Technique – Sealant Placement
Sealants are an important part of preventive care and dental hygienists must be comfortable with their recommendation and placement.
The placement of pit and fissure sealants on permanent molars is highly effective in preventing caries. Twenty percent of children experience tooth decay by age 2 or 3 and 80% of young people have a cavity by the age of 17.1 Dental hygienists are aptly suited to perform this simple preventive procedure.
 Tooth on the left should be sealed.Tooth on the right should be restored. |
In the past, pit and fissure lesions were visually inspected and clinically detected with a sharp explorer “sticking” when removed from the occlusal surface. Today, this evaluation technique is no longer the current and acceptable procedure. Tooth structures cavitate during this procedure because the surrounding supporting dental tissues have been structurally undermined.1 Created by the dental expl orer, this cavitation ultimately leads to permanent restoration.
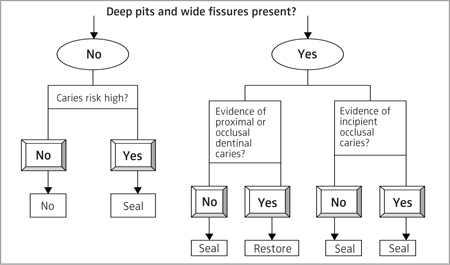
Research shows that dental hygienists hesitate placing sealants on teeth due to uncertainty of whether the tooth is carious or not.2 Dental hygienists need to be confident in their decision-making skills when confronted with a tooth with a carious or an incipient lesion. Figure 1 provides a sealant placement decision making tree.
| Figure 1. Sealant placement decision making tree.4
|
If the treatment plan calls for preventive sealants, other teeth may be at risk. The smooth surfaces of the teeth should be examined. White spot lesions or early demineralized teeth can be reversed if the caries balance is restored.3 During a preventive appointment or after the fluoride treatment, the dental hygienist should reinforce and educate the child and parent about reducing the acid attack in the mouth, including decreasing the amount of plaque, sugar consumption, and frequency of snacking. In addition, all high-risk children should have their primary and permanent molars sealed soon after eruption.
High-risk children include the medically compromised, developmentally disabled, or those with hyposalivary functions due to medications.5 Children who are at moderate risk with significant plaque, frequent snacking, and inadequate fluoride or dental care should have preventive sealants placed as well. Placement of a sealant by a dental hygienist can be considered a preventive and therapeutic treatment modality. Caries free teeth should be sealed if they have deep occlusal anatomy. Therapeutically, a sealant placed over an incipient lesion can stop the caries process provided the sealant remains intact and no portion of the sealant is lost.6
Over the years, light-cured sealant placement has not drastically changed unlike sealant material, which is constantly evolving. Improvements have been made to help clinicians manage the sealant procedure, such as better flow rates for easy penetration and colored sealants to help with visual placement. Figure 2 is a procedure table that provides step-by-step instructions for applying light-cured pit and fissure sealants.
In conjunction with a diagnosis by the supervising dentist when possible, dental hygienists should feel confident in the recommendation and placement of sealants for those at risk of caries.
| Procedure | Rationale |
|
| 1. Identification of client in need of sealant. Clinically identified by caries detection device, visual examination, or diagnosed by dentist.
2. Provide client with protective eyewear. 3. Polish with pumice using bristle brush attached to a slow-speed handpiece. Rinse. 4. Isolate teeth with rubber dam or cotton rolls. Insert saliva ejector. 5. Dry with compressed air. 6. Apply phosphoric acid etch to the tooth if indicated. 7. Rinse with copious amounts of water. 8. Replace cotton rolls, dry completely with air if indicated. 9. Use a hydrophobic primer if indicated. 10. Apply liquid sealant over pits and fissures. Allow the material to flow into the etched surface. 11. Operator uses light shield and applies light cure. 12. Evaluate the sealant with an explorer. 13. Check occlusion with articulating paper. Remove excess sealant with a finishing bur. 14. Apply topical fluoride. |
1. Unmet human need for biologically sound and functional dentition. Preventive or therapeutic management.
2. Protect eyes from particulate matter generated from polishing. 3. Surface must be free of plaque and organic debris. Air abrasion units may be used. 4. Treatment site should be visible, accessible, and dry (when indicated by manufacturer) for ultimate sealant success (see image A). 5. Presence of saliva or water compromises sealant bonding and retention in those products requiring a dry field. 6. Acid etch produces micropores to the enamel and mechanically locks the sealant for successful retention (see image B). 7. Rinsing washes away the acid. Use high volume evacuation to prevent bitter taste. 8. Sealant success depends on a dry field in those products where a dry field is required (see image C). 9. Hydrophobic primers can aid in sealant retention. 10. A low-viscosity sealant prevents air entrapment. 11. The curing process of the sealant varies by the light source. Time varies between 20-30 seconds. 12. A successful sealant feels hard and smooth without the presence of bubbles. 13. High spot interferes with normal occlusion (see image D). 14. Encourages remineralization of acid-etched surfaces. |
Acknowledgement
Thank you to Cara Miyasaki-Ching, RDHEF, MS, and Steve Eakle, DDS, for their help with photography.
References
- Sanchez-Figueras A Jr. Occlusal pit-and-fissure caries diagnosis: a problem no more. Compend Contin Educ Dent. 2003;24(5 Suppl):3-11.
- Feigal R. Making the most of sealant usage. Dimensions of Dental Hygiene. 2004;2(7):18-20.
- Featherstone JDB. The caries balance. Dimensions of Dental Hygiene. 2004;2(2):14-16.
- Yamamoto J, Fannon M. Pit and fissure sealants. In Darby M, Walsh M, eds. Dental Hygiene Theory and Practice. 2nd Ed. St Louis: Saunders; 2003: 553-561.
- Eakle S. Caries management by risk assessment (CAMBRA). Presented at: University of California, San Francisco, Alumni Meeting; January 18, 2003; San Francisco.
- Jackson R, Fontana M. Maximizing the benefits of sealants. Dimensions of Dental Hygiene. 2005;3(2): 16-21.
From Dimensions of Dental Hygiene. July 2005;3(7):18, 20.