Treating Patients With Cancer
Diet plays an integral role in promoting oral health.
This course was published in the August 2014 issue and August 31, 2017. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- List the oral side effects of cancer treatments and drug-related manifestations in patients with head and neck cancer.
- Discuss the complications of polypharmacy.
- Describe the dental management of patients with head and neck cancer.
In the United States, heart disease remains the number one cause of death, but the percentage of deaths caused by cancer has been rising—from 19.2% in 1975 to 23.3% in 2010.1 According to data from the Surveillance, Epidemiology, and End Results Program, 10.8% of primary cancer sites were detected in the oral cavity and pharyngeal area between 1975 and 2010.1 The treatment of this relatively small subcategory of cancers, however, has a disproportionate impact on patients’ quality of life.2,3 As key members of the interprofessional cancer treatment team, dental hygienists can assist patients with head and neck cancer manage the oral side effects of treatment, which can be devastating, as well as educate them on effective self-care strategies.
CANCER TREATMENT
Three treatment options are usually employed for head and neck cancers: surgery, radiation therapy, and chemotherapy. The three options may be provided separately or in combination, based on the stage and origin of the cancer.4,5 Various surgical techniques are used to remove the physical site of the cancer, such as the area of malignant tumor growth.5 Radiation therapy is used to shrink tumors or kill cancer cells by damaging their DNA.4 Chemotherapy reduces the risk of the cancer spreading by destroying rapidly dividing cancer cells at different points in the cell cycle. It is also utilized when cancer has already metastasized because radiation and surgery are only effective when cancer is localized. Additionally, chemotherapy increases the efficacy of radiation on malignant cells.2,6
Patients undergoing treatment for head and neck cancer may experience a variety of uncomfortable and painful side effects, especially in the oral cavity.7 This is because the treatments, while effective against cancer, injure healthy cells at the same time.2
SIDE EFFECTS
Oral mucositis is one of the most debilitating side effects of cancer therapy and is caused by both chemotherapy and radiation therapy.8 It is a common nonhematological complication that causes inflammation and ulceration, making it difficult to eat, swallow, speak, and perform proper oral hygiene.8,9 These effects, in turn, may result in weight loss, nutritional deficiencies, dehydration, increased risk of oral infections, and long-term dysphagia due to atrophy of the pharyngeal muscles.8,10,11 Symptoms of oral mucositis may become so severe that they interfere with cancer treatment. Sometimes cancer therapy must be postponed until the patient becomes well enough to eat and drink.8
Radiation therapy may cause xerostomia. It can hinder the production of saliva—the main biological defense against demineralization. Saliva also provides a buffer against pH fluctuation in the oral cavity and serves as a medium for fluoride dissemination.2,12 Reduction in salivary flow not only increases the risk of caries, but can also significantly interfere with a patient’s intake of solids and liquids—complicating nutritional status and quality of life.11,12
Nausea and vomiting are side effects of chemotherapy that are both physically and psychologically burdensome.13 Despite significant advances in antiemetic medicine, approximately 50% of patients with cancer who undergo treatment experience nausea and vomiting.14 Even with the antiemetic treatments, the benefits of chemotherapeutic drugs can be counteracted by their side effects.15
Oral viral, bacterial, and fungal infections are common in patients with cancer, and can manifest for years after initial cancer therapy is completed. Candidiasis is the most common infection among patients with cancer, due to the diminished level of salivary output. The clinical presentations include pseudomembranous candidiasis or thrush (Figure 1); erythematous candidiasis (red appearance); hyperplastic candidiasis, which causes white tissue overgrowth (Figure 2); and angular cheilitis, or redness at the corners of the mouth (Figure 3).16
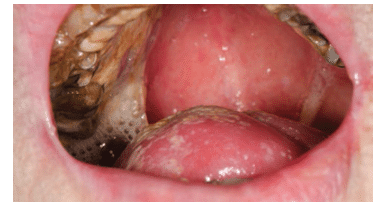 FIGURE 1. Pseudomembranous candidiasis, or thrush, is a side effect of head and neck cancer treatment due to diminished salivary flow. FIGURE 1 TO FIGURE 3. DR P. MARAZZI/SCIENCE PHOTO LIBRARY
FIGURE 1. Pseudomembranous candidiasis, or thrush, is a side effect of head and neck cancer treatment due to diminished salivary flow. FIGURE 1 TO FIGURE 3. DR P. MARAZZI/SCIENCE PHOTO LIBRARY
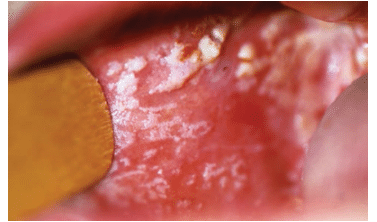 FIGURE 2. Hyperplastic candidiasis causes white tissue overgrowth. FIGURE 1 TO FIGURE 3. DR P. MARAZZI/SCIENCE PHOTO LIBRARY
FIGURE 2. Hyperplastic candidiasis causes white tissue overgrowth. FIGURE 1 TO FIGURE 3. DR P. MARAZZI/SCIENCE PHOTO LIBRARY
 FIGURE 3. Angular cheilitis, or redness at the corners of the mouth, is a common side effect of cancer treatment.
FIGURE 3. Angular cheilitis, or redness at the corners of the mouth, is a common side effect of cancer treatment.
FIGURE 1 TO FIGURE 3. DR P. MARAZZI/SCIENCE PHOTO LIBRARY
DRUG-RELATED MANIFESTATIONS
Patients with cancer are vulnerable to drug-related manifestations because chemotherapeutic drugs possess narrow therapeutic indices and are often harmful to healthy cells.17 For patients undergoing treatment for one or more comorbid systemic diseases, managing the side effects created by the polypharmacy, along with the cancer therapy, can create a variety of complications. Patients taking multiple medications, women, and older adults are at increased risk of drug-related complications.18 The use of corticosteroids, anticoagulates, and antihypertensive drugs increases the incidence of hospitalization due to adverse drug interactions during chemotherapy. The risk of a negative event due to drug interaction is eight times higher among patients receiving drugs for comorbid conditions than for patients receiving only supportive care during cancer treatment.19
CHEMOTHERAPY
Many types of chemotherapy drugs are available. These drugs are categorized by factors such as how they work in the disruption of the cancer cell growth cycle, their chemical structure, and how they interact with one another.20 Alkylating agents work in all phases of the cell cycle by directly damaging the cell’s DNA to prevent the cancer cell from reproducing. Alkylating agents are divided into several different classes, such as nitrogen mustards, nitrosoureas, alkyl sulfonates, triazines, and ethylenimines. Platinum-based antineoplastic drugs (eg, cisplatin) are sometimes grouped with alkylating agents because they disrupt the cells in a similar way. Because these drugs directly affect cell DNA, they can cause long-term damage to the bone marrow. Anti-metabolites disrupt the growth of cells in DNA and RNA by substituting for their normal components. This damages the cells during the synthesis phase of the cell cycle.20
Antitumor antibiotics interfere with the enzymes involved in DNA replication. Lifetime dose limits are placed on these drugs because they can permanently damage the heart when given in high doses. Topoisomerase (I and II) inhibitors directly interfere with the enzyme topoisomerase, which helps separate DNA strands so they can be copied. These drugs increase the risk of developing acute myelogenous leukemia.20
Mitotic inhibitors work during the mitosis phase of the cell cycle but they can damage the cells in all phases. They either stop mitosis or inhibit enzymes from making the proteins needed for cell reproduction. They also have dose limits due to the risk of peripheral nerve damage.20
POLYPHARMACY MANAGEMENT
Corticosteroid drugs, such as prednisolone and dexamethasone, may be used in conjunction with cancer therapy. They provide many benefits, including: helping prevent inflammation during radiation therapy; serving as a concurrent antiemetic therapy during chemotherapy; and increasing appetite.20,21 Side effects of corticosteroids include sleep problems, fluid retention, hyperglycemia, and weight gain. Hyperglycemia may increase the risk of diabetes, thereby increasing susceptibility to infections, depending on how long the steroid drug is used in conjunction with cancer therapy.21,22
Some patients may take anticoagulates (eg, aspirin, warfarin) to treat thrombolytic heart conditions, such as myocardial infarction and stroke, or to prevent cardiovascular diseases. Bleeding complications are possible in patients on this drug regimen and recent international normalized ratio level (a test used to monitor the efficacy of anticoagulants) should be obtained.23,24 Drug interactions should also be carefully monitored, as anticoagulant drugs may interact with antihypertensive and corticosteroid drugs, and some anticancer drugs may intensity the effects of warfarin.19
The use of antihypertensives often causes xerostomia. Antihypertensive drugs may also interact with anticancer agents and may prolong neutropenia, a reduction in neutrophils, which also occurs during chemotherapy. This increases the risk of infection.2,19,25
DENTAL MANAGEMENT
Patients with head and neck cancer experience significant and persistent physical, functional, and psychosocial problems, ranging from nausea, vomiting, oral mucositis, dysphagia, and xerostomia to psychologically debilitating problems, such as depression and social isolation.3
Traditionally, cancer treatments focused on objective measurements, such as survival rates, tumor recurrence, or toxicity grading. While such measurements are important, they do not reflect patients’ quality of life.26 As dental professionals, it is important to coordinate with patients’ medical teams, including oncologists and surgeons, to maintain and improve their quality of life before, during, and after cancer treatment.
Before receiving any type of cancer treatment, patients should receive comprehensive oral exams, along with education about maintaining optimal self-care routines. They should also undergo any necessary preventive therapies or restorative treatments/extractions in order to improve oral function.24,27 All dental visits should take place at least 4 weeks prior to the start of cancer treatment, in order for patients to properly heal. This is especially important for patients receiving radiation because maintaining optimal oral health is the best defense against this therapy’s severe oral side effects.4
Oral health professionals should consult with patients’ medical teams to remain up-to-date on whether any invasive procedures have been performed, and to alert them to any changes in dental treatment plans in case there is a need for prophylactic antibiotics.4,24
Dental hygienists play a crucial role during patients’ cancer treatment. Because long-term physical health and survival are the top priorities, oral health is often seen as less important while patients undergo cancer treatment. Fewer problems occur during cancer therapy when oral disease is eliminated and oral prophylaxis is regularly performed to reduce the bacterial load. Excellent oral hygiene must also be maintained throughout treatment. Patients must be educated on the importance of oral health and the impact it has on their quality of life.2,27,28
Virtually all patients who undergo cancer therapy, especially radiation, will experience oral mucositis.24,29,30 Because of this, patients should be instructed to remove biofilm twice daily through brushing with an extra-soft toothbrush, as well as daily flossing.2 Patients should also be instructed to eat a soft, bland diet, avoiding spicy or acidic foods.31 Toothpastes with sodium lauryl sulfate, which can irritate soft tissues, should not be used.30 Chlorhexidine mouthrinses are not recommended during cancer therapy—especially among patients receiving head and neck radiation and those who already have mucositis—because they may cause taste alteration, burning sensation, and mucosal irritation.31,32 When patients receive chemotherapy drugs, cryotherapy, or holding ice in the mouth, may help reduce oral mucositis.31
Patients may also need to implement measures to relieve symptoms of xerostomia. To ease xerostomia and decrease caries risk, patients should be instructed to sip water frequently and use saliva substitutes or moistening gels. Salivary substitutes should be used for symptom relief, as well as nonmedicated oral rinses containing bicarbonate or fluoride.33 Rinsing with water frequently can also lessen the effects of vomiting on the oral cavity by neutralizing the acidic environment.12 Sialogogues, such as chewing gum and pilocarpine, may be used for the relief of symptoms; however, pilocarpine can cause sweating, diarrhea, and bronchospasm in some people.33
Oral infections can be prevented by maintaining good oral hygiene, routine rinsing and moistening of the oral cavity, and using antifungal, antiviral, or antibacterial medications as necessary.16
CONCLUSION
The World Health Organization defines quality of life as affected by patients’ ”physical health, psychological state, level of independence, social relationships, and their relationships to salient features of their environment.”34 Among patients with head and neck cancer, quality of life measurements have been shown to affect survival rates.35–37 To support quality of life and improve treatment response, side effects of any prescribed treatment should be minimized to an appropriate benefit/risk ratio.11 Drug-related side effects need to be accurately communicated to patients. In order to prevent or minimize drug toxicities, adjunctive dental therapies should be discussed with patients’ medical teams.11,31 Dental examinations and treatments should continue throughout active cancer treatment and throughout patients’ lifetimes.31
REFERENCES
- National Cancer Institute. SEER Cancer Statistics Review, 1975-2010. Available at: seer.cancer.gov/ csr/1975_2010. Accessed July 17, 2014.
- Stefan SA. Cancer care. Dimensions of Dental Hygiene. 2010;8(9):66–69.
- Ojo B, Genden EM, Teng MS, Milbury K, Misiukiewicz KJ, Badr H. A systematic review of head and neck cancer quality of life assessment instruments. Oral Oncol. 2012;48:923–937.
- Whisenhunt J, Puette ES, Saylor AL. Caring for patients with oral cancer. Dimensions of Dental Hygiene. 2012;10(9):54–59.
- American Cancer Society. Surgery for oral cavity and oropharyngeal cancer. Available at: cancer.org/cancer/oralcavityandoropharyngealcancer/detailedguide/oral-cavity-and-oropharyngeal-cancer-treating-surgery. Accessed July 17, 2014.
- Oral Cancer Foundation. Chemotherapy. Available at: oralcancerfoundation.org/ treatment/chemotherapy.php. Accessed July 17, 2014
- Fang FM, Tsai WL, Chen HC, et al. Intensity-modulated or conformal radiotherapy improves the quality of life of patients with nasopharyngeal carcinoma: comparisons of four radiotherapy techniques. Cancer. 2007;109:313–321.
- Qutob AF, Gue S, Revesz T, Logan RM, Keefe D. Prevention of oral mucositis in children receiving cancer therapy: a systemic review and evidence-based analysis. Oral Oncol. 2013;49:102–107.
- Cheng KKF, Lee V, Li CH, et al. Incidence and risk factors of oral mucositis in paediatric and adolescent patients undergoing chemotherapy. Oral Oncol. 2011;47:153–162.
- Bossi P, Numico G, De santis V, et al. Prevention and treatment of oral mucositis in patients with head and neck cancer treated with (chemo) radiation: report of an Italian survey. Support Care Cancer. 2014;22:1889–1896.
- Watters AL, Epstein JB, Agulnik M. Oral complications of targeted cancer therapies: a narrative literature review. Oral Oncol. 2011;47:441–448.
- Szalma P, Yoon S. Enhance remineralization. Dimensions of Dental Hygiene. 2013;11(5):42–46.
- Abidi MH, Tageja N, Ayash L, et al. Aprepitant for prevention of nausea and vomiting secondary to high-dose cyclophosphamide administered to patients undergoing autologous peripheral blood stem cells mobilization: a phase II trial. Support Care Cancer. 2012;20:2363–2369.
- Pirri C, Bayliss E, Trotter J, et al. Nausea still the poor relation in antiemetic therapy? The impact on quality of life and psychological adjustment of nausea, vomiting and appetite loss, individually and concurrently as part of a symptom cluster. Support Care Cancer. 2013;21:735–748.
- Eren OO, Ozturk MA, Oyan B. Cancer related fatigue: can it be due to adrenal suppression secondary to high-dose steroids used as antiemetic? Support Care Cancer. 2014 Jan 19. Epub ahead of print.
- Elad S, Meyerowitz C. Late oral adverse effects of cancer treatments. In: Philip R, Louis CS, Marks S, Lawrence B, eds. ALERT: Adverse Late Effects of Cancer Treatment. New York: Springer; 2014:141–166.
- Cohen MR, Anderson RW, Attilio RM, Green L, Muller RJ, Pruemer JM. Preventing medication errors in cancer chemotherapy. Am J Health-Syst Pharm. 1996;53:737–746.
- Chan A, Soh D, Ko Y, Huang YC, Chiang J. Characteristics of unplanned hospital admissions due to drug-related problems in cancer patients. Support Care Cancer. 2014;22:1875–1881.19.
- Riechelmann RP, Tannock IF, Wang L, Saad ED, Taback NA, Krzyzanowska MK. Potential drug interactions and duplicate prescriptions among cancer patients. J Natl Cancer Inst. 2007;99:592–600.
- American Cancer Society. Different Types of Chemotherapy Drugs. Available at: cancer.org/treatment/treatmentsandsideeffects/treatmenttypes/chemotherapy/chemotherapyprinciplesanindepthdiscussionofthetechniquesanditsroleintreatment/chemotherapy-principles-types-of-chemo-drugs. Accessed July 17, 2014.
- American Cancer Society. Anti-nausea/Vomiting Medicines. Available at: cancer.org/treatment/treatmentsandsideeffects/physicalsideeffects/nauseaandvomiting/nauseaandvomiting/nausea-and-vomiting-drugs. Accessed July 17, 2014.
- Vigneri P, Frasca F, Sciacca L, Pandini G, Vigneri R. Diabetes and cancer. Endocr Relat Cancer. 2009;16:1103–1123.
- van Diermen DE, van der Waal I, Hoogstraten J. Management recommendations for invasive dental treatment in patients using oral antithrombotic medication, including novel oral anticoagulants. Oral Medicine. 2013;116:709–716.
- Tavoc T. Symptom management. Dimensions of Dental Hygiene. 2013;11(7):59–63.
- Hsieh MM, Everhart JE, Byrd-Holt DD, Tisdale JF, Rodgers GP. Prevalence of neutropenia in the US population: age, sex, smoking status, and ethnic differences. Ann Intern Med. 2007;146:486–492.
- Klein J, Livergant J, Ringash J. Health related quality of life in head and neck cancer treated with radiation therapy with or without chemotherapy: a systematic review. Oral Oncology. 2014;50:254–262.
- Dockter KM. Oral implications of cancer treatment. Dimensions of Dental Hygiene. 2011;9(6):74–79.
- Greco N. Xerostomia and the cancer patient. Dimensions of Dental Hygiene. 2007;5(1):28–30.
- Sonis ST. Oral mucositis. Anticancer Drugs. 2011;22:607–612.
- Oral Cancer Foundation. Mucositis. Available at: oralcancerfoundation.org/complications/ mucositis.php. Accessed July 17, 2014.
- Keefe DM, Schubert MM, Elting LS, et al. Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer. 2007;109:820–831.
- Farah CS, McIntosh L, McCullough MJ. Mouthwashes. Aust Prescr. 2009;32:162–164.
- Beech N, Robinson S, Porceddu S, Batstone M. Dental management of patients irradiated for head and neck cancer. Aust Dent J. 2014;59:20–28.
- World Health Organization. WHOQOL Measuring Quality of Life. Available at: who.int/mental_health/media/68.pdf. Accessed July 17, 2014.
- Meyer F, Fortin A, Gelinas M, et al. Health-related quality of life as a survival predictor for patients with localized head and neck cancer treated with radiation therapy. J Clin Oncol. 2009;27:2970–2976.
- Karvonen-Gutierrez CA, Ronis DL, Fowler KE, Terrell JE, Gruber SB, Duffy SA. Quality of life scores predict survival among patients with head and neck cancer. J Clin Oncol. 2008;26:2754–2760.
- Scharpf J, Karnell LH, Christensen AJ, Funk GF. The role of pain in head and neck cancer recurrence and survivorship. Arch Otolaryngol Head Neck Surg. 2009;135:789–794.
From Dimensions of Dental Hygiene. August 2014;12(8):26–29.



