 EDWARDOLIVE/ISTOCK/GETTY IMAGES PLUS
EDWARDOLIVE/ISTOCK/GETTY IMAGES PLUS
The Relationship Between Obesity and Periodontal Diseases
Identifying and addressing oral complications are essential to successful management of this chronic inflammatory autoimmune disease.
This course was published in the May 2018 issue and expires May 30, 2021. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Identify the prevalence of obesity in the United States.
- Explain obesity-related systemic effects that result in chronic inflammation.
- Discuss implications of obesity on the periodontium.
- Identify key components necessary for management of obese patients.
Obesity is defined as excessive body fat in relation to lean body mass, and contributing factors include a complex interaction of excess caloric consumption, unhealthy food choices, sedentary lifestyles, genetics, medications, and some diseases.1 Obesity is most commonly determined by body mass index (BMI), which is calculated by dividing an individual’s weight in kilograms (kg) by squaring of the height in meters (kg/m2).1 For adults, a calculated BMI ≥ 25kg/m2 is considered overweight; while a BMI ≥30 kg/m2 is considered obese.1 For children ages 5 to 19, overweight is defined as a BMI-for age greater than one standard deviation above the growth reference median, and childhood obesity is defined as more than two standard deviations above the median.1 Obesity is also be measured by waist circumference (WC). Men with a WC ≥ 102 cm and women with a WC ≥ 88 cm are considered obese.3 Waist circumference measurements and BMI calculations appear to be strongly correlated with an increased disease risk.4–6
Accumulated excessive fat associated with obesity contributes to serious health risks including chronic inflammatory diseases such as arthritis, diabetes, cardiovascular disease, and some cancers.7–9 Increasing concerns regarding obesity-related health implications include adverse consequences on oral health, in particular periodontitis, a disease caused from pathogenic bacteria and the host immune response. Up-to-date knowledge related to the potential association between obesity and periodontal diseases can better prepare oral health professionals to educate patients on oral and systemic implications associated with obesity, identify patients with increased risk of developing periodontal diseases, and recognize important treatment outcomes associated with obese patients.
THE ORAL-SYSTEMIC LINK
Numerous studies suggest obesity is a risk factor for periodontal diseases.3,5,7,8,10,11 A state of inflammation that results from obesity may increase host susceptibility to periodontal breakdown. While poorly understood, an imbalance between the host’s immune and inflammatory systems likely plays a significant role in both obesity and periodontitis.6,12 Several biological effects of obesity seem to relate to the pathogenesis of periodontitis. In particular, inflammatory cytokines—such as interleukins (IL) and tumor necrosis factor (TNF)—play a role in each disease.
Fat, or adipose tissue, is primarily responsible for regulating body energy, and, under normal conditions, maintains homeostasis of energy storage and exertion. Abnormal or excessive abdominal fat, called visceral adipose tissue, is more highly associated with adverse health conditions than excess subcutaneous fat, and it contributes to multiple medical conditions.5–7,13,14 Body-shape morphology, indicated by the location of visceral adipose fat deposition, has been identified as a contributor to adverse health conditions. Proportionally more visceral adipose tissue, evident in an apple-shaped body type, increases the risk of metabolic health conditions, unlike a pear-shaped body type evidenced by excess fat below the waist.15 Research on the obese gene revealed visceral adipose tissue—in addition to energy regulation—functions as a complex metabolic endocrine organ with a role in cytokine secretion.16 Research suggests a possible link between obesity and periodontitis related to alterations in the host immune and inflammatory systems associated with both diseases.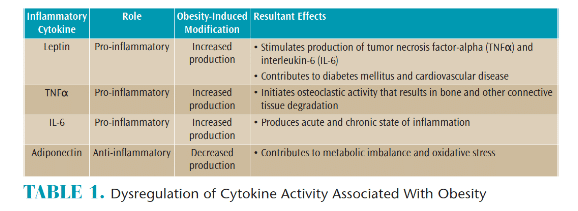
Adipocytes, found in visceral adipose tissue, contain activated macrophages that produce various cytokines.7,9,17–23 Excess visceral adipose tissue secretes bioactive peptides and can alter circulating signaling molecules called adipokines that are critical to endocrine function.24 As fat cells grow larger, recruitment of activated macrophages occurs, stimulating the production of pro-inflammatory mediators.7,9,17-23 Leptin, adiponectin, TNF-alpha (TNFα), and IL-6 are specialized cytokines, referred to as adipokines, that act as inflammatory mediators in communication with the immune system.22,23,25 Adipokines are categorized as either anti-inflammatory or pro-inflammatory according to their role (Table 1). Excessive visceral adipose tissue increases production of pro-inflammatory cytokines, leptin, TNFα, and IL-6, as well as reduces adiponectin, an anti-inflammatory cytokine. Hence, an exaggerated hyper-inflammatory reaction can be activated and may increase susceptibility to tissue breakdown, including tissues of the periodontium.7,21–24,26,27 Responsible for regulation of inflammation and immunity, an imbalance of cytokine activity can lead to chronic low-grade systemic inflammation and a modified metabolic and immune response influencing host susceptibility to disease (Figure 1).7,9,18–23 The resultant pro-inflammatory state may stimulate pro-inflammatory mediators and cytokines and contribute to periodontal diseases; the greater the amount of adipose tissue, the greater the production of inflammatory mediators.
Weisberg et al28 researched the expression of obesity-related macrophages and found a positive correlation between activated macrophages and body mass. Increased macrophage activity leads to increased cytokine secretion that generates an inflammatory response.29 Responsible for regulation of inflammation and immunity, research suggests an imbalance of cytokine activity can lead to chronic low-grade systemic inflammation and a modified metabolic and immune response influencing host susceptibility to disease.7,9,18–23
Recent research indicates obesity is significantly associated with modifications in pro- and anti-inflammatory cytokines that results in a hyper-inflammatory host response.30 High levels of leptin initiate macrophage activity that stimulates production of TNFα and IL-6, thus producing an inflammatory reaction.22,26 High levels of circulating leptin are associated with an increased production of C-reactive protein (CRP), a chronic inflammatory marker associated with multiple diseases, including diabetes mellitus and cardiovascular disease.23,27 Furthermore, increased leptin production contributes to metabolic changes associated with bone formation and destruction,27 influences oxidative stress, and affects host immunity.31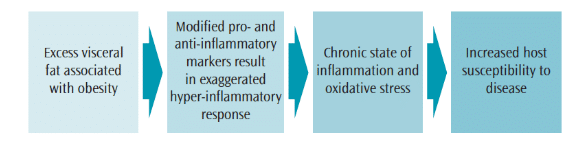
Associated with osteoclastic formation, increased TNFα can lead to the degradation of the connective tissue matrix, resulting in the breakdown of bone.7,22 Additionally, both TNFα and IL-6 are linked to the destruction of connective tissue and bone associated with periodontal breakdown. Furthermore, inflammatory marker modifications and overaccumulation of fatty acids in adipose tissue can increase the production of reactive oxygen species molecules that contribute to a chronic state of oxidative stress.10,32 Attributable to adverse metabolic conditions, oxidative damage is significantly greater in obese individuals than nonobese individuals.10,33 A state of oxidative stress associated with visceral obesity contributes to systemic inflammation and a modified immune response that results in host susceptibility to disease.
The state of inflammation resulting from dysregulation of cytokine activity and oxidative stress appears to play a role in the relationship of obesity as a risk factor for periodontal diseases (Table 2). The imbalance of anti-inflammatory and pro-inflammatory adipokines modulate the development and progression of periodontal diseases.18,19,22 Recent studies indicate the rate of developing periodontitis increases 1.8 times more in obese individuals, and those with a BMI > 30 were three times more likely to develop periodontitis.18,19
![Inflammatory Markers & Periodontal Dieases]() ORAL HEALTH CONCERNS
ORAL HEALTH CONCERNS
Understanding the link between obesity and periodontal diseases may contribute to improved patient care in the medical, dental, and scientific communities. The success of periodontal therapy may be modulated by the adverse effects of obesity on periodontal tissues.28,34,35 Higher levels of inflammatory markers such as leptin, TNFα, IL-6, and even CRP post-treatment, suggest obesity may inhibit positive long-term results. Obesity seems to complicate outcomes of periodontal treatment. A multidisciplinary approach between medical and oral health professionals may be needed to promote optimal health outcomes.
In a study to determine if significant weight loss would improve the response to nonsurgical periodontal therapy, obese individuals who underwent bariatric surgery achieved significant improvement after periodontal therapy compared with those who did not.36Additionally, obese individuals who received gastric bypass surgery (GBS) realized a reduction in periodontopathogenic bacteria and periodontal disease, as well as a reduction in some inflammatory biomarkers. However, the severity of periodontal disease increased, suggesting that GBS may decrease inflammatory biomarkers, but does not improve dysregulation of the immune system.37
It appears that adverse conditions associated with obesity and periodontal diseases are evident. As such, oral pathogens and systemic inflammatory markers should be controlled via nonsurgical treatment to reduce the risk of periodontal diseases. In addition, oral health professionals should promote a healthy lifestyle that includes weight control, dietary counseling, and oral biofilm control. Dental hygienists are well suited to recognize and inform patients of health risks associated with obesity with recommendations for good nutrition and exercise.
Weight control education may focus on teaching empathy, patient motivation skills, specialized levels of care associated with the “5 A’s” intervention steps (Ask, Advise, Assess, Assist, and Arrange), and professional intercollaboration. The ability to initiate an open dialogue with patients regarding the latest research on obesity-related health concerns can facilitate awareness for health promotion and disease prevention. In treating obese periodontal patients, dental hygienists should consider more frequent patient recare appointments and early treatment of disease, including the use of adjunctive therapies, such as antimicrobials, to decrease the host inflammatory burden. In addition, individualized behavioral and dietary counseling should be included in treatment planning for obese patients and those at-risk of obesity. Dental hygienists should closely monitor the periodontal health of obese patients and perform continuous assessment, education, and dietary counseling and encourage lifestyle changes promoting a healthy diet and weight loss. The US Department of Agriculture’s Dietary Guidelines for Americans 2015-2020 provides an excellent overview of healthy eating recommendations via MY Plate and the Dietary Guidelines for Life.38 Excellent suggestions for physical activity are found at: health.gov/paguidelines.
Continuing education courses are needed to promote awareness of oral and systemic implications associated with obesity, reduce assessment and treatment plan barriers, and improve practitioner confidence when approaching obesity-related health topics. Increased knowledge of appropriate caloric intake and physical activity for weight loss and sustainability, combined with skill development in behavior modifications may promote dental hygienists’ role in facilitating positive lifestyle changes for patients. Interprofessional collaboration is important. As part of a multidisciplinary approach to improve health outcomes, dental hygienists are in an ideal position to facilitate prevention and intervention efforts and referrals to other health care professionals.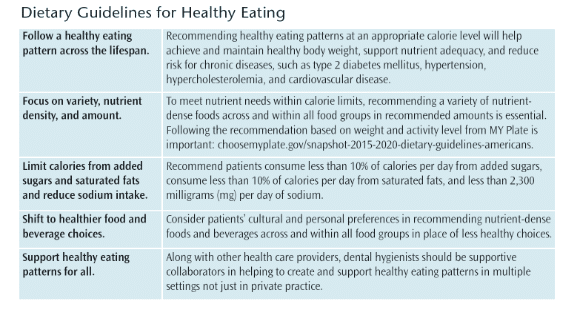
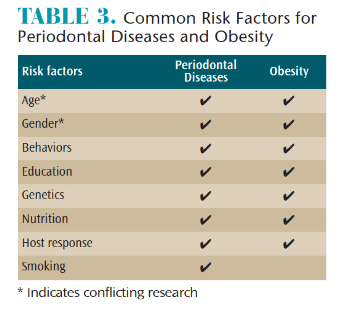
In recognition of periodontal implications associated with obesity, dental hygienists should integrate practice modifications based on the latest research. Specifically, dental hygienists can include BMI and waist-to-height ratio calculations as part of the patient assessment in coordination with evaluating medical history risk factors (Table 3). Such information will enable clinicians to identify additional risks associated periodontal diseases. The ability to initiate an open dialogue with patients regarding the latest research on obesity-related health concerns can facilitate awareness for health promotion and disease prevention.
Identification of patients’ needs are a significant component of the American Dental Hygienists’ Association (ADHA) dental hygiene clinical practice guidelines and important in promoting patient-centered care and interprofessional collaboration.39 Therefore, dental hygienists should be competent in the management of patients with obesity and be able to convey current research on the link between periodontitis, obesity, and systemic health. To maintain better control over their periodontal inflammation, obese patients should be referred to health care professionals and weight loss centers for weight reduction interventions. Moreover, with expansion of interprofessional care models, future dental hygiene obesity specialists could potentially be employed in weight loss centers as an integral part of weight loss management teams to promote overall health and wellness.
Dental hygienists need to understand that obesity predisposes patients to periodontal diseases. Learning to communicate effectively with obese patients about their disease risk may facilitate improved oral and systemic health.
REFERENCES
- World Health Organization. Obesity and Overweight. Available at: who.int/mediacentre/factsheets/fs311/en/. Accessed April 14, 2018.
- Hales C, Carroll M, Fryar C, Ogden C. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Brief. 2017;288:1–8.
- Dahiya P, Kamal R, Gupta R. Obesity, periodontal and general health: relationship and management. Indian J Endocrinol Metab. 2012;16:88–93.
- Dittmann C, Doueiri S, Kluge R, Dommisch H, Gaber T, Pischon N. Porphyromonas gingivalis suppresses differentiation and increases apoptosis of osteoblasts from New Zealand obese mice. J Periodontol. 2015;86:1095–1102.
- Ritchie C. Obesity and periodontal disease. Periodontol 2000. 2007;44:154–163.
- Kangas S, Timonen P, Knuuttila M, Jula A, Ylostalo P, Syrjala AH. Waist circumference and waist-to-height ratio are associated with periodontal pocketing-results of the Health 2000 Survey. BMC Oral Health. 2017;17:1–7.
- Keller A, Rohde J, Raymond K, Heitmann B. Association between periodontal disease and overweight and obesity: a systematic review. J Periodontol. 2015;86:766–776.
- Suresh S, Mahendra J, Sudhakar U, Pradeep AR, Singh G. Evaluation of plasma reactive oxygen metabolites levels in obese subjects with periodontal disease. Indian J Dent Res. 2016;27:155–159.
- Nascimento GG, Leite FR, Do LG, et al. Is weight gain associated with the incidence of periodontitis? A systematic review and meta-analysis. J Clin Periodontol. 2015;42:495–505.
- Atabay VE, Lutfioglu M, Avci B, Sakallioglu EE, Aydogdu A. Obesity and oxidative stress in patients with different periodontal status: a case-control study. J Periodontal Res. 2017;52:51–60.
- Singh M, Chopra R, Bansal P, Dhuria S. Association between obesity and periodontitis—a clinical and biochemical study. Indian J Dent Sci. 2013;2:6–8.
- Pischon N, Heng J, Bernimoulin B, Willich S, Pischon T. Obesity, inflammation, and periodontal disease. J Dent Res. 2007;86:400–409.
- Maciel SS, Feres M, Goncalves TE, et al. Does obesity influence the subgingival microbiota composition in periodontal health and disease? J Clin Periodontol. 2016;43:1003–1012.
- Gorman A, Kaye EK, Apovian C, Fung TT, Nunn M, Garcia RI. Overweight and obesity predict time to periodontal disease progression in men. J Clin Periodontol. 2012;39:107–114.
- Shearer ES. Obesity anaesthesia: the dangers of being an apple. Br J Anaesth. 2013;110:172–174.
- Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman J. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–431.
- Wang Z, Nakayama T. Inflammation, a link between obesity and cardiovascular disease. Mediators Inflamm. 2010;2010:1–17.
- Khader YS, Bawadi HA, Haroun TF, Alomari M, Tayyem RF. The association between periodontal disease and obesity among adults in Jordan. J Clin Periodontol. 2009;36:18–24.
- Shah M, Rehan A, Zakir S. Effect of obesity on periodontal disease. Pakistan Oral Dent J. 2015;35:628–630.
- Suvan JE, Petrie A, Nibali L, et al. Association between overweight/obesity and increased risk of periodontitis. J Clin Periodontol. June 9, 2015. Epub ahead of print.
- Nascimento GG, Peres KG, Mittinty MN, et al. Obesity and periodontal outcomes: a population-based cohort study in Brazil. J Periodontol. 2017;88:50–58.
- Zimmermann GS, Bastos MF, Dias Goncalves TE, Chambrone L, Duarte PM. Local and circulating levels of adipocytokines in obese and normal weight individuals with chronic periodontitis. J Periodontol. 2013;84:624–633.
- Buduneli N, Biyikoglu B, Ilgenli T, et a.. Is obesity a possible modifier of periodontal disease as a chronic inflammatory process? A case-control study. J Periodontal Res. 2014;49:465–471.
- Kwon H, Pessin JE. Adipokines mediate inflammation and insulin resistance. Front Endocrinol. 2013;4:71.
- Trayhurn P, Wood I. Signaling role of adipose tissue adipokines and inflammation in obesity. Biochem Soc Trans. 2005;33:1078–1081.
- Goncalves TE, Zimmermann GS, Figueiredo LC, et al. Local and serum levels of adipokines in patients with obesity after periodontal therapy: one-year follow-up. J Clin Periodontol. 2015;42:431–439.
- Jain H, Mulay S. Relationship between periodontitis and systemic diseases: leptin, a new biomarker? Indian J Dent Res. 2014;25:657–661.
- Weisberg S, McCann D, Desai M, Rosenbaum M, Leibel R, Ferrante A. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003;112:1796–1808.
- Makki K, Froguel P, Wolowczuk I. Adipose tissue in obesity-related inflammation and insulin resistance: cells, cytokines, and chemokines. ISRN Inflamm. 2013;2013:1–12.
- Schmidt FM, Weschenfelder J, Sander C, et al. Inflammatory cytokines in general and central obesity and modulating effects of physical activity. PLoS One. 2015;10:1–17.
- Bullon P, Morillo JM, Ramirez-Tortosa MC, Quiles JL, Newman HN, Battino M. Metabolic syndrome and periodontitis: is oxidative stress a common link? J Dent Res. 2009;88:503–518.
- Levine RS. Obesity, diabetes and periodontitis—a triangular relationship? Br Dent J. 2013;215:35–9.
- Dandona P, Mohanty P, Ghanim H, et al. The suppressive effect of dietary restriction and weight loss in the obese on the generation of reactive oxygen species by leukocytes, lipid peroxidation, and protein carbonylation. J Clin Endocrinol Metab. 2001;86:355–362.
- Nascimento GG, Leite FR, Correa MB, Peres MA, Demarco FF. Does periodontal treatment have an effect on clinical and immunological parameters of periodontal disease in obese subjects? A systematic review and meta-analysis. Clin Oral Investig. 2016;20:639–647.
- Suvan J, Petrie A, Moles DR, et al. Body mass index as a predictive factor of periodontal therapy outcomes. J Dent Res. 2014;93:49–54.
- Lakkis D, Bissada NF, Saber A, et al. Response to periodontal therapy in patients who had weight loss after bariatric surgery and obese counterparts: a pilot study. J Periodontol. 2012;83:684–689.
- Sales-Peres SH, de Moura-Grec PG, Yamashita JM, et al. Periodontal status and pathogenic bacteria after gastric bypass: a cohort study. J Clin Periodontol. 2015;42:530–36.
- United States Department of Agriculture. Dietary Guidelines for Americans 2015-2020. Available at: choosemyplate.gov/dietary-guidelines. Accessed April 14, 2018.
- American Dental Hygienists’ Association. ADHA Standards for Clinical Practice. Available at: adha.org/resources-docs/2016-Revised-Standards-for-Clinical-Dental-Hygiene-Practice.pdf. Accessed April 14, 2018.
From Dimensions of Dental Hygiene. May 2018;16(5):54-57.


 ORAL HEALTH CONCERNS
ORAL HEALTH CONCERNS
