Treating Patients with Lupus
Following are simple strategies to help patients with this autoimmune disorder maintain their oral health.
This course was published in the October 2013 issue and expires 10/31/16. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain the classification system for lupus.
- Identify the prevalence of lupus.
- List the systemic signs and symptoms of lupus.
- Describe the oral manifestations of lupus and their treatment.
LUPUS DEFINED
Lupus is an autoimmune disorder of unknown etiology, although it may be related to genetic, environmental, or hormonal factors.2,3 It is a complex and potentially severe rheumatic disease in which the immune system attacks healthy cells, tissues, and organs, resulting in chronic inflammation. At present, there is no cure for lupus, and treatment options differ based on severity.2,4 Symptoms include, but are not limited to, joint pain/swelling, muscle pain, fever, rashes, chest pain, swollen glands, and fatigue. However, the classic feature of lupus is chronic inflammation. Patients with lupus experience periods of reoccurring acute or chronic inflammation called flares, and intervening periods of remission.2
Lupus is defined according to the following classification system: SLE, the most common and severe form of lupus, affects several parts of the body (joints, skin, kidneys, heart, lungs, blood vessels, and brain). Discoid lupus erythematosus (DLE) appears on the skin only and causes a rash that remains on the affected area. Subacute cutaneous lupus erythematosus causes sores on the skin when exposed to sunlight. Neonatal lupus is rare and affects newborn infants.3,5 Drug-induced lupus erythematosus (DILE) can be caused by certain medications that induce autoantibodies—namely, procainamide and hydralazine—but is usually temporary, with symptoms resolving upon cessation of the drug regimen.6
Oral complications of lupus may be directly related to the disease or caused by a medication used to treat the disease. Patients with lupus experience varied oral manifestations that include xerostomia, cracked lips, ulcers, periodontal diseases, lichen planus, and oral candidiasis.7
EPIDEMIOLOGY
Lupus is universally prevalent and varies within ethnic groups; generally, Blacks, Hispanics, Asians, and Native Americans are most frequently affected. In addition, lupus is more prevalent among women between the ages of 15 and 50 than men.2,3 The strongest risk factor for lupus is gender, with an approximate male to female ratio of 1:10. The average age of onset for women is 29 years.1,4,8 Moreover, women have more enhanced immune systems than men, and are 2.7 times more likely to acquire an autoimmune disease such as lupus.9 Worldwide incidence rates of SLE range from one to 10 per 100,000 people, and prevalence rates range from 20 to 70 per 100,000 people.4 According to recent statistics from the US Centers for Disease Control and Prevention, incidence rates in the US are difficult to obtain because the disease is difficult to diagnose. They vary widely, ranging from 1.8 cases to 7.6 cases per 100,000. Prevalence rates of SLE range from 14.6 cases to 68 cases per 100,000 people, with as many as 1,500,000 individuals affected.3,10 Lupus was once considered fatal, but now patients can potentially live years to decades after diagnosis.4 Survival rates at 5 years are 88% to 96%; at 10 years, they are 95% for young people, and 71% for older adults; and at 20 years, survival rates are 80%. The survival rates have improved primarily due to an increased incidence of early diagnosis and the introduction of additional treatment options.10

PATHOGENESIS
Research suggests that the immune system plays an important role in the development of lupus, but the cause of immune system dysfunction remains unknown.10 Researchers speculate that environmental factors may be the cause, but there is not enough consistent evidence to support this theory.10 In healthy people, the immune system protects the body; however, in patients with lupus, the immune system malfunctions and attacks healthy cells.2 SLE develops as a result of B-lymphocyte and T-lymphocyte dysregulation, autoantibody production, and immune complex formation. Cytokines are thought to have significant influence in the immune response system, and may explain the variations seen in clinical manifestations.10
Immunologic gene abnormalities in patients with lupus have been identified—interferon regulatory factor 5, protein tyrosine phosphatase nonreceptor type 22, and integrin alpha M—and are associated with increased susceptibility.8,10 Research suggests the concordance rate for identical twins is 24%, whereas the concordance rate for nonidentical twins is only 2%.8 Likewise, infants diagnosed with SLE within the first year of life show a high incidence of family members diagnosed with an autoimmune disease.10 A cumulative effect involving numerous genes is thought to result in SLE.8 Nevertheless, only three out of 100 children born to a parent with SLE will develop the disease.11

Hormonal abnormalities and environmental estrogens are associated with the pathogenesis of SLE. Metabolism of estrogen and androgen differs among women and men with lupus. Women with SLE metabolize estrogen to a more potent form, which may result in irregular menstrual cycles and increased risk of miscarriage. In fact, hormonal fluctuations in women tend to be associated with flares. High estrogen-to-androgen proportions in men may increase the risk of developing SLE. More research is needed, however, to understand how hormonal changes may lead to the development of lupus.8,10
Environmental triggers, such as sun exposure, infection, and certain medications, may be involved in the pathogenesis of SLE in predisposed patients.1 Photosensitivity to ultraviolet (UV) rays that cause a rash have been reported in almost 70% of patients with lupus.2 Autoantibody production has been found in 38% of patients with SLE who have been infected with the Epstein-Barr virus, but it is unclear whether the autoantibodies lead to the progression of SLE or just occur simultaneously.10 Approximately 80 drugs have been associated with DILE. Procainamide, hydralazine, and isoniazid are the predominant offenders, and can cause DILE in patients with genetic abnormalities.10 In 99% of DILE cases, symptoms disappear within 3 months of discontinuing the use of the drug.2
SIGNS AND SYMPTOMS
Lupus is a multisystem disease with a varied clinical course, ranging from a mild benign illness to a rapidly progressive illness culminating in organ failure and death. Lupus targets the central nervous system, heart, lungs, kidneys, reproductive system, blood, oral cavity, mucous membranes, gastrointestinal and musculoskeletal systems, and skin.8 The most common symptoms of SLE include severe fatigue, weight loss, malaise, myalgia, joint pain, mucocutaneous lesions, and lymphadenopathy.1 The earliest manifestation of lupus is arthralgia (joint pain), which usually affects the hands, wrists, and knees.10 In some patients, arthralgia may cause temporomandibular joint (TMJ) discomfort.1 Skin manifestations include generalized sun-induced rashes and discoid (flat and round) lesions.1 The classic malar or butterfly rash on the face is a common skin manifestation (Figure 1).1,2,9,10 Hair loss, caused by hair follicles becoming plugged with keratin, is also common.1
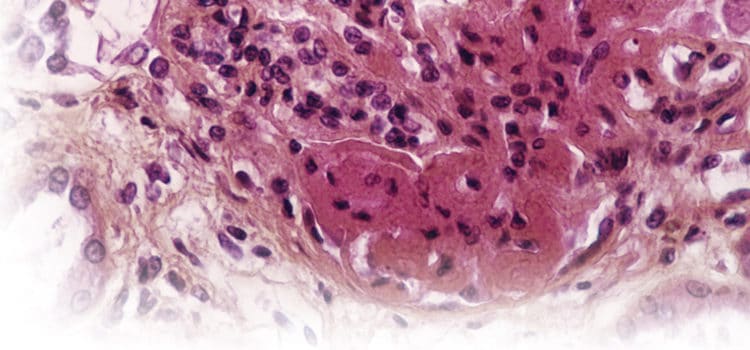
DLE manifests as hyperkeratotic (thickened) lesions, resulting in scarring and loss of skin pigmentation (Figure 2). Mucocutaneous lesions, such as marginal gingivitis, desquamative gingivitis, and mucosal ulcerations, occur in 40% to 50% of patients.10 Patients with advanced stages of lupus may present with Sjögren’s syndrome (dryness of the mouth, skin, and eyes), which increases caries risk.1,10 Flares may be triggered by a multitude of factors, including, but not limited to, stress, increased work load, emotional problems, exposure to sunlight, pregnancy, and noncompliance with medication regimens.10
DIAGNOSIS
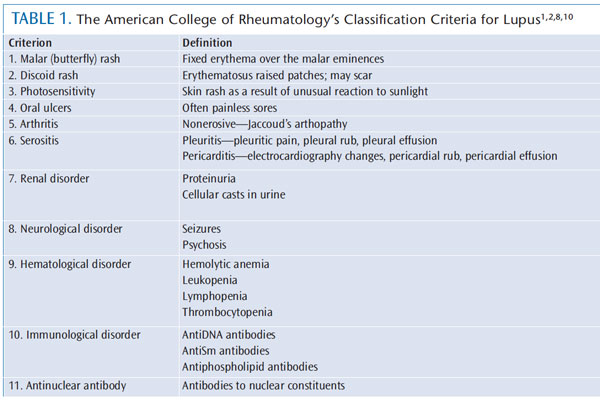
Diagnosing lupus may prove difficult, as there are many unknown causes and multiple organ systems involved. As a result, permanent organ damage may occur before treatment begins.8 The American College of Rheumatology (ACR) has developed criteria to help in the diagnosis of lupus. The following classification system is used to establish a baseline for diagnosis: malar rash, discoid rash, photosensitivity, oral ulcers, nonerosive arthritis, serositis, renal disorder, neurologic disorder, hematologic disorder, immunologic disorder, or antinuclear antibody positive. A person is diagnosed with lupus if he or she meets four or more of the 11 classification criteria, either simultaneously or in succession (Table 1).1,2,8,10
TREATMENT OPTIONS
The ultimate goals of SLE management are to focus on prevention, inflammation reversal, symptom management, and extending remission periods.1 Several specialists may be involved in treating patients with lupus, including rheumatologists, clinical immunologists, nephrologists, hematologists, dermatologists, neurologists, cardiologists, and endocrinologists. Patients may receive medical treatment from one or more specialized health care professionals, depending on the extent of organ involvement and severity of disease.5 Oral health professionals are a valuable asset to the interprofessional team due to the oral manifestations of lupus. For example, oral ulcers rank fourth on the ACR’s criteria for the classification of lupus.

Nonsteroidal anti-inflammatory drugs (NSAIDs), such as COX-2 inhibitors, and antimalarial drugs, corticosteroids, and immunosuppressants are all used to treat lupus.12 NSAIDs are commonly prescribed because approximately 90% of people with lupus develop arthralgia or polyarthritis. In addition reduce fever, pain, and pleurisy.10 Antimalarial drugs are used to treat and prevent flares, and they are particularly useful when arthralgia is not controlled by NSAIDs.10 In addition, antimalarial medicines aid in the treatment of skin rashes, mouth ulcers, and joint pain.11 Corticosteroids help decrease swelling, warmth, pain, and tenderness. Lastly, immunosuppressants control inflammation and overactive immune systems, particularly when steroids have failed to manage symptoms.11
In March 2011, the US Food and Drug Administration approved belimumab, an immunosuppressive drug, for adults with active autoantibody-positive SLE. It is the first new drug approved for the treatment of lupus in more than 50 years.3,10 Auto-antibodies are the leading cause of tissue damage among patients with lupus.2
Beyond pharmacotherapy, proper sun protection against UVA and UVB rays, avoiding tanning beds, and smoking cessation may help reduce symptoms. Regular exercise and consuming a diet rich in vitamin D and calcium are important for patients taking glucocorticoids.10 Pycnogenol, a plant extract obtained from the bark of a French maritime pine, has shown strong antioxidant activity and may be useful in reducing inflammatory effects of SLE. More research is warranted.13
WHAT THE FUTURE MAY HOLD
Stem cells may present several options for the future treatment of many diseases. Research suggests that stem cells retrieved from adult blood or bone marrow may provide benefits for certain patients with autoimmune and cardiovascular disorders.9 Stem cells are believed to modulate the immune system, and dental stem cells harvested from the pulp of teeth have exhibited immunoregulatory and immunosuppressive properties.14 With the current medication options used to treat lupus, the side effects can be just as troubling as the clinical manifestations of the disease. Over time, stem cell therapy could result in an alternative option to medications or offer a hybrid approach in treating patients with lupus.
DETECTION AND MANAGEMENT OF ORAL MANIFESTATIONS
Oral health professionals play a vital role in the early detection and multidisciplinary management of lupus.1,15 Manifestations of lupus in the oral mucosa are quite common. 15,16 Unfortunately, many initial investigations by health care providers do not incorporate a thorough exam of the oral cavity, thus delaying early diagnosis and intervention strategies.15,16
Research pertaining to oral manifestations has been limited to individuals with SLE and DLE.15 A variety of oral mucosal lesions are reported, and include gingivitis, erythematosus patches (red mucosal macules and plaques), cheilitis (Figure 3), honeycomb plaques, discoid lesions, mucosal ulcers, recurrent aphthous stomatitis, and leukoplakia or lichen planus-like lesions.1,15,16 A correlation between oral lesions and increased disease activity (flares) and duration has been established. 17 The classic oral lesion is described as a whitish plaque, red in the center, with keratotic, white irradiating striae (thickened stripes or bands) at the periphery, and is most often found on the hard palate, lips, and buccal mucosa.15,18 Lupus-related lesions require biopsy for definitive diagnosis, as they can mimic those of erythemia multiforme, lichen planus, and other vesiculobullous lesions.1,15 Chronic ulcers must be monitored carefully, due to the increased risk of transforming into squamous cell carcinomas.
Patients with lupus may also be affected by other orofacial manifestations, such as xerostomia or burning (caused by medications or Sjögren’s syndrome); candidiasis (due to immunosuppressive therapy); periodontal diseases (due to lack of oral hygiene caused by the presence of painful ulcers); TMJ disorder (joint pain with limited opening and lateral movement); and dysgeusia (medication induced alteration of taste).17 Oral manifestations should be treated with standard palliative care and more aggressive periodontal therapy when indicated.15 Patients who have had lupus for a long time and are on a high prednisone regimen are at increased risk of gingivitis, delayed primary and permanent tooth eruption, and twisted root formation, while patients taking immunosuppressants experience more TMJ impairment.19 Immunosuppressive drugs may also increase the risk of infection and delay healing, both of which are concerns when providing dental treatment.18
DENTAL CONSIDERATIONS
As with all patients, a thorough health history should be completed and reviewed prior to beginning dental procedures.7 Patients who have SLE with major organ involvement may warrant special considerations, such as seeking consultation with their physician or rheumatologist prior to beginning dental care. This is due to existing medical conditions or the risk that dental treatment could affect the functions of the kidneys, heart, lungs, and anticoagulant or immune thrombocytopenic system.7
Kidney function may become compromised when tetracycline or analgesics, such as aspirin or NSAIDs, are taken prior to medical consultation. Patients with mitral valve prolapse, antiphospolipid syndrome, or Liebman-Sacks endocarditis require prophylactic antibiotics before dental procedures. 7 Previously, all patients with SLE required antibiotic prophylaxis prior to dental procedures; however, this may no longer be necessary (but should be confirmed with the patient’s physician).11 The use of nitrous oxide is contraindicated for patients with lupus, due to its ability to depress breathing. Lastly, patients with lupus anticoagulant or immune thrombocytopenic purpura may have abnormal bleeding during extractions and periodontal surgery; therefore, treatment must be performed with great caution.7
As with all patients, a comprehensive oral cancer screening should be performed at each visit. This screening is imperative for patients with SLE because they are predisposed to severe head and neck infections that may progress rapidly with immunosuppressive therapy, which may raise their risk of oral cancer.1 Approximately 95% of patients with lupus present with oral manifestations; therefore, patients may benefit from recare visits every 3 months to 4 months.7 Maintaining proper oral hygiene care in this patient population is especially important.1 Patients with lupus should be instructed to use a soft-bristled toothbrush, toothpaste without sodium lauryl sulfate for those with oral ulcerations, and oral care products with fluoride to reduce acidity, caries, and potential infection.7,11,14 Furthermore, these patients may need to avoid hot/spicy foods and acidic fruits, as they can aggravate oral sores and lesions.7,11 Those with photosensitivity often have dry and scaly lips that would benefit from a lip balm with SPF.14 Dental hygienists are encouraged to provide patients with up-to-date education on oral health maintenance and oral hygiene aids.
CONCLUSION
Lupus is an autoimmune connective tissue disease that displays a broad spectrum of clinical and immunological manifestations resulting in inflammation, organ damage, and loss of function. Although the etiology is unknown, lupus is thought to derive from a complex interaction of genes, hormones, and the environment. The disease is characterized by periods of illness (flares) and remission, and most often affects women of color and of childbearing age. Several organ systems may be affected by lupus, with many patients experiencing oral complications. In some instances, the medications used to treat lupus create oral manifestations that result in a greater susceptibility to head/neck infections, or impaired healing after dental procedures. The dental team shares the important role of identifying and treating oral lesions, in addition to continuous reinforcement of the need to maintain adequate oral hygiene. A multidisciplinary or comprehensive medical-dental management approach is recommended and beneficial when treating patients with lupus.
References
- Albilia JB, Lam DK, Clokie CM, Sándor GK.Systemic lupus erythematosus: a review for dentists. J Can Dent Assoc. 2007;73:823–828.
- Ferenkeh-Koroma A. Systemic lupus erythematosus: nurse and patient education. Nurs Stand. 2012;26:49–57.
- Centers for Disease Control and Prevention.Systemic lupus erythematosus. Available at: www.cdc.gov/arthritis/basics/lupus.htm. Accessed September 17, 2013.
- Pons-Estel GJ, Alarcón GS, Scofield L, Reinlib L,Cooper GS. Understanding the epidemiology and progression of systemic lupus erythematosus. Semin Arthritis Rheum. 2010;39:257–268.
- National Institutes of Health. What isLupus? Available at: www.niams.nih.gov/Health_Info/ Lupus/lupus_ff.pdf. Accessed September 17, 2013.
- Schoonen WM, Thomas SL, Somers EC, et al.Do selected drugs increase the risk of lupus? A matched case-control study. Br J Clin Pharmacol. 2010;70:588-596.
- Galusha-Phillips, H. Lupus Guide to DentalCare. Available at: www.lupusgreaterohio.com/public/documents/Lupus%20Guide%20to%20Dental%20Care.pdf. Accessed September 19, 2013.
- Systemic Lupus Erythematosus: A Primer for Managed Care. Available at: www.ajmc.com/ publications/supplement/2012/SLE-Primer-for-Managed-Care/May12. Accessed September 17, 2013.
- Goldie MP. What to do when the body turnson itself. Dental Nursing. 2012;8(8):494–500.
- Bailey T, Rowley K, Bernknopf A. A review of systemic lupus erythematosus and current treatment options. Formulary. 2011;46(5): 178–94.
- Wake C. Systemic lupus erythematosus understanding the condition. Dental Health. 201;50(6):18–20.
- Amissah-Arthur MB, Gordon C. Contemporary treatment of systemic lupus erythematosus: an update for clinicians. Ther Adv Chronic Dis. 2010;1:163–175.
- Lupus Foundation of America. Medications to Treat Lupus Symptoms. Available at: www.lupus.org/answers/entry/medications-totreat-lupus. Accessed September 17, 2013.
- Fernandes EG, Savioli C, Siqueira JT, Silva CA.Oral health and the masticatory system in juvenile systemic lupus erythematosus. Lupus. 2007;16:713–719.
- D’Andrea G. Pycnogenol: A blend of procyanidins with multifaceted therapeutic applications? Fitoterapia. 2010;81:724–736.
- Mays JW, Sarmadi M, Moutsopoulos NM. Oral manifestations of systemic autoimmune and inflammatory diseases; diagnosis and clinical management. J Evid Base Dent Pract. 2012;12(Suppl):265–282.
- Lupus Foundation of America. Oral disease.Available at: www.lupus.org/resources/15-questions-oral-issues-with-lupus. Accessed September 17, 2013.
- Khatibi M, Shakoorpour AH, Jahromi ZM,Ahmadzadeh A. The prevalence of oral mucosal lesions and related factors in 188 patients with systemic lupus erythematosus. Lupus. 2012;21:1312–1315.
- Ergun S, Katz J, Cifter ED, Koray M, Esen BA,Tanyeri H. Implant-supported oral rehabilitation of a patient with systemic lupus erythematosus: case report and review of the literature. Quintessence Int. 2010;41:863–867.
From Dimensions of Dental Hygiene. October 2013;11(10):53–57.



