The First Line of Defense
Dental hygienists play an important role in recognizing the signs of antiresorptive agent-induced osteonecrosis of the jaw.
This course was published in the March 2013 issue and expires March 2016. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the indications for bisphosphonates and how they work.
- Identify the risk factors of antiresorptive agent-induced osteonecrosis of the jaw (ARONJ).
- Explain treatment and management strategies for ARONJ.
Bisphosphonates are anti resorptive medications prescribed to prevent and/or treat bone diseases. While they are designed to improve quality of life and increase longevity, these medications may also cause undesirable side effects. A small percentage of patients experience antiresorptive agent-induced osteonecrosis of the jaw (ARONJ) either while taking antiresorptive medications or several years post-therapy. As the median age of the American population continues to increase, the number of dental patients taking antiresorptive medications will probably increase, as well. As such, dental hygienists need to be well versed in the signs and symptoms of this serious complication.
BISPHOSPHONATES
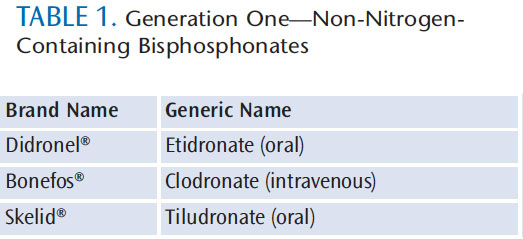
Bisphosphonates are a class of drugs given orally or parenterally to patients with bone loss. The majority of patients treated for osteoporosis receive the drugs orally. As a group, these drugs have a phosphorus-carbon-phosphorus backbone, and work by decreasing the number of osteoclasts.1,2 Two generations of bisphosphonate medications therefore exist: generation one contains no nitrogen and generation two contains nitrogen (Table 1 and Table 2). The structure and function of varying bisphosphonates are modified by side chains of R1 and R2, with the R2 side chain determining the antiresorptive potency. The R2 side chain containing nitrogen is the most potent and is most often associated with complications. Nitrogen side chains increase the binding affinity of the bisphosphonate to hydroxyapatite crystals and decrease bone resorption. As such, generation two bisphosphonates last the longest and are the most potent.2 Parenteral bisphosphonates have a longer duration of action and are more intense than those administered orally.
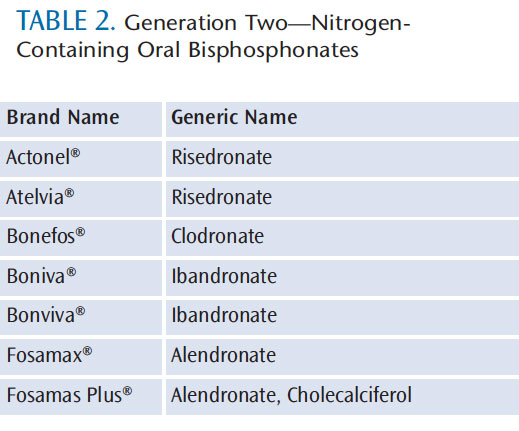
Bisphosphonate medications containing nitrogen have been associated with ARONJ more than any other antiresorptive therapy. While rare, ARONJ, or bone death, is a debilitating side effect. The current consensus, however, is that the benefits gained from preventing skeletal fractures outweigh the risks of ARONJ.1,3–5
OSTEONECROSIS
Osteonecrosis can occur in the hip, arm, knee, talus, shoulder, and jaw.6,7 It is unclear why osteonecrosis occurs, but it may be a natural consequence of local or systemic factors that impair blood flow.7,8 The American Association of Oral and Maxillofacial Surgeons (AAOMS) asserts that three characteristics must be present to meet the definition of ARONJ: current or previous treatment with a bisphosphonate, exposed bone in the maxillofacial region that has persisted for more than 8 weeks, and no history of radiation therapy to the jaw.6
Limited evidence is available on the risk factors related to ARONJ,9 but bisphosphonate potency, length of use, and the performance of invasive dentoalveolar surgery all seem to be related.6,9 Risk also increases if oral surgery has been or needs to be performed during antiresorptive treatment or after bisphosphonate therapy has been discontinued.
Periapical surgery that causes osseous injury increases risk, although there is much debate about whether dental implant therapy increases the likelihood of ARONJ.6,7,9 Studies also suggest that concomitant diseases, such as periodontitis and advanced caries, may increase the risk of developing ARONJ.4,6,9,10 While poor oral hygiene may not be a specific risk factor, the distinct microflora of the oral cavity may initiate or cause progression of ARONJ.11,12, Xerostomia is also related because salivary hypofunction increases the risk of caries and ulcerations.4 Bony protuberances (eg,mandibular and palatal tori) in the oral cavity are also associated with ARONJ because these osseous areas are covered with very thin mucosa, which is easily susceptible to damage from oral trauma.4–6 Patients with ill-fitting dentures that cause continuous tissue injury are also more likely to develop ARONJ.3,4,6 Advanced age may be related, although cancer and osteoporosis are more common among older adults and most of the studies were conducted on this population, so it is unclear what role age plays.
SIGNS AND SYMPTOMS
Because few treatments are available for ARONJ, prevention is the best approach. Prevention starts with an accurate, current medical history containing a list of all medications being taken. For patients taking bisphosphonates, the dosage, frequency, and duration should be obtained because each can influence the risk of developing ARONJ.
Recording patients’ past usage is also important due to the drug’s long half-life.2,13 Patients should also be queried about past or present treatment for any other bone diseases. Patients should then be educated about the risks and benefits of dental care while taking bisphosphonates, beginning signs and symptoms of ARONJ, and the importance of early treatment. Oral care providers must be proficient in identifying the clinical signs of ARONJ. Asymptomatic signs may be present for weeks or months before ARONJ is diagnosed.5 Dental professionals should look for exposed bone on the maxilla or mandible during the intraoral examination. The most common site of ARONJ is the mandibular posterior lingual region close to the mylohyoid ridge, although the alveolar ridge of the maxilla may also be affected.4–6,13,14
Other signs may include sequestra of bone or secondary infection with or without purulent drainage. If the patient has removable oral prosthetics, dental professionals must assess areas where the appliance comes in contact with tissue, specifically the lingual flange.3,6 Removable appliances may cause trauma to underlying tissues and adjacent mucosa, thus increasing the risk of developing ARONJ.3,6,15
As ARONJ progresses, exposed bone with smooth or ragged borders becomes clinically apparent.1,14 Bone lesions vary in color from yellow to grayish-tan and often present with fragmented friable soft tissue. With progression, pain may increase due to inflammation and secondary infection.13,16 More specific signs may include pathologic fracture, orocutaneous fistula, oroantral fistula, or oronasal fistula formation.13 When performing the extraoral exam, dental hygienists should look for an extraoral fistula from infected bone, which strongly indicates progression of ARONJ. Soft tissue ulcerations, swelling, paresthesia, suppuration, involvement with intraorextraoral sinus tracks, tooth mobility, and extraoral fistulae may also occur.1,14
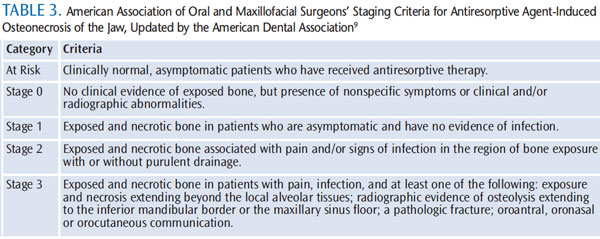
Radiographs may help determine oral involvement.17 Dental hygienists must be diligent in decreasing trauma to areas, such as exostoses and tori, when exposing radiographs because these minor traumas may result in poor healing among patients susceptible to ARONJ. While radiographs are helpful, early ARONJ may not appear on dental X-rays, computed tomography (CT), or magnetic resonance imaging. Dental professionals should be familiar with the AAOMS’ staging criteria to better assist in identifying ARONJ cases (Table 3).9
DIFFERENTIAL DIAGNOSIS
Eliminating conditions that may be similar to ARONJ, including aphthous ulcers, gingivitis, periodontal diseases, alveolar osteitis, caries, osteomyelitis or malignancies, sinusitis, temporomandibular disorders (TMDs), and osteoradionecrosis, assists in treatment planning.6,3,7 With proper oral hygiene, conditions, such as ulcers, gingivitis, and alveolar osteitis, may heal within a short time, while ARONJ usually will not.5 Caries may be assessed by radiographs, and if lesions are not advanced into the alveolar bone, then restorative treatment may be completed.6,9
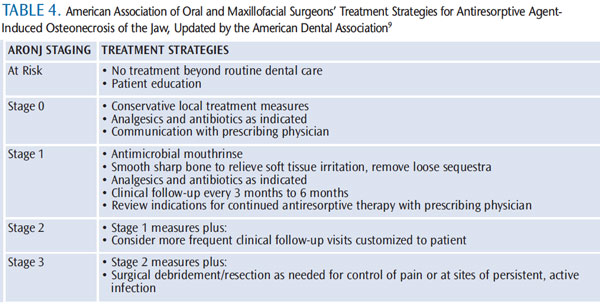
Osteomyelitis and other malignancies can be ruled out by a physician who can review CT cans and bone biopsies.7,13 Osteoradionecrosis of the jaw may appear similar to ARONJ. Dental professionals should contact the oncologist of patients who have received head and neck radiation to help definitively diagnose osteoradionecrosis.18 ARONJ is best diagnosed using the AAOMS’ criteria in the presence of exposed jaw, a history of bisphosphonate use, and no prior exposure to radiation of the head and neck (Table 4).9
TREATMENT
The goal of treating patients with ARONJ is to increase quality of life, control pain, manage secondary infections, and decrease the progression of necrosis.9,19 Ideally, all restorative, preventive, and periodontal therapy should be completed prior to the start of a bisphosphonate regimen.6 Specifically, scaling and root planing and other treatments for periodontal diseases should be done. Vescovi and Nammour recommend regular dental maintenance appointments at 4 months for cancer patients taking bisphosphonate medications and 8 months for noncancer patients, because spontaneous forms of ARONJ may develop. However, 3-month to 4-month maintenance appointments for scaling and root planing and review of self-care strategies may prove beneficial for controlling biofilm and oral infection.19
Once bisphosphonate therapy begins, patients should be managed with less invasive dental treatments.6,9 For example, scaling and root planing and minor restorations may be acceptable, but extractions are contraindicated due to potential exposure of the alveolar bone.5,6,9 If possible, questionable teeth should be treated endodontically, rather than through extraction, to avoid exposing the alveolar bone. When antiresorptive therapy has been completed, the dental team needs to remember that bisphosphonates have a long half-life and they could affect future treatment.13 Although surgical therapy carries a slight risk of ARONJ, there is no oral or periodontal surgical procedure, including implant placement, strictly contraindicated. However, the American Dental Association recommends that treatment plans should minimize periosteal and/or intrabony exposure or disruption.9
Maintaining optimal oral hygiene and keeping regular and frequent maintenance appointments are key strategies in preventing ARONJ.3,17,19 Therapeutic preventive maintenance procedures are important in reducing the bacterial load and minimizing oral infection. Patients must understand the importance of meticulous oral hygiene and its role in reducing oral infection and the risk of ARONJ. Dental hygienists need to educate patients about daily biofilm removal techniques and suggest alternative strategies if dexterity issues preclude optimal self-care. Antimicrobial mouthrinses, powered toothbrushes and flossers, and water irrigators may assist patients improve their oral health care regimens.
Control of dental caries is critical to preventing periapical infections, which can increase susceptibility to ARONJ. Regular use of caries preventive agents are valuable.9 Recommending tobacco cessation therapies to patients who smoke, as well as counseling patients to limit alcohol consumption, may lower the risk of developing ARONJ.19 When xerostomia is present, strategies for managing this condition should also be discussed. Because oral trauma is a risk factor for patients predisposed to ARONJ, individuals with removable prosthetic appliances should have them evaluated during each maintenance appointment for proper fit and to review daily oral care instructions. The importance of leaving the appliance out for at least 6 hours per day should also be emphasized. Frequent recare appointments enable dental hygienists to control oral deposits and apply professional products, such as fluoride varnish to decrease caries, as well as to closely monitor removable appliances.
Dental hygienists should be aware of any current dental treatment the patient is receiving from the dentist and look for signs of healing. Since extraction sites normally mucosalize within 14 days to 21 days, the dentist should be notified if healing has arrested.1,6,17 Dental hygienists should immediately report suspicious conditions and pathology to the dentist and encourage the patient to report uncomfortable areas exhibiting pain, swelling, or exposed bone.3,5,6,9,17
CONCLUSION
Dental professionals need to stay current on ARONJ as the literature is still evolving on its risk factors and management. The treatment and prevention of ARONJ is not well-defined yet. Hopefully, ongoing and future research will provide more clarity on this serious condition.
REFERENCES
- Watts NB, Diab DL. Long-term use ofbisphosphonates in osteoporosis. J Clin Endocrinol Metab. 2010;95:1555–1565.
- Graham R, Russell G. Determinants ofstructure-function relationships among bisphosphonates. Bone. 2007;40(Suppl):S21–S25.
- Shehabi Z. Managing the oral effects of bisphosphonate therapy. Dental Nursing.2011;7(5):258–261.
- Koka S, Clarke BL, Amin S, Gertz M, RuggieroSL. Oral bisphosphonate therapy and osteonecrosis of the jaw: what to tell the concerned patient. Int J of Prosthodont.2007;20:115–122.
- Rizzolo D, Sedrak M. Managing the adverse effects of bisphosphonate therapy on the jaw.JAAPA. 2009;22:48–52.
- Ruggiero SL, Dodson TB, Assael LA, et al. American Association of Oral and MaxillofacialSurgeons position paper on bisphosphonate related osteonecrosis of the jaw—2009 update. Aust Endod J. 2009;35:119–130.
- National Institute of Arthritis andMusculoskeletal and Skin Diseases. Questions and Answers about Osteonecrosis (AvascularNecrosis). Available at: www.niams.nih.gov/Health_Info/Osteonecrosis/default.asp. Accessed February 1, 2013.
- Vescovi P, Manfredi M, Merigo E, et al. Surgical approach with Er:YAG laser on osteonecrosis ofthe jaws (ONJ) in patients under bisphosphonate therapy (BPT). Lasers Med Sci. 2010;25:101–113.
- Hellstein JW, Adler RA, Edwards B, et al.American Dental Association Council on ScientificAffairs Expert Panel on Antiresorptive Agents.Managing the care of patients receiving antiresorptive therapy for prevention and treatment of osteoporosis: executive summary of recommendations from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2011;142:1243–1251.
- Palomo L, Bissada N, Liu J. Bisphosphonate therapy for bone loss in patients with osteoporosis and periodontal disease: clinical perspective and review of the literature. Quintessence Int. 2006;37:103–107.
- Hujoel P, Barasch A, Cunha-Cruz J, et al.Osteonecrosis of the Jaw and Oral Hygiene: A Case-Control Study from Condor Dental PBRN.J Dent Hyg. 2012;86:32–33.
- Mawardi H, Giro G, Kajiya M, et al. A role of oral bacteria in bisphosphonate-induced osteonecrosis of the jaw. J Dent Res.2011;90:1339–1345.
- Fantasia, JE. Bisphosphonates—what the dentist needs to know: practical considerations.J Oral Maxillofac Surg. 2009;67(Suppl):53–60.
- Woo SB, Hellstein JW, Kalmar JR. Narrative[corrected] review: bisphosphonates and osteonecrosis of the jaws. Ann Intern Med.2006;144:753–761.
- Mavrokokki T, Cheng A, Stein B, Goss A.Nature and frequency of bisphosphonate associated osteonecrosis of the jaws in Australia.J Oral Maxillofac Surg. 2007;65:415–423.
- Little JW, Falace DA, Miller CS, Rhodus NL.Dental Management of the Medically Compromised Patient. 7th ed. St. Louis:Mosby/Elsevier Publishing; 2008.
- Rayman S, Almas K, Dincer E.Bisphosphonate-related jaw necrosis: a team approach management and prevention. Int JDent Hygiene. 2009;7:90–95.
- Cohen HV. Bisphosphonate-associated osteonecrosis of the jaw: patient care considerations: overview for the orthopaedic nursing healthcare professional. Orthop Nurs. 2010;29:176–180.
- Vescovi P, Nammour S. Bisphosphonate-Related Osteonecrosis of the Jaw (BRONJ)therapy. A critical review. Minerva Stomatol. 2010;59:181–213.
From Dimensions of Dental Hygiene. March 2013; 11(3): 50–53.



