 MICROSCAPE / SCIENCE SOURCE
MICROSCAPE / SCIENCE SOURCE
Understanding Cerebral Palsy
Children with this neurological disorder experience a variety of signs and symptoms, some of which impact the delivery of dental care.
This course was published in the December 2015 issue and expires December 21, 2018 2021. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the clinical and public health significance of the prevention of cerebral palsy (CP).
- Define the risk factors for CP.
- Describe the common impairments and complications caused by CP.
- Identify oral health care considerations for patients with CP.
Individuals with CP experience abnormalities in the part of the brain that controls muscle movement.3 Medical complications associated with CP include spasticity, joint contractures, hip dislocations, spinal disorders, osteoporosis, intellectual disability, seizures, gastroesophageal reflux, dysphagia, failure to thrive, and hearing loss.4 CP causes motor disorders accompanied by disturbances of sensation, cognition, communication, perception, and behavior, in addition to seizures.5
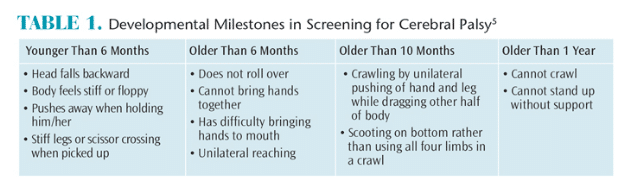
CP’s etiology is unclear, but genetic mutations may play roles.6 There is no known cure nor is there a single definitive test to diagnose CP. Instead, a detailed differential diagnostic process is used to rule out other maladies. Early detection and diagnosis are recommended for all children who exhibit known risk factors for CP. Early screening tests, such as developmental monitoring or surveillance for intellectual, motor, or movement delays, and medical evaluations by a pediatrician are recommended.7 The early signs of CP are detectable before age 3 (Table 1).3,5
CLINICAL AND PUBLIC HEALTH SIGNIFICANCE
Approximately 500,000 children have been diagnosed with CP in the US.2 About two children to three children are affected out of every 1,000 live births.2 Each year approximately 10,000 babies in the US are diagnosed with CP.2 The US Centers for Disease Control and Prevention monitors the prevalence of CP and other health conditions via the Autism and Developmental Disabilities Monitoring Network (ADDM). The ADDM estimates about one in 323 US children have CP.7 Boys are approximately 1.5 times more likely than girls to be diagnosed with CP.8 Evidence suggests that non-Hispanic blacks are more likely than non-Hispanic whites to be diagnosed with CP and that non-Hispanic whites are just as likely as Hispanics to be diagnosed with CP.2
The expense of caring for those with CP is high. The estimated cost of caring for all Americans who are affected by CP over a lifetime is $11.5 billion.7 For an individual, the expense of care provided over a lifetime is about $1 million.7 More than 80% of total expenditures are indirect costs, such as loss of productivity, whereas 10% are related to direct medical costs. The remaining 10% of costs go toward special educational services.9 In 2005, expenditures for Medicaid-enrolled children with CP were 10 times higher than for children without CP or other intellectual disabilities.7 For Medicaid-enrolled children with both CP and an intellectual disability, costs were 26 times higher than for children without CP or an intellectual disability.7
The most common risk factors for CP are premature birth, low birth weight, untreated neonatal jaundice, and birthing complications such as insufficient oxygen supply or injury. The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists conclude that the majority of CP cases are not caused by adverse complications experienced during labor and delivery.10 Thyroid dysfunction, intellectual disability, history of epilepsy, excessive mercury consumption, blood incompatibility, and incomplete immunization history in pregnant women are also related to CP risk.6 Specifically, infections during pregnancy—such as varicella, rubella, and cytomegalovirus—are established risk factors for poor pregnancy outcomes.7 While most cases of CP are congenital, approximately 10% are acquired via exposure to trauma such as an infection like meningitis or a closed head injury.7 Expectant mothers need to be advised on these risk factors so they can minimize the risk of CP.
CATEGORIZATION OF CEREBRAL PALSY![Cerebral Palsy Common Impairments]()
There are two types of CP: spastic and nonspastic. The spastic form is the most common, affecting approximately 80% of the diagnosed population.7 Patients with spastic CP have increased muscle tone, which causes stiffness and awkward movements.7 Approximately 20% to 30% of those with spastic CP have hemiplegia, or weakness on either the right side or left side of the body. Arms are affected more often than legs. Between 30% and 40% of individuals with spastic CP have diplegia, or paralysis of corresponding parts on both sides of the body in which the legs are more commonly affected than the arms. Patients with CP and diplegia often walk in a scissor-like manner, with the legs turning inward. Quadriplegia, or complete or partial loss of limb movement, affects approximately 10% to 15% of patients with spastic CP. It is the most severe form of spastic CP and often leaves the affected individual immobile. Dyskinetic and ataxic CP (nonspastic types) affect approximate 20% of the diagnosed population. Individuals with dyskinetic CP experience uncontrollable limb movement, varying levels of muscle tone, and chronic dysphagia. Ataxic CP causes problems with balance, steadiness, control, and coordination.4 Table 2 lists the most common signs and symptoms of CP.
NEUROLOGICAL IMPAIRMENT
The four most common comorbidities associated with CP are: neurological impairment, musculoskeletal impairment, gastroesophageal reflux, and failure to thrive.11 Approximately 41% of patients with CP experience seizures and undergo treatment to manage epilepsy.2 Furthermore, about 30% to 50% of people with CP experience some form of intellectual disability.2 The highest rate of intellectual disability is found in those with the spastic quadriplegic form of CP.2 Unfortunately, the neurological impairments often result in spasticity and a loss of gross and/or fine motor skills.11 Seizures are categorized as either partial/focal or generalized, depending on where the seizure activity originates in the neurological tissues. Partial seizures are additionally classified as either simple or complex. Assessing the patient’s level of consciousness is important in determining which type of seizure he or she has. For example, patients with partial simple seizures typically do not lose consciousness. On the other hand, patients with partial complex seizures typically experience partial or complete consciousness impairment. Common signs and symptoms of a simple partial seizure include tingling of the contralateral side of the body, ringing in the ears, and sweating.2 Partial complex seizure signs and symptoms usually present as auditory and visual hallucinations, psychomotor masticatory movements, and dysphagia.2 Finally, patients with generalized seizures typically lose consciousness entirely. Generalized seizures are additionally classified as absence, myoclonic, tonic-clonic, tonic, and atonic.7
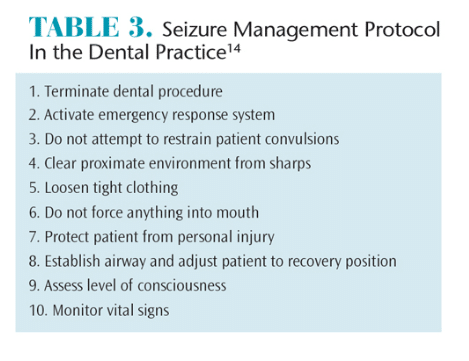 Individuals with seizure disorders are at increased risk of traumatic injuries. Uncontrollable biting reflexes during an epileptic episode can cause fractured hard dentition and/or self-induced lacerations on the tongue.4 Anticonvulsant medications, such as dilantin and phenytoin, are often prescribed to patients who experience seizures, and these significantly increase the risk of gingival hyperplasia and other oral health problems.12 Several studies noted an increase in the prevalence of bruxism among populations with intellectual disability—a common comorbidity associated with CP—compared to those without intellectual disability.4 In the dental setting, anxiety or bright light/movement can trigger seizures in patients with CP. Oral health professionals need to be prepared to handle an epileptic episode by stabilizing care until the arrival of an emergency medical response team (Table 3).13
Individuals with seizure disorders are at increased risk of traumatic injuries. Uncontrollable biting reflexes during an epileptic episode can cause fractured hard dentition and/or self-induced lacerations on the tongue.4 Anticonvulsant medications, such as dilantin and phenytoin, are often prescribed to patients who experience seizures, and these significantly increase the risk of gingival hyperplasia and other oral health problems.12 Several studies noted an increase in the prevalence of bruxism among populations with intellectual disability—a common comorbidity associated with CP—compared to those without intellectual disability.4 In the dental setting, anxiety or bright light/movement can trigger seizures in patients with CP. Oral health professionals need to be prepared to handle an epileptic episode by stabilizing care until the arrival of an emergency medical response team (Table 3).13
MUSCULOSKELETAL IMPAIRMENT
Secondary musculoskeletal impairments associated with CP include spinal disorders such as scoliosis and kyphosis, joint contractures, osteoporosis, and hip dislocations.4 Populations with musculoskeletal impairments typically require long-term rehabilitation through physical and occupational therapy. Surgical interventions, such as spinal instrumentation, are required to treat moderate to severe forms of scoliosis and/or kyphosis.4 More than 50% of dental patients with musculoskeletal impairments manifest with a Class II malocclusion and an anterior open bite due to hypotonia of the facial musculature.4
Clinicians need to be aware that patients with CP are at increased risk of dysphagia, which is associated with poor swallowing reflex, and chronic inflammation of the soft tissues due to mouth breathing.4 Patients who have undergone spinal surgical intervention are particularly susceptible to secondary infections after the completion of invasive dental treatment. Oral health professionals need to consult with the patient’s surgeon(s) to obtain medical clearance, determine the need for prophylactic antibiotic premedication, and assess whether elective preventive or restorative dental treatment should be deferred.11
GASTROINTESTINAL REFLUX AND FAILURE TO THRIVE
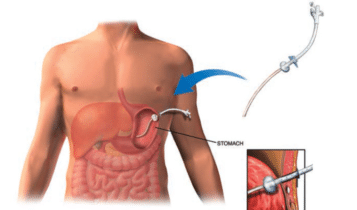
Supporting healthy growth and development and delivering proper nutrition are challenging in patients with CP.15 Chronic gastrointestinal concerns are common among this population.4 Recurrent emesis, or vomiting, and malnutrition are significant problems for people with chronic gastroesophageal reflux.2 An estimated one-third of children with CP are undernourished.2 The most frequently cited reasons for feeding difficulties include poor posture control, uncoordinated movements of upper limbs, lack of independent mobility, and impairments in vision and hearing.2 If left untreated, the chronic irritation of regurgitated gastric acid can erode the mucosal lining of the esophagus (erosive esophagitis) and potentially aspirate into the bronchial tissues.4 Medical interventions to manage moderate to severe gastroesophageal reflux disease and malnourishment include the surgical placement of a gastrostomy and Nissen fundoplication. A gastrostomy is a surgical procedure in which a feeding tube is inserted, so the patient is able to receive adequate nourishment (Figure 1).11 The Nissen fundoplication is a surgical procedure that prevents the resurgence of gastric acid into the esophageal tissue.2
JOHN T. ALESI / SCIENCE SOURCE
Individuals with chronic gastric acid reflux are at increased risk of oral health problems such as enamel erosion and Barrett’s esophagus. Dental enamel—the hardest tissue in the body—undergoes permanent and irreversible erosion from regurgitated gastric acid and leaves oral tissues susceptible to disease. Many patients with chronic acid reflux develop dentinal hypersensitivity due to exposure of the enamel.4
Barrett’s esophagus is irreversible damage to the lining of the esophagus caused by regurgitation of gastric acid. Patients exposed to chronic gastric acid reflux are at an increased risk for esophageal and pharyngeal cancer due to metaplasia of the soft tissues. These patients require close monitoring and should be immediately referred if a suspicious lesion arises.2
Individuals with a feeding tube are at increased risk of periodontal diseases and poor swallowing reflex.4 These patients typically experience oral aversion, do not eat by mouth, and have difficulty maintaining an oral hygiene regimen. Preventive dental visits are critical for patients with feeding tubes because of their increased accumulation of bacteria, which forms heavy layers of biofilm and calculus. Patients with feeding tubes are also at increased risk of aspiration, so debridement should be provided with the minimum amount of water and prophylaxis paste. The saliva ejector should be used judiciously and the dental chair should be positioned in a more upright position to minimize the risk of dysphagia. The assistance of extra personnel during periodontal debridement is recommended to maintain adequate suctioning.11
CONCLUSION
Children with special health care needs are an underserved and vulnerable population. In the US, CP is the most common motor-related disability in pediatric populations. Providing lifelong care to people with CP requires an interdisciplinary effort with oral health professionals playing critical roles on the health care team. All children should be assessed for chronological developmental milestones as a screening mechanism for CP. Children with CP often exhibit the following impairments: limited sight, hearing, or speech; abnormal sensation and perception; recurrent seizures; inability to control bladder and bowel function; intellectual and learning disabilities; dysphagia and dyspnea; sensitive skin and/or pressure wounds; and difficulty in feeding. Making children with CP feel comfortable in the health care environment is an interdisciplinary responsibility. Implementing a tell-show-do approach and the use of anticipatory guidance may assist in providing a positive learning environment for pediatric populations during critical developmental years.
REFERENCES
- American Academy of Pediatric Dentistry Council on Clinical Affairs. Guideline on management of dental patients with special health care needs. Pediatr Dent. 2015;36:161–166.
- MyChild. The Ultimate Resource for Everything Cerebral Palsy. Available at: cerebralpalsy.org/ about-cerebral-palsy. Accessed November 12, 2015.
- National Institute of Neurological Disorders and Stroke. NINDS Cerebral Palsy Information Page. Available at: ninds.nih.gov/disorders/cerebral_ palsy/ cerebral_palsy.htm. Accessed November 12, 2015.
- Dougherty NJ. A review of cerebral palsy for the oral health professional. Dent Clin North Am. 2009;53:329–338.
- Centers for Disease Control and Prevention. Facts About Cerebral Palsy. Available at: cdc.gov/ncbddd/cp/facts.html. Accessed November 12, 2015.
- March of Dimes. Birth Defects. Available at: marchofdimes.org/baby/cerebral-palsy.aspx. Accessed November 12, 2015.
- Centers for Disease Control and Prevention. Data & Statistics for Cerebral Palsy. Available at: cdc.gov/ncbddd/cp/data.html. Accessed November 12, 2015.
- United Cerebral Palsy. Research and Statistics. Available at: ucp.org/resources/research-and-statistics. Accessed November 12, 2015.
- Centers for Disease Control and Prevention. Economic costs associated with mental retardation, cerebral palsy, hearing loss, and vision impairment—United States, 2003. MMWR Morb Mortal Wkly Rep. 2004;53:57–59.
- American Academy of Pediatrics. Cerebral Palsy. Available at: healthychildren.org/ English/health-issues/conditions/developmental-disabilities/pages/ Cerebral-Palsy.aspx. Accessed November 12, 2015.
- Kabani F. Special care for the dental patient with cerebral palsy. Presented at: Dallas County Dental Hygiene Society; January 8, 2015.
- Wynn RL, Meiller TF. Drug Information Handbook for Dentistry. 21st ed. Indianapolis: Wolters Kluwer; 2015.
- Wlkins E. Clinical Practice of the Dental Hygienist. 11th ed. Philadelphia: Lippincott Williams & Williams; 2013.
- Malamed S. Medical Emergencies in the Dental Office. 6th ed. St. Louis: Mosby; 2007.
- Kuperminc MN, Stevenson RD. Growth and nutrition disorders in children with cerebral palsy. Dev Disabil Res Rev. 2008;14:137–146.
From Dimensions of Dental Hygiene. December 2015;13(12):52–55.




