
Support Orthodontic Treatment Success
Dental hygienists play an integral role in helping orthodontic patients maintain adequate oral hygiene—a necessity for positive treatment outcomes.
Patient motivation is crucial to the success of dental therapy. In the case of orthodontics, treatment success also depends on the patient’s commitment to maintaining good oral hygiene. Due to the biology of tooth movement within the periodontal environment, maintaining the health of both periodontal tissue and teeth during orthodontic treatment is imperative to achieving the desired end result. In this respect, dental hygienists play a major role in motivating patients to maintain good oral hygiene during orthodontic therapy.
Orthodontic treatment with fixed appliances inevitably predisposes patients to an increased risk of dental problems. Not only do fixed orthodontic appliances make performing effective oral hygiene challenging, the design of most orthodontic appliances creates additional sites that harbor plaque and oral microorganisms.
In addition, orthodontic therapy may alter saliva flow and saliva pH, while also changing the oral microbial flora. These changes make the enamel and tooth-supporting periodontal tissues more susceptible to disease.1–3 In the absence of good oral hygiene practices, two adverse effects commonly occur: enamel demineralization and gingival inflammation.
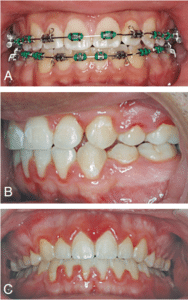
Enamel demineralization, more commonly known as white spot lesions, is frequently seen in patients who receive fixed orthodontic appliance therapy. The accumulation of plaque around orthodontic brackets, wires, and elastic ligatures creates an environment susceptible to white spot lesions (Figure 1A to Figure 1C). The bacteria at these sites cause a drop in pH and increased acid formation. White spot lesions are typically seen in close proximity to orthodontic appliances, which are difficult areas for patients to keep clean.
Gingival inflammation is the most common periodontal problem seen among patients with orthodontic appliances (Figure 2). When excellent oral hygiene is maintained, orthodontic treatment does not lead to periodontal diseases. When oral hygiene is poor, however, the orthodontic appliances may cause iatrogenic periodontal problems. Left untreated, gingival inflammation may progress to loss of bone attachment, recession, and compromised treatment outcomes.
ORTHODONTIC PATIENTS
The vast majority of orthodontic patients are children and adolescents. Developing good oral hygiene practices at this age can result in the maintenance of a strong routine into and throughout adulthood. It can be just as easy, however, to give up on these practices due to the difficulty posed by fixed orthodontic appliances. Oral health professionals are charged with promoting and encouraging patients to maintain their oral health, and helping young patients build good home-based oral hygiene practices. Doing so may help prevent or greatly reduce the risk of oral diseases, not only while undergoing orthodontic treatment, but throughout their lifetimes.
Orthodontic treatment, however, is not limited to pediatric patients. Today, most orthodontic practices also treat adults. In the absence of other local or systemic factors, there are no contraindications for orthodontic treatment among older patients. When treating adults, the orthodontic team and the dental team should both assess patients’ hygiene status prior to committing to therapy. The general dental practice and the orthodontic practice need to maintain an open line of communication in order to establish and customize oral care to the needs of each patient. Just as in the case of young patients, adult patients should be educated and prepared to maintain oral hygiene once orthodontic treatment begins.

THE ROLE OF ORAL HEALTH PROFESSIONALS
Oral health professionals cannot stress enough the importance of good oral hygiene. Therefore, a joint effort between the orthodontic practice and the general dental practice in relaying this message to patients is essential. Patients undergoing orthodontic treatment tend to delay their visit to their general dentist, under the misconception that the orthodontist can take care of their general dental health needs. For this reason, orthodontists should also educate patients about any changes that need to be made to their oral hygiene regimens. Orthodontic visits, however, cannot be considered a replacement for treatment in the general dental practice. The orthodontic practice team needs to encourage patients to maintain their follow-up regimen with their dental hygienist every 6 months.
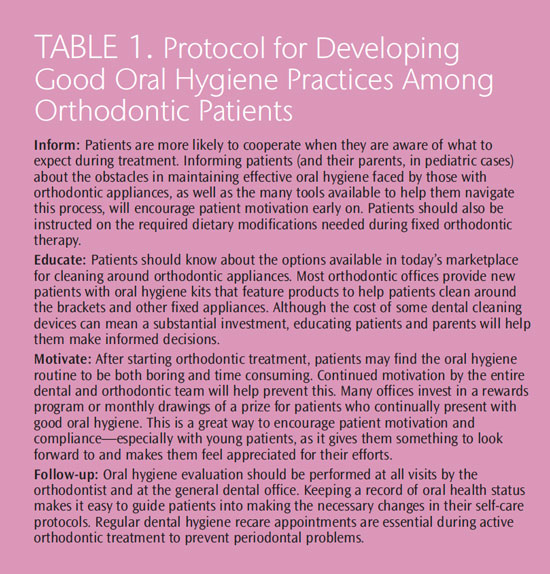
The goal of the entire interdisciplinary team, as well as the patient, is to achieve an esthetically pleasing and healthy smile. The dental hygienist plays a vital role in this process by ensuring the patient is constantly motivated to maintain good oral health, and also has the necessary education and access to the tools needed for keeping up their oral hygiene (Table 1).
PRIOR TO ORTHODONTIC TREATMENT
At the initial orthodontic visit, the patient must be evaluated for oral hygiene status, gingival inflammation, recession, and periodontal pocketing. Prior to starting active orthodontic therapy, the patient must visit his or her general dental practice to receive a thorough exam for detection of active oral diseases, including periodontal diseases and caries. All active diseases must be treated prior the start of orthodontic therapy. The presence of orthodontic appliances not only makes it difficult to carry out general dental treatment, but also can lead to a rapid progression of untreated disease.
A pretreatment visit to the dental hygienist must include an evaluation of the patient’s oral hygiene status and self-care routine, in addition to education about how to best maintain oral health once the orthodontic appliances are installed. An assessment of periodontal health, pocket depths, and the presence of gingival inflammation and recession, along with scaling, root planing, and plaque removal, must be performed at this visit.
DURING ORTHODONTIC TREATMENT
To facilitate good oral hygiene during orthodontic treatment, a variety of dental cleaning aids designed for patients with orthodontic appliances are available. Cleaning to achieve plaque removal with orthodontic appliances can be an overwhelming task. Power toothbrushes may be more effective in plaque removal among patients with multi-bracketed orthodontic appliances than manual toothbrushes.4 There are power brush heads designed specifically for cleaning around orthodontic brackets. Not all patients, however, will decide to invest in a power toothbrush. Patients who prefer manual toothbrushes may benefit from the use of brush heads designed specifically to clean around orthodontic brackets. Patients must be instructed to brush the labial, as well as lingual surfaces of all teeth. With the increase in popularity and use of lingual brackets, oral hygiene can become even more challenging than with labial appliances. Often, patients do not put enough concentrated effort into brushing the lingual surfaces of teeth, which are more likely to accumulate plaque and calculus buildup—even in the absence of orthodontic appliances.
Access to the interdental area is more difficult with brackets and wires. Interdental brushes allow the patient to clean these areas more effectively. Different designs may make it easier to maneuver around the orthodontic appliances. Although interdental brushes effectively remove plaque, there is some debate about whether they are a cost-effective addition to the oral hygiene regimen for orthodontic patients.5–7 Anecdotal evidence obtained in clinical practice generally supports the use of interdental brushes, as patients use them not only for cleaning the designated areas, but also to remove food and plaque debris adhered to the brackets and undercuts on most fixed orthodontic appliances.
The benefits of toothbrushing cannot be reaped without utilizing proper technique. Between three groups of toothbrushing techniques in orthodontic patients over a period of 9 months, those who used the Bass technique showed a significant improvement in the plaque index and gingival index.8 The widespread availability of power toothbrushes has increased their use among patients; as a result, patients tend to be less diligent with technique. Reemphasizing proper brushing technique, both in the orthodontic and dental offices, may help cement its importance in reducing plaque.
The application of fluoride varnish is an effective measure in preventing or reducing demineralization during orthodontic treatment.9 Fluoride varnish is a necessity for those patients with poor oral hygiene. The use of fluoride dentifrice is always recommended, and the addition of antimicrobials, such as triclosan and cetylpyridinium chloride, may also prove beneficial. One study found that patients who brushed with propolis-containing toothpaste (a resin-like material collected by bees from trees and buds that possesses antimicrobial properties) showed significantly improved oral hygiene, as evaluated by the orthodontic plaque index and gingival index, when compared to those who brushed with a toothpaste without propolis.10
The application of sealants should also be considered before orthodontic therapy begins. O’Reilly et al11 found that teeth treated with sealants prior to orthodontic treatment had a statistically significant decrease in the development of white spot lesions on treated teeth by the end of the therapy. Although adjunctive preventive measures are most certainly valuable in the prevention of demineralization and caries, conventional plaque control measures and a daily oral hygiene regimen are key players in the successful prevention of active oral diseases.
Flossing the interdental areas can be a tedious job with brackets and wires bonded to the teeth. Fortunately, advancements in interdental cleaning devices provide patients a variety of options to choose from. Products, such as floss threaders, floss holders, and other adjuncts used with traditional floss, can make this task more manageable. Besides floss devices and interdental brushes, water irrigation devices are also available. These products may also help in cleaning the interdental area and the gingival sulcus (flushing zone).12 Whatever the method, interdental cleaning reduces the incidence of gingival bleeding and inflammation; decreases the presence of inflammatory mediators, such as interleukins and prostaglandins; and promotes a stable periodontal support for the teeth before, during, and after orthodontic treatment.12–15
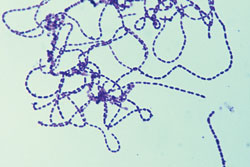
Orthodontic patients with poor oral hygiene are at significantly greater risk of developing white spot lesions than patients with good to moderate compliance.16 Acharya et al found17 that the use of phase contrast microscopy (technique that uses shifts in light to highlight changes in the specimen, Figure 3), in conjunction with plaque disclosure, was more successful in motivating patients to effectively perform oral hygiene than conventional plaque control measures. In the study, orthodontic patients were shown a sample of their plaque under a phase contrast microscope to demonstrate the presence of live motile bacteria in their own biofilm.17
Investing in orthodontic therapy to achieve a healthy and esthetic smile calls for changes not only to the oral hygiene routine of the patient, but also to the diet. Patients should be instructed to avoid highly fermentable carbohydrates in foods (lactose, fructose), and to limit intake of sugary and sticky foods (soda, candy). Brushing and rinsing immediately after every meal is necessary. Carbonated drinks that may alter pH—such as soft drinks and sports drinks, which are also high in sugar—must be limited in order minimize the risk for enamel demineralization.
Orthodontic patients must maintain the best oral hygiene possible to ensure the health of their teeth after treatment, as well as the integrity of the orthodontic appliances for the duration of the treatment plan. Any breakage in appliances is a setback to the progress of treatment. Research shows that ultrasonic instrumentation can decrease the bond strength of flowable composite to the tooth enamel and dentin.18,19 The use of ultrasonic scalers among orthodontic patients is not contraindicated, however, as long as care is taken to work around the bonded appliances. Dental hygienists need to be careful to ensure that appliances are not affected by scaling and debridement. The overflow of composite around orthodontic brackets may be frequently encountered by the dental hygienist. The removal of excess composite around brackets using hand instruments or ultrasonic scalers should be avoided as much as possible. Using the dental handpiece with an appropriate bur is the best means for removing excess composite around brackets because it will not compromise the bond strength of the brackets.
POST-ORTHODONTIC TREATMENT
At the end of orthodontic treatment, patients must visit their general dental practice. Even when patients have exercised the best hygiene habits during orthodontic therapy, some level of plaque and calculus buildup is inevitable. The post-debonding dental appointment must include reevaluation of periodontal status, along with pocket measurements and periodontal debridement. A complete series of radiographs must be taken to evaluate for bone loss, as well as any caries activity. Some patients, especially adults, may become more aggressive with their brushing when undergoing orthodontic treatment. At the end of treatment, patients’ oral hygiene regimens should be reevaluated, and additional education should be provided to help patients prevent trauma caused by overzealous brushing habits.20
CONCLUSION
Helping patients maintain good oral hygiene during orthodontic treatment requires a team effort that involves not only the dental and orthodontic teams, but also the patients themselves. It is the professional and ethical responsibility of all interdisciplinary team members to regularly evaluate, educate, and reinforce healthy oral habits and practices with orthodontic patients. The role of the dental hygienist is vital in influencing patient motivation and commitment to the upkeep of oral health, not only for the duration of orthodontic treatment, but also post-treatment to ensure patients’ improved smiles remain beautiful and healthy for life.
REFERENCES
- Lundström F, Krasse B. Streptococcus mutans and lactobacilli frequency in orthodontic patients; the effect of chlorhexidine treatments. Eur J Orthod.1987;9:109–116.
- Rosenbloom RG, Tinanoff N. Salivary Streptococcus mutans levels inpatients before, during, and after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991;100:35–37.
- Chang HS, Walsh LJ, Freer TJ. The effect of orthodontic treatment on salivary flow, pH, buffer capacity, and levels of mutans streptococci and lactobacilli. Aust Orthod J. 1999;15:229–234.
- Erbe C, Klukowska M, Tsaknaki I, Timm H, Grender J, Wehrbein H. Efficacy of 3 toothbrush treatments on plaque removal in orthodontic patients assessed with digital plaque imaging: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2013;143:760–766.
- Goh HH. Interspace/interdental brushes for oral hygiene in orthodontic patients with fixed appliances. Cochrane Database Syst Rev.2007;18:CD005410.
- Schmage P, Platzer U, Nergiz I. Comparison between manual and mechanical methods of interproximal hygiene. Quintessence Int.1999;30:535–539.
- Bock NC, von Bremen J, Kraft M, Ruf S. Plaque control effectiveness and handling of interdental brushes during multibracket treatment—a randomized clinical trial. Eur J Orthod. 2010;32:408–413.
- Nassar PO, Bombardelli CG, Walker CS, et al. Periodontal evaluation of different toothbrushing techniques in patients with fixed orthodontic appliances. Dental Press J Orthod. 2013;18:76–80.
- Nalbantgil D, Oztoprak MO, Cakan DG, Bozkurt K, Arun T. Prevention of demineralization around orthodontic brackets using two different fluoride varnishes. Eur J Dent. 2013;7:41–47.
- Machorowska-Pien??ek A, Morawiec T, Mertas A, Tanasiewicz M, DziedzicA, Król W. Influence of propolis on hygiene, gingival condition, and oral microflora in patients with cleft lip and palate treated with fixed orthodontic appliances. Evid Based Complement Alternat Med. 2013;2013:183915.
- O’Reilly MT, De Jesús Viñas J, Hatch JP. Effectiveness of a sealant compared with no sealant in preventing enamel demineralization in patients with fixed orthodontic appliances: a prospective clinical trial. Am J Orthod Dentofacial Orthop. 2013;143:837–844.
- Sharma NC, Lyle DM, Qaqish JG, Schuller R. Comparison of two power interdental cleaning devices on plaque removal. J Clin Dent. 2012;23:17–21.
- Jackson MA, Kellett M, Worthington HV, Clerehugh V. Comparison of interdental cleaning methods: a randomized controlled trial. J Periodontol.2006;77:1421–1429.
- Kossack C, Jost-Brinkmann PG. Plaque and gingivitis reduction in patients undergoing orthodontic treatment with fixed appliances-comparison of toothbrushes and interdental cleaning aids. A 6-month clinical single-blindtrial. J Orofac Orthop. 2005;66:20–38.
- Rosema NA, Hennequin-Hoenderdos NL, Berchier CE, Slot DE, Lyle DM,van der Weijden GA. The effect of different interdental cleaning devices on gingival bleeding. J Int Acad Periodontol. 2011;13:2–10.
- Hadler-Olsen S, Sandvik K, El-Agroudi MA, Øgaard B. The incidence of caries and white spot lesions in orthodontically treated adolescents with a comprehensive caries prophylactic regimen—a prospective study. Eur J Orthod. 2012;34:633–639.
- Acharya S, Goyal A, Utreja AK, Mohanty U. Effect of three different motivational techniques on oral hygiene and gingival health of patients undergoing multi bracketed orthodontics. Angle Orthod. 2011;81:884–888.
- El Hafiz ESA, Elewa M, Hammoda IM. Effect of the vibration of ultrasonic scaling on composite restorative materials (in vivo and in vitro study).Egyptian Dental Journal. 2004;50(4.2):2101.
- [The impact of ultrasonic dental hygiene procedures on the bonding strength of restorations]. Stomatologiia (Mosk). 2013;92:36–39.
- Sanders NL. Evidence-based care in orthodontics and periodontics: a review of the literature. J Am Dent Assoc. 1999;130:521–527.
From Dimensions of Dental Hygiene. October 2013;11(10):22–24,26–27.

