis can occur from self-induced bacteremia caused by eating, chewing gum, bruxism, or any activity that forces bacteria through the wall of a diseased sulcus or pocket. Periodontal therapy and scaling that induce bleeding can also create bacteremia.26
Hypertension, or the “silent killer,” is responsible for more deaths from CVD than any other risk factor. Oral health professionals can support their patients’s health by taking a complete medical history and medication review prior to each appointment, providing blood pressure screenings at all appointments, and offering medical referrals for patients who are prehypertensive or hypertensive.
Patients who take anticoagulants—such as heparin and warfarin; those who take direct oral anticoagulants, such as dabigatran, rivaroxaban, apixaban, and edoxaban; and patients on antiplatelet therapy medications, such as aspirin, clopidogrel, ticlopidine, and ticagrelor—need special care. Oral health professionals should always take a complete medical history and medication review at each appointment. A consultation with the patient’s cardiologist or primary care physician to determine bleeding risk may be prudent. Clinicians should also ask for the patient’s most recent international normalized ratio, or INR, which evaluates the status of coagulation. Patients should be advised to continue on their anticoagulant therapy prior to the dental visit and to perform meticulous oral self-care in order to remove as much biofilm as possible prior to treatment to minimize bleeding. If anesthesia is needed, a local drug with a vasoconstrictor should be administered to minimize bleeding; the administration of nerve blocks should be avoided if possible to prevent hemorrhage. Oral health professionals should also take care to minimize tissue trauma and apply pressure to control bleeding. The patient should remain in the dental office under observation until all bleeding stops.26
After dental treatment is complete, oral health professionals should follow up with the patient to check on overall health status. Patients should be advised to avoid rinsing for 24 hours, avoid vigorous brushing for several hours or until the next day, and avoid hot and hard foods until the next day. Patients should leave the practice with extra gauze and an emergency contact at the practice if there is excessive bleeding.26
Conclusion
The true value of the dental hygienist goes beyond teaching patients good oral hygiene. Dental hygienists can help patients improve their oral and systemic health by helping them understand the relationship between oral health and overall health. Oral health professionals can emphasize the importance of routine medical exams, as well as educate patients on drug interactions and their effect on the oral cavity. Developing interprofessional collaborations with medical professionals also provides an opportunity to educate about the effects of systemic disease on oral health. Oral health professionals should be familiar with current trends and issues associated with CVD and share this information with patients to emphasize the importance of optimal oral hygiene as a factor in maintaining good overall health.
References
- United States Centers for Disease Control and Prevention. Underlying cause of death, 1999–2018. Available at: wonder.cdc.gov/wonder/help/ucd.html#. Accessed April 23, 2021.
- Murphy SL, Kochanek KD, Xu JQ, Arias E. Mortality in the United States, 2014. Available at: cdc.gov/nchs/data/databriefs/ db229.pdf. Accessed April 23, 2021.
- Benjamin EJ, Munter P, Alonso A, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528.
- Fryar CD, Chen TC, Li X. Prevalence of uncontrolled risk factors for cardiovascular disease: United States, 1999–2010. NCHS Data Brief. 2012;103:1–8.
- Dalen JE, Alpert JS, Goldberg RJ, Weinstein RS. The epidemic of the 20th century: coronary heart disease. Am J Med. 2014;127:807–812.
- Jones DS, Greene JA. The decline and rise of coronary heart disease: understanding public health catastrophism. Am J Public Health. 2013;103:1207–1218.
- Pallazola VA, Davis DM, Whelton SP, et al. A clinician’s guide to healthy eating for cardiovascular disease prevention. Mayo Clin Proc Innov Qual Outcomes. 2019;3:251–267.
- Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. 2020;324:510–513.
- US Centers for Disease Control and Prevention. Social determinants of health. Available at: cdc.gov/socialdeterminants/ index.htm. Accessed April 23, 2021.
- Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health.1992;82:816–20.
- Rosengren A, Smyth A, Rangarajan S, et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob Health. 2019;7:e748–e760.
- Havranek EP, Mujahid MS, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–898.
- Harper S, Lynch J, Smith GD. Social determinants and the decline of cardiovascular diseases: understanding the links. Annu Rev Public Health. 2011;32:39–69.
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–492.
- Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105:e60–76.
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18:19.
- Akil L, Ahmad HA. Relationships between obesity and cardiovascular diseases in four southern states and Colorado. J Health Care Poor Underserved. 2011;22(4 Suppl):61–72.
- US Centers for Disease Control and Prevention. Overweight and Obesity. Available at: cdc.gov/obesity/data/adult.html. Accessed April 23, 2021.
- Bhupathiraju SN, Hu FB. Epidemiology of obesity and diabetes and their cardiovascular complications. Circ Res. 2016;118:1723–1735.
- US Centers for Disease Control and Prevention. Prevalence of Childhood Obesity in the United States. Available at: cdc.gov/obesity/data/childhood.html. Accessed April 23, 2021.
- US Centers for Disease Control and Prevention. Diabetes Report Card 2019. Available at: cdc.gov/diabetes/pdfs/library/Diabetes-Report-Card-2019-508.pdf. Accessed April 23, 2021.
- Miller M, Stone NJ, Ballantyne C, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292–2233.
- US Centers for Disease Control and Prevention. Type 2 Diabetes. Available at: cdc.gov/diabetes/basics/type2.html. Accessed April 23, 2021.
- US Centers for Disease Control and Prevention. Insulin Resistance and Diabetes. Available at: cdc.gov/diabetes/ basics/insulinresistance.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fdiabetes%2Flibrary%2Fspotlights%2Fdiabetes-insulin-resistance.html. Accessed April 23, 2021.
- Stewart R, West M. Increasing evidence for an association between periodontitis and cardiovascular disease. Circulation. 2016;133:549–551.
- Smallidge D, Boyd L. The patient with cardiovascular disease. In: Boyd L, Mallonee LF, Wyche CJ, eds. Wilkins’ Clinical Practice of the Dental Hygienist. 13th ed. Burlington, Massachusetts: Jones and Bartlett; 2020:1043–1060.
- American Heart Association. Heart Valves and Infective Endocarditis. Available at: heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/heart-valves-and-infective-endocarditis. Accessed April 23, 2021.
From Dimensions of Dental Hygiene. May 2021;19(5):40-43


 Employment/Occupational Status
Employment/Occupational Status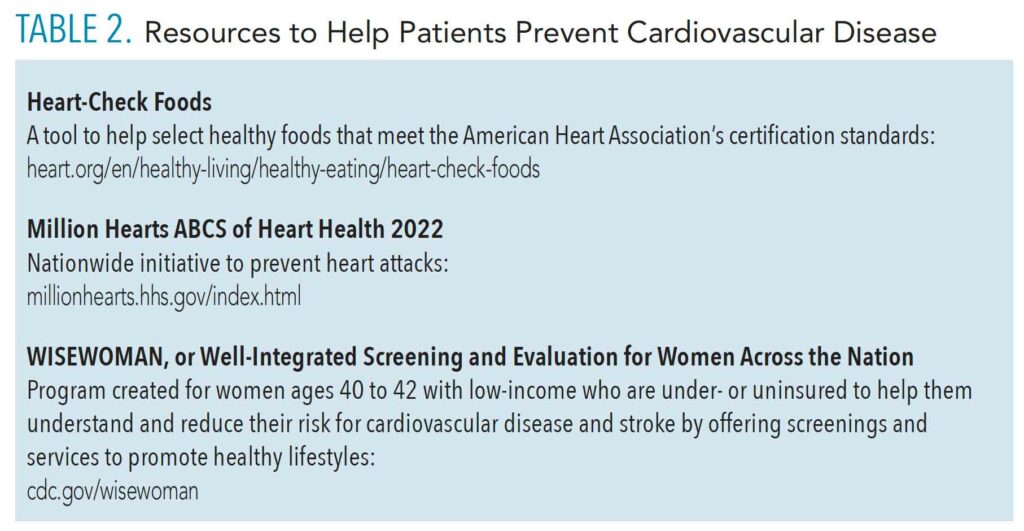 Current Issues
Current Issues
