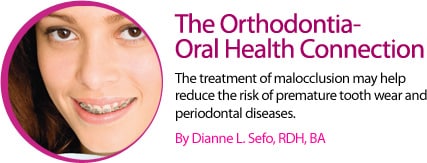
The Orthodontia-Oral Health Connection
The treatment of malocclusion may help reduce the risk of premature tooth wear and periodontal diseases.
Orthodontic treatment has long been used to create esthetic smiles and improve function. But could orthodontia also provide underlying oral health benefits? Evidence suggests that uneven occlusal forces may increase the risk of premature tooth wear and periodontal diseases. Although more research is necessary to answer this question, it is biologically plausible that aligning maloccluded teeth could address the root of some of today’s most common dental problems, including occlusal trauma, tooth wear, noncarious lesions, and periodontitis.
ORAL HEALTH PROBLEMS RELATED TO MALOCCLUSION
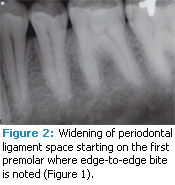
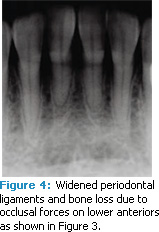
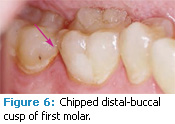
Occlusal trauma. An injury to the contact surfaces of opposing teeth, occlusal trauma leads to tissue changes within the attachment apparatus (tissues that support the teeth’s function) due to the pressure of occlusal forces. Any tooth that has premature, lateral, balance, or protrusive contact is more likely to experience occlusal trauma.1,2 Clinical symptoms include tooth pain, mobility, and widening of periodontal ligament spaces that can be viewed radiographically (Figure 1 to Figure 4). Excessive occlusal forces can injure the attachment apparatus and affect the temporomandibular joint, mastication muscles, pulp tissue, and integrity of tooth structure and restorations. Tooth wear. Patients may see or feel changes in tooth anatomy when a tooth is cracked or fractured (Figure 5 and Figure 6). Symptoms include sensitivity to pressure, cold, and/or sweets. The etiology of these cracks/fractures is multifactorial. Ratcliff et al suggest that excursive forces initiate cracks in teeth, which increase in the presence of parafunction.2 They found that stained or symptomatic cracks were age-related—demonstrating that the process is chronic. Staufer et al found a correlation between an increase in tooth fractures and lower anterior crowding (Figure 7). They concluded that an even occlusion, which eliminates interferences, may decrease the risk of cracks or fractures.3
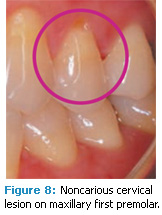
Noncarious lesions. It has been suggested that occlusal interferences may cause the development of noncarious cervical lesions or abfractions (Figure 8), although scientific evidence of this effect is lacking. When occlusal loading forces are placed on the long axis of the tooth, the forces are scattered, which results in minimal stress on the dentin or enamel. When the forces are lateral, the stress is concentrated in the cervical area. Chemical bonds of the enamel and dentin crystalline structures break, and tooth structure is lost due to acid exposure and abrasions.4–9 Redirecting the lateral forces to the long axis of the tooth may alleviate the stress along the cervical area. Studies evaluating the incidence and prevalence of abfractions are limited, however, it is possible that occlusal trauma is related to the morphology and location of these lesions.10–12
 |
 |
 |
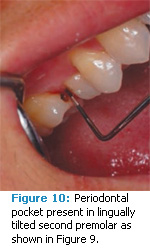
Periodontitis. Glickman first introduced the concept of occlusal trauma accelerating the progression of periodontal diseases in 1963.13 He proposed that although excessive occlusal forces do not cause inflammation, they do alter the pathway of inflammation. Glickman suggested that these forces, together with plaque-induced inflammation, act as co-destructive forces, resulting in an alteration of the normal pathway of inflammation and the formation of angular bone defects and infrabony pockets (Figure 9 and Figure 10). Additional studies demonstrated that as occlusal forces increased, so did pocket depths among patients with established periodontitis.1,14,15 On the other hand, Shefter et al’s study of patients with mild to moderate periodontitis did not find a relationship between pocket depths and occlusal forces.7 The interrelationship between occlusal trauma and periodontal inflammation remains controversial due to conflicting study results. These results may be due to differences in the species of animal used in the research, the methods used to produce occlusal trauma, and inherent inaccuracies in measurement.
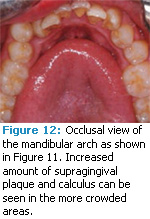
Evidence establishing a relationship between crowding and periodontal conditions has also been contradictory. Studies have reported results that range from no relationship to weak or limited relationships.3,17–20 Staufer et al found no correlation between deep periodontal pockets and the presence of crowding.3 The same study did link gingivitis and gingival recession to the degree of crowding present. Crowding in relation to other factors associated with the progression of periodontal diseases, such as oral hygiene, has been evaluated and also demonstrated inconsistent results. Some studies have showed the relationship is weak, while others have noted that supragingival plaque accumulation in crowded areas is significantly greater than in noncrowded areas (Figure 11 and Figure 12).21,22 Periodontal pathogens, such as Fusobacterium, Capnocytophaga, Campylobacter rectus, and Peptostreptococcus micros, were also present in larger numbers in crowded areas vs noncrowded areas. One possible conclusion is that oral health is more easily maintained in a noncrowded dentition.23
 |
 |
 |
Orthodontics used for molar uprighting may aid in the elimination of vertical bone defects on the mesial surfaces of molars that have tipped into edentulous spaces, although studies have not found any differences in alveolar bone and gingival inflammation between tipped and upright molars.24,25 On the other hand, Kraal et al did find that pocket depths in mesial to uprighted molars were more shallow than control teeth.25
 |
 |
 |
RESEARCH REVIEW
A systemic review on existing studies evaluating orthodontic treatment and periodontal outcomes has identified an absence of reliable evidence.26 The studies reviewed had potential for bias and were flawed. In some, no evaluations were taken at baseline or no follow-up of factors, such as oral hygiene regimen, socioeconomic status, or smoking, was provided. Other issues included lack of information on pretreatment periodontal status, reporting the number of subjects lost to follow-up, and missing data. Many participants were adolescents or young adults. Often, untreated controls had slight malocclusion. Very few studies included current orthodontic expansion methods. More epidemiologic studies with adequate comparison groups, specific techniques, and substantial follow-up are needed to fully understand the impact of orthodontic treatment on oral health.
 |
 |
 |
CONCLUSION
Although the concept of improving oral health by treating malocclusion is not scientifically proven, there is evidence that forces created by malocclusion increase the risk of premature tooth wear and periodontal diseases. Correcting malocclusion to improve oral health is supported by the American Dental Association and the American Association of Orthodontics, and can be found in educational literature available to the public.27,28 It is the dental team’s responsibility to ensure that patients are educated about the possible risks of malocclusion and all available treatment options.
PHOTO CREDITS:
FIGURE 1 THROUGH FIGURE 6 COURTESY OF KATHRINA AGATEP, DDS, DENTAL DESIGNS SD, SAN DIEGO
FIGURE 7 THROUGH FIGURE 12 COURTESY OF KATHRINA AGATEP, DDS, DENTAL DESIGNS SD, SAN DIEGO
REFERENCES
- Harrel SK, Nunn ME. The effect of occlusal discrepancies on periodontitis. II. Relationship of occlusal treatment to the progression of periodontal disease. J Periodontol. 2001;72: 495–505.
- Ratcliff S, Becker IM, Quinn L. Type and incidence of cracks in posterior teeth. J Prosthet Dent. 2001; 86:167–172.
- Staufer K, Landmesser H. Effects of crowding in the lower anterior segment—a risk evaluation depending upon the degree of crowding. J Orafac Orthop. 2004;65:13–25.
- Pegoraro LF, Scolaro JM, Conti PC, Telles D, Pegoraro TA. Noncarious cervical lesions in adults: prevalence and occlusal aspects. J Am Dent Assoc. 2005;136:1694–1700.
- Lee WC, Eakle WS. Possible role of tensile stress in the etiology of cervical erosive lesions of teeth. J Prosthet Dent. 1984;52:374–380.
- Grippo JO, Simring M. Dental erosion revisited. J Am Dent Assoc. 1995; 126: 619–620, 623–624, 627–630.
- Shefter GJ, McFall WT Jr. Occlusal relations and periodontal status in human adults. J Periodontol. 1984;55:368–374.
- Grippo JO, Simring M, Schreiner S. Attrition, abrasion, corrosion and abfraction revisited: a new perspective on tooth surface lesions. J Am Dent Assoc. 2004;135:1109–1118.
- Francisconi LF, Graeff MS, Martins Lde M, et al. The effects of occlusal loading on the margins of cervical restorations. J Am Dent Assoc. 2009; 140: 1275–1282.
- Aw TC, Lepe X, Johnson GH, Mancl L. Characteristics of noncarious cervical lesions: a clinical investigation. J Am Dent Assoc. 2002; 133:725–733.
- Lee WC, Eakle WS. Stress-induced cervical lesions: review of advances in the past 10 years. J Prosthet Dent. 1996;75:487–494.
- Litonjua LA, Andreana S, Bush PJ, Tobias TS, Cohen RE. Noncarious cervical lesions and abfractions: a reevaluation. J Am Dent Assoc. 2003;134:845–850.
- Glickman I. Inflammation and trauma from occlusion: Codestructive factors in chronic periodontal disease. J Periodontol. 1963;34:5–10.
- Burgett FG, Ramfjord SP, Nissle RR, Morrison EC, Charbeneau TD, Caffesse RG. A randomized trial of occlusal adjustment in the treatment of periodontitis patients. J Clin Periodontol. 1992;19:381–387.
- Nunn ME, Harrel SK. The effect of occlusal discrepancies on periodontitis. I. Relationship of initial occlusal discrepancies to initial clinical parameters. J Periodontol. 2001;72:485–494.
- Shefter GJ, McFall WT Jr. Occlusal relations and periodontal status in human adults. J Periodontol. 1984; 55:368–374.
- Onyeaso CO, Arowojolu MO, Taiwo JO. Periodontal status of orthodontic patients and the relationship between dental aesthetic index and community periodontal index of treatment need. Am J Orthod Dentofacial Orthop. 2003;124:714–720.
- Helm S, Kreiborg S, Solow B. Malocclusion at adolescence related to self-reported tooth loss and functional disorders in adulthood. Am J Orthod. 1984;85:393–400.
- Ngom PI, Diagne F, Benoist HM, Thiam F. Intraarch and interarch relationships of the anterior teeth and periodontal conditions. Angle Orthod. 2006;76:236–242.
- Helm S, Petersen PE. Casual relation between malocclusion and periodontal health. Acta Odontol Scand. 1989;47:223–228.
- Onyeaso CO, Arowojolu MO, Taiwo JO. Oral hygiene status and occlusal characteristics of orthodontic patients at University College Hospital, Ibadan, Nigeria. Odontostomatol Trop. 2003;26:24–28.
- Artun J, Osterberg SK. Periodontal status of secondary crowded mandibular incisors. Long-term results after orthodontic treatment. J Clin Periodontol. 1987;14:261–266.
- Chung CH, Vanarsdall RL, Cavalcanti EA, Baldinger JS, Lai CH. Comparison of microbial composition in the subgingival plaque of adult crowded versus non-crowded dental regions. Int J Adult Orthodon Orthognath Surg. 2000; 15: 321–330.
- Lundgren D, Kurol J, Thorstensson B, Hugoson A. Periodontal condition around tipped and upright molars in adults. An intra-individual retrospective study. Eur J Orthod. 1992;14:449–455.
- Kraal JH, Digiancinto JJ, Dail RA, Lemmer man K, Peden JW. Periodontal conditions in patients after molar uprighting. J Prosthet Dent. 1980;43:156–162.
- Bollen AM, Cunha-Cruz J, Bakko DW, Huang GJ, Hujoel PP. The effects of orthodontic therapy on periodontal health: a systematic review of controlled evidence. J Am Dent Assoc. 2008;139:413–422.
- American Dental Association. For the dental patient. Braces: straighter teeth can improve oral health. J Am Dent Assoc. 2007; 138:556.
- American Association of Orhtodontists. Want a beautiful smile? Available at: www.webcitation.org/5RDWqElut. Accessed March 8, 2012.
From Dimensions of Dental Hygiene. April 2012; 10(4): 34, 37-38.

