
The Role of Fluoride In Caries Prevention
Fluoride is one of the most valuable weapons in the fight against tooth decay among pediatric patients.
Dental caries remains a public health concern. In the United States, it is the most common chronic disease of childhood.1 Globally, untreated caries in primary teeth is the 10th most common chronic condition in children, impacting 621 million individuals.2 Data from the US National Health and Nutrition Examination Survey 2011-2012 revealed that 23% of children between the ages of 2 and 5 and 56% of children between the ages of 6 and 8 experienced dental caries in a primary tooth.3 Among permanent dentition, 21% of children between the ages of 6 and 11 experienced dental caries.3 Of those children, 6% had untreated dental caries.3 The data also revealed that race and ethnicity play a role in dental caries prevalence among children between the ages of 2 and 8. For example, Hispanic (46%), and non-Hispanic black children (44%) had more reported dental caries than non-Hispanic white children (31%).3
Caries is preventable with proper implementation of preventive measures by parents/caregivers and dental and medical professionals, and fluoride is one of the most effective strategies for preventing tooth decay.
SOURCES OF FLUORIDE
Fluoride is found in community water sources, foods, toothpastes, mouthrinses, and professional products. Roughly, 72% of the US population has fluoridated water.4 Current drinking water recommendations are 0.7 mg of fluoride/liter (mg/L) to prevent dental caries.5 This concentration provides a balance of reducing dental caries while minimizing the risk of dental fluorosis.5 Children who reside in communities with fluoridated tap water have less tooth decay than children who reside in nonfluoridated communities.1 The consumption of fluoridated water reduces dental caries in about 25% of children and adults.6
Infant formula and formula concentrate contain fluoride. In previous years, the US Centers for Disease Control and Prevention (CDC) and the American Dental Association (ADA) suggested using low-fluoride water to prepare infant formula to minimize the risk of dental fluorosis.4 However, with the current reduced fluoride concentration in drinking water (0.7 ppm), the ADA supports the use of tap water to prepare infant formula.7 Parents/caregivers should monitor their children’s exposure to fluoride to prevent dental fluorosis.
Fluoride is also found in processed foods and beverages. A study by Martinez-Mier et al8 evaluated fluoride concentrations found in foods and beverages. Grains, meats, and fish revealed the highest fluoride concentrations, followed by fruits and dairy products.8
Manufactured sources of fluoride include toothpaste, mouthrinse, professionally applied products, and supplements. The CDC does not recommend that children younger than 2 use fluoride toothpaste unless prescribed by an oral health or medical professional.1However, the ADA suggests that children’s deciduous teeth be brushed twice per day with a tiny smear of fluoride toothpaste as soon as they erupt. The ADA also recommends children age 3 and younger use no more than a smear or grain-of-rice-size amount of fluoride toothpaste.9 Children ages 3 to 6 should use no more than a pea-size amount of fluoride toothpaste during toothbrushing.10Regardless of age, young children should be directly supervised while toothbrushing to minimize the risk of ingestion. Fluoride mouthrinses can be effective in caries prevention for children ages 6 to 18.4 A systematic review determined that the use of a prescription-strength mouthrinse containing 900 ppm fluoride (0.09%) at least weekly reduced dental caries risk.4
Professionally applied acidulated phosphate fluoride (APF) gels and foams were the most widely used method of in-office application in the US from the late 1960s to the early 2000s.11 APF gels and foams reduce the incidence of dental caries in primary and permanent teeth.11 Both APF gel and foam have a fluoride concentration of 12,300 ppm.11 The use of APF gel or foam on infants, young children, and patients with disabilities is no longer recommended due to the risk of ingestion.12 Fluoride varnish has overtaken APF gels and foams as the most common form of professional fluoride application.13 A panel convened by the ADA Council on Scientific Affairs recommends the application of 2.26% fluoride varnish or 1.23% fluoride APF gel, or a prescription-strength, home-use 0.5% fluoride gel or paste or 0.09% fluoride mouthrinse for patients age 6 and older who are at risk of dental caries. For children younger than 6, the panel only recommends 2.26% fluoride varnish.11
In 2014, the US Preventive Services Task Force (USPSTF) recommended the use of fluoride varnish in all children, from birth through age 5 and gave a B evidence grade for its use.12 A grade B implies the USPSTF recommends the service, and “there is a high certainty the net benefit is moderate,” or “there is moderate certainty that the net benefit is moderate to substantial.”12
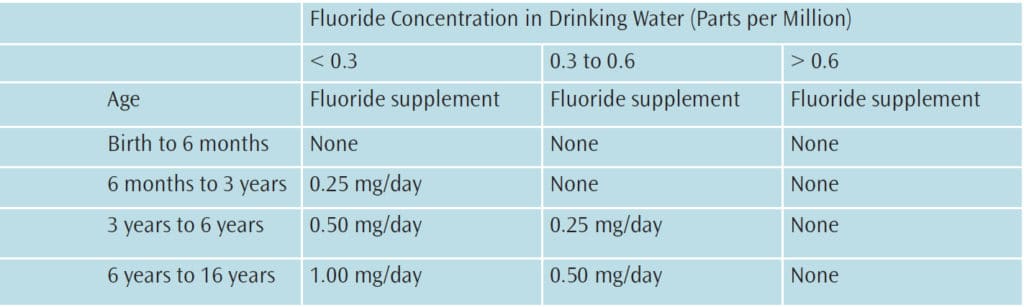
Children who are at high risk for caries and who have no or suboptimal exposure to fluoride may benefit from prescribed dietary fluoride supplements.14,15 The following dietary supplement schedule is recommended when fluoride ion concentration is low in drinking water, and children are at high risk for caries (Table 1).14
Silver diamine fluoride (SDF)—while not used as a preventive measure for dental caries—is an important new therapy in the treatment of cavitated lesions for pediatric and special-needs populations. SDF is commonly used to arrest dental caries in children and adults. The American Academy of Pediatric Dentistry (AAPD) released new guidelines in 2017 on the use of SDF for dental caries in children and adolescents.16 The guidelines support the use of 38% SDF to arrest cavitated caries lesions in primary dentition.16
ACUTE AND CHRONIC FLUORIDE TOXICITY
Fluoride toxicity can occur if recommended doses for fluoride additives are not followed. Acute fluoride toxicity is dependent on the dose-intake and a patient’s weight.17 While small ingestions of fluoride can cause gastrointestinal irritation, large amounts can lead to organ damage.18 The overconsumption of fluoride can also lead to fluorosis, skeletal fluorosis, and bony outgrowths.14,18
Elevated amounts of fluoride during enamel formation increase the risk of fluorosis. Repeated exposure of fluoride-concentrated foods and beverages early in a child’s life can increase this risk.4 Enamel defects are symptomatic of fluorosis and may present as white specks, striations, or rough pitted surfaces.4 Fluorosis can range from very mild to severe. Very mild fluorosis is often misdiagnosed because it can mimic other oral conditions such as tetracycline staining.4
FLUORIDE RECOMMENDATIONS
Based on evidence from clinical trials, meta-analyses, systematic reviews, and expert panels conducted by the AAPD, ADA, and USPSTF, the following recommendations can be made on the utilization of fluoride in preventing dental caries or minimizing dental caries risk among pediatric patients.10,19 Fluoride is both safe and highly effective in minimizing caries prevalence.10,19Professionally applied topical fluoride treatments at 5% sodium fluoride (NaF) varnish or 1.23% gel preparations are efficacious in reducing caries risk in children.10 Mouthrinse containing 0.2% NaF and 1.1% NaF gels and toothpastes are effective in reducing dental caries in children.10 There is a moderate net benefit in preventing future dental caries with oral fluoride supplements beginning at 6 months for children whose water supply is deficient in fluoride.19 There is a moderate net benefit of preventing dental caries when fluoride varnish is applied to children’s teeth beginning at the eruption of primary dentition. Thus, all children can benefit from fluoride varnish application regardless of dental caries risk. Fluoride varnish can be applied every 6 months among preschool aged children who are at moderate risk for dental caries.19 Moreover, children who are at moderate risk for dental caries should receive the application every 3 months to 6 months.20
COLLABORATIVE APPROACH
An interprofessional collaborative approach is needed in order to address factors associated with caries risk and implement preventive measures. Primary care providers (PCPs) see children and their parents/caregivers the most often through well-child visits, which focus on disease prevention and the patient’s development and growth.21 Thus, oral health assessments, anticipatory guidance, and fluoride varnish application should be part of these visits. In most states, PCPs can apply fluoride varnish.22,23However, barriers associated with performing oral health assessment include insufficient time to perform additional duties, lack of confidence in referring patients to local dentists, and inadequate training in oral health.24,25
Performing oral health assessments, applying fluoride varnish, and making proper referrals to oral health professionals are tasks PCPs must feel confident in initiating. The American Academy of Pediatrics has several oral health education training programs to assist in increasing confidence and competence among PCPs.26 While educating PCPs is important, teaching parents/caregivers on caries-preventive measures is also essential. Through interprofessional collaboration and education, a sound partnership and referral system can be established to improve access to care and minimize caries risk.
CONCLUSION
Both oral health and medical professionals should assess children’s caries risk and fluoride exposure at each preventive appointment. Clinicians should also educate parents/caregivers on the sources of fluoride through foods, oral health products, and professional applications. Through patient-centered interprofessional collaboration, children’s caries risk can be significantly reduced; thereby improving overall health and quality of life.
REFERENCES
- Centers for Disease Control and Prevention. Children’s Oral Health. Available at: cdc.gov/oralhealth/children_adults/child.htm. Accessed January 22, 2018.
- Kassebaum NJ, Bernabe E, Dahiya M, Bhandari B, Murray CJL, Marcenes W. Global burden of untreated caries: A systematic review and metaregression. J Dent Res. 2015;94:650–658.
- Dye BA, Thorton-Evans G, Li X, Lafolla T. Dental caries and sealant prevalence in children and adolescents in the United States, 2011-2012. NCHS Data Brief. 2015;191:1–8.
- Carey C. Focus on fluorides: update on the use of fluoride for the prevention of dental caries. J Evid Based Dent Pract. 2014;14(Suppl):95–102.
- US Department of Health and Human Services Federal Panel on Community Water Fluoridation. US public health service recommendation for fluoride concentration in drinking water for the prevention of dental caries. Public Health Rep. 2015;130: 318–331.
- United States Centers for Disease Control and Prevention. Community Water Fluoridation. Available at: cdc.gov/fluoridation/index.htm. Accessed January 22, 2018.
- Berg J, Gerweck C, Hujoel PP, et al. Evidence-based clinical recommendations regarding fluoride intake from reconstituted infant formula and enamel fluorosis: A report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2011;142:79–87.
- Martinez-Mier EA, Spencer KL, et al. Fluoride diet of 2- year-old children. Community Dent Oral Epidemiol. 2017;45:251–257.
- US Centers for Disease Control and Prevention. Brush Up on Healthy Teeth. (n.d). Available at cdc.gov/OralHealth/pdfs/BrushUpTips.pdf. Accessed January 22, 2018.
- American Academy of Pediatric Dentistry. Guideline on fluoride therapy. Pediatr Dent. 2013;35:E165–168.
- Weyant R, Tracy SL, Anselmo T, Beltran-Aguilar ED, Donly KJ, Frese W. Topical fluoride for caries prevention. J Am Dent Assoc. 2013;144:1279–1290.
- US Preventive Services Task Force. Grade Definition. Available at uspreventiveservicestaskforce.org/Page/Name/grade-definitions. Accessed January 22, 2018.
- Bonnetti D, Clarkson JE. Fluoride varnish for caries prevention: Efficacy and implementation. Caries Res. 2016;50(Suppl 1):45–49.
- Rozier RG, Adair S, Graham F, et al. Evidence-based clinical recommendations on the prescription of dietary fluoride supplements for caries prevention. J Amer Dent Assoc. 2010;141:1480–1489.
- Levy SM, Guha-Chowdury N. Total fluoride intake and implications for dietary supplementation. J Public Health Dent. 1999;59:211–223.
- American Dental Association. New Guidelines Address the Use of Silver Diamine Fluoride in Pediatric and Special-Needs Patients. Available at: ada.org/en/science-research/science-in-the-news/new-guideline-addresses-the-use-of-silver-diamine-fluoride-in-pediatric-and-special-needs-patients. Accessed January 22, 2018.
- Garcia RI, Gregorich SE, Ramos-Gomez F, et al. Absence of fluoride varnish-related adverse events in caries prevention trials in young children, United States. Prev Chronic Dis. 2017;14:E17.
- Shah S, Quek S, Ruck B. Analysis of phone calls regarding fluoride exposure made to New Jersey poison control center from 2010 to 2012. J Dent Hyg. 2016;90:35–45.
- Moyer V. Prevention of dental caries in children from birth through age 5 years: US Preventive Services Task Force recommendation statement. Pediatrics. 2014;133:1102–1111.
- American Dental Association Council on Scientific Affairs. Professionally applied topical fluoride: evidence-based clinical recommendations. J Am Dent Assoc. 2006;137:1151–1159.
- American Academy of Pediatrics. Recommendations for Preventive Pediatric Health Care. Available at: aap.org/enus/Documents/periodicity_ schedule.pdf. Accessed January 22, 2018.
- State Medicaid Payment for Caries Prevention Services by Nondental Professionals. Avaliable at: paconnect.wpengine.netdna-cdn.com/wp-content/uploads/2013/07/AAP-OHReimbursementChart-2.pdf. Accessed January 22, 2018.
- Virginia Oral Health Coalition. Important Update to Fluoride Varnish Billing Code For Medical Providers. Available at: vaoralhealth.org/ WHOWEARE/News/TabId/96/ArtMID/838/ArticleID/29/Important-Update-to-Fluoride-Varnish-Billing-Code-for-Medical-Providers.aspx. Accessed January 22, 2018.
- Hegner R. The interface between medicine and dentistry in meeting the oral health needs of young children: A white paper. Pediatr Dent. 2005;–130.
- Mitchell-Royston L, Nowak A. Interprofessional study of oral health in primary care. Available at: aapd.org/assets/1/7/Dentaquest_Year_1_ Final_Report.pdf. Accessed January 22, 2018.
- American Academy of Pediatrics. Oral Health Education and Training. Available at: aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Oral-Health/Pages/Education-and-Training.asp. Accessed January 22, 2018.
From Dimensions of Dental Hygiene. February 2018;16(2):30-33.


[…] is a valuable preventive measure in the fight against caries. Adjusting the fluoride concentration in public water to a safe and optimal level of 0.7 ppm is […]