 ALEX-MIT STOCK/THINKSTOCK
ALEX-MIT STOCK/THINKSTOCK
Strategies to Maintain Complex Implant Restorations
Understanding prosthetic design is essential to tailoring effective maintenance regimens for the prevention and treatment of peri-implant diseases.
This course was published in the December 2016 issue and expires December 31, 2019. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the dental hygienist’s role in the maintenance of complex implant-borne restorations.
- Explain peri-implant mucositis and peri-implantitis as they relate to implant outcomes, and differentiate between the two conditions.
- Identify challenges to the assessment and treatment of peri-implant diseases, and list the steps clinicians can take to help ensure successful long-term implant outcomes.
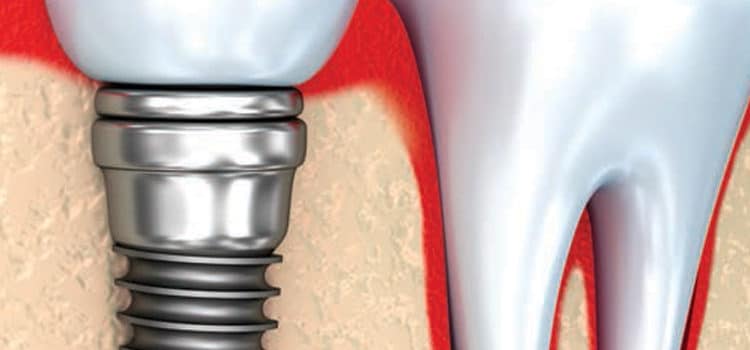
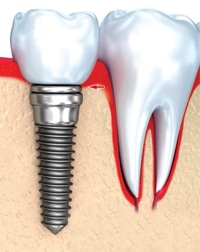
With the known associations between oral health and overall health, tooth loss can significantly compromise individuals’ quality of life. Fortunately, technological advances allow the placement of dental implants in a wide range of cases.1 In the United States, 300,000 dental implants to 428,000 dental implants are placed annually and restored with fixed or removable prostheses.2,3 Implants are not subject to decay (due to lack of natural tooth structure). However, oral biofilm must be managed, as evidence has shown that microbial colonization at the gingiva/implant interface (Figure 1) can induce peri-implant mucositis or peri-implantitis and jeopardize implant outcomes.2,4
While current guidelines for maintaining implant-supported prosthetics are poorly defined, periodic evaluation by a dental professional is suggested for the preservation of healthy peri-implant tissues. With dental hygienists at the forefront of oral disease prevention and detection, knowing how to assess and treat peri-implant diseases is part of the dental hygiene standard of care.1,3,5 Complicating factors in this endeavor include the multifaceted structure of implant-supported prostheses and anatomical challenges that can make plaque control difficult (Figure 2).6 Clinicians and patients need to be aware of anatomical challenges because they can interfere with the professional and at-home mechanical removal of biofilm and food debris. Understanding how to navigate through and around the complex structural design of these prosthetics is necessary to effectively disrupt the bacterial colonization and food impaction that occur around implants and prostheses.1,4
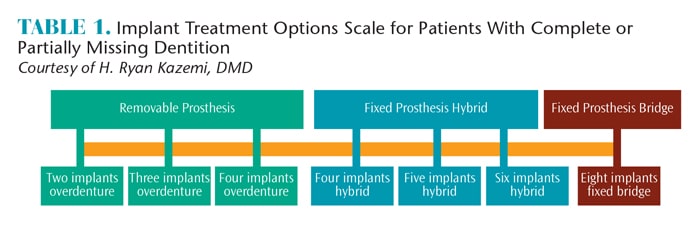
The implant treatment options for partially or fully edentulous patients depend on the type of prosthesis desired by the patient, and whether an adequate amount of jawbone is present (Table 1). The patient may choose a fixed or removable prosthetic. A fixed prosthesis can be either a hybrid denture or an implant-supported bridge.7
ALEX-MIT STOCK/THINKSTOCK
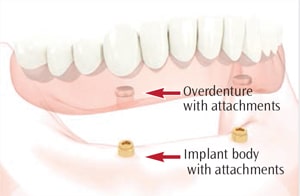
A removable prosthesis or overdenture includes a removable full set of prosthetic teeth that may be supported by two implants to four implants, depending on its location (maxilla or mandible). For example, Figure 3 illustrates an overdenture supported by two implants in the mandible. The overdenture snaps onto the supporting implants. These attachments have male and female components: one attaches to the implant body, and the other attaches to the inside of the overdenture.1 Depending on the design, the components can be magnets, clips, locators, or ball attachments.7 The components located on the inside of the overdenture can be removed and/or changed as needed.1
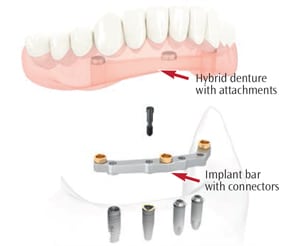
Hybrid dentures, also known as fixed detachable dentures, are a mixed design that combine the benefits of a fixed replacement with the advantages of a removable denture.7 This prosthesis is a cross between a traditional denture and a fixed bridge that does not require daily removal because it is screw retained into the implants. This means it can be detached by the dentist.1 Depending on the shape and size of the jaw, this prosthesis may be supported by four implants to eight implants.

Various methods are used to attach hybrid dentures to implants. One approach connects the dental implants to the denture through abutments that are screwed into a metal framework known as an implant bar (Figure 4). The bar is screwed into the dental implants, and the prosthesis is screwed into the implant bar. Other examples of hybrid dentures are the “all-on-four” and fixed dentures supported by five to six implants.1 These designs typically have a metal substructure that is attached to the implants.
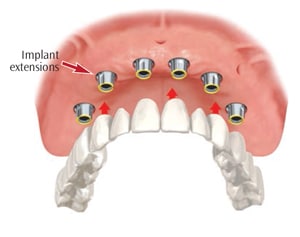
“All-on-four” is a fixed denture mounted on four implants (Figure 5). This is a minimal design that may be appropriate for patients with less-than-optimal bone levels. The prosthesis is screwed directly into the implant abutments.8 When five implants to six implants are used, an overdenture with a metal substructure is fixed to the implant extensions. Implant-supported overdentures with six implants provide optimum support, making this an ideal option for hybrid dentures.1
Another option for the edentulous patient is a fixed implant-supported bridge (Figure 6), which is a conventional bridge made of porcelain or other ceramic material and supported by six implants to eight implants.1 A bridge design is suitable for patients with minimal or no loss of bone and gingiva, as the bridge only replaces the crown aspect (ie, there is no denture base). Fixed implant-supported bridges closely resemble the look and feel of natural dentition. The fixed implant-supported bridge is customized for each case and cannot be removed by the patient.1 Extensions are attached to the dental implants, and the bridge is fixed onto the implants.
ANATOMICAL CHALLENGES
Clinically, when performing implant hygiene and assessment, the critical areas include the surfaces around the attachments for fixed or hybrid overdentures, and the gingiva/implant interface of implant-supported fixed bridges.1,4 Often, anatomical challenges may be present that make oral hygiene care difficult for the patient and clinician. Dental professionals must understand the mechanical design of implant-supported restorations in order to overcome challenges when treating patients with full-arch, implant-supported prosthetics.4
With removable implant-supported dentures, the implant superstructures are easily accessible once the denture is removed.5 The prosthesis should be evaluated for retention, surface damage, and cleanliness.9 The soft tissues of the oral cavity should be examined for signs of inflammation, including denture irritation and peri-implant diseases around the attachments.5 Patients should be advised to remove the denture overnight, or at least for several hours each day, to prevent denture stomatitis.9 Fixed hybrid overdentures cannot be removed by the patient, which limits access to the implant superstructures and restoration surfaces. Because they cannot be removed, hybrid dentures are designed to allow space between the prosthesis and jawbone. This provides access underneath the denture for ease of cleaning. A potential downside to this design is the risk of food impaction and inflammation.
Another anatomical challenge of fixed dentures is presented by buccal and labial flanges. Denture flanges extend into the vestibule areas to help support the lips and cheeks—although this makes the buccal and labial surfaces of the implant superstructures inaccessible for hygiene care.
A correct fit and complete seating of implant components—as well as superstructures—must be ensured to minimize niches that promote biofilm adherence. With a fixed conventional full-arch bridge, anatomical challenges present when the pontic’s emergence profile does not mimic the natural tooth (emergence profile describes the contour of a crown as it emerges from the gingiva). Poorly shaped implant crowns can create inaccessible undercuts; in turn, this results in embrasure spaces and abutments that are unreachable from all surfaces. An improper emergence profile can also create embrasure spaces that allow food impaction, or small, tight embrasures that are difficult to access with oral hygiene aids. Clinicians should be aware that implant placement at a submucosal level (to hide crown margins) may raise the risk of infection. This can compromise professional and self-care efforts to remove biofilm and food debris, making the patient vulnerable to peri-implant infections.2
IMPLANT MAINTENANCE

The clinical goal of implant care is identical to that for natural dentition: biofilm control—except that implant maintenance must be accomplished without harming the implant surface and prosthesis.1 Studies have demonstrated that microbiotic pathogens adhere to implant surfaces that are rough or scratched—and because it is possible to scratch implants in therapy, the efficacy of scaling will be compromised if scratches encourage microbial buildup and inflammation.4 In order to achieve optimal implant care for patients with hybrid dentures or fixed bridges, professionally removing the
prosthesis may aid dental hygienists by allowing complete access to implant superstructures.5 The prosthesis should be evaluated for surface scratches and cleanliness while inside the oral cavity and outside of the mouth.1 Prior to treatment, implant components and surrounding tissues should be examined for signs of peri-implant diseases, plaque accumulation, and food deposits.10
Performing a radiographic examination of dental implants is critical to assess implant health and detect possible problems. Dental plaque may be left underneath an implant-supported prosthesis that is not fully seated, which may result in peri-implant disease.11 Radiographs also provide a point of comparison for future maintenance visits.
Peri-implant mucositis is reversible inflammation in the soft tissue around the implant characterized by erythema, bleeding on probing, possible presence of exudate, and no bone loss.12,13 Peri-implantitis presents with the characteristics of peri-implant mucositis, except the microbiotic pathogens have invaded the bone, resulting in bone loss.12,13 If exudate is present—with or without increased pocket depths—a radiographic examination of the implant site is necessary to assess the underlying supporting structures and rule out peri-implant mucositis or peri-implantitis induced by a foreign object.
A thorough assessment is necessary to plan an evidence-based, individualized therapeutic and preventive approach to care.2,10,14 The clinical detection of bleeding on probing is essential for the diagnosis of peri-implant mucositis, while the presence of deep pocketing indicates peri-implantitis.2,10,14 Although researchers have debated which probe to use—with some of the literature suggesting plastic probes and other studies recommending metal probes—all research indicates the need for gentle probing. Inappropriate probing pressure can induce bleeding and increase pocket depths, even at healthy sites.12,14
Subsequent to data collection, clinicians should determine if the patient’s oral condition suggests the use of hand instruments for the mechanical debridement of calculus and/or cement,14 ultrasonic irrigation for biofilm disruption, and/or the use of locally applied antibiotics. Clinicians should also determine best practices and products for prevention protocols and self-care maintenance.5 Although current research suggests limited efficacy with mechanical debridement in the nonsurgical treatment of peri-implantitis, many studies agree the use of adjunctive measures may improve overall outcomes.12 While some in vitro research has shown that metal instruments can cause scratching of the implant surface,4,10 other types of instruments, such as plastic, may not effectively remove calculus.15
Adjunctive measures may include, but are not limited to, ultrasonic lavage with an antimicrobial solution, locally applied antibiotics, and glycine air powder polishing.5,14 Subgingival lavage with an antimicrobial solution and a carbon-composite minitip on an ultrasonic scaler used at low amplitude may be helpful when nonsurgical treatment is warranted. If exudate presents—with or without bone loss—the subgingival delivery of a locally applied antibiotic is suggested after ultrasonic irrigation. The patient should return for a 1-month follow-up to reevaluate the implant site for signs of an arrested infection (eg, no exudate and decreased bleeding on probing). If the infection persists, a referral to a periodontist or oral surgeon is warranted.10,14
With or without adjunctive therapy, professional implant maintenance can reverse peri-implant mucositis and arrest early bone loss. Moderate to severe peri-implantitis should be referred for surgical consultation.2,12,13 Recent clinical practice guidelines published by the American College of Prosthodontists suggest that patients with favorable implant health should return for maintenance appointments at least every 4 months to 6 months. The guidelines further suggest implant maintenance protocols should be individually based and dependent on risk factors associated with the oral/systemic link and limitations to care.5
ORAL HYGIENE INSTRUCTIONS
In all implant cases, effective self-care is imperative to successful long-term outcomes—and this is particularly true for patients with full-arch, implant-supported prostheses. Research indicates that 3 weeks of ineffective or poor oral hygiene practice will contribute to peri-implant mucositis.12 Professional plaque control should include regular oral hygiene instructions tailored to a patient’s individual needs.5,12,13 Appropriate interproximal cleaning methods should be recommended, such as the use of interdental brushes with plastic-coated wires, soft picks, rubber tip stimulators, air flossers, and/or water flossers.5 Emerging evidence suggests the use of dental floss may be a possible risk factor for the development of peri-implant diseases. In an observational study of 10 patients with progressive peri-implantitis, remnants of dental floss were found around the neck and coronal portion of dental implants.16 Brushing with a power toothbrush in conjunction with the use of an antimicrobial were found to be safe and effective for self-care maintenance of implant-supported prostheses.2,5
CONCLUSION
Patients who qualify for implant-supported prosthetics can realize significant benefits—including the preservation of alveolar bone structures, as well as improved esthetics and oral function. Proper oral care is essential to the longevity of dental implants, yet anatomical challenges exist that can make biofilm disruption and plaque control complex for patients and practitioners.5 Dental hygienists are at the forefront of prevention and detection of oral diseases, thus, patient education and effective implant maintenance are key to today’s standard of care.1–3,5 Understanding prosthetic design is essential to tailoring effective professional and self-care maintenance regimens for the prevention and treatment of peri-implant diseases.1
REFERENCES
- Wingrove SS. Peri-Implant Therapy for the Dental Hygienist: Clinical Guide to Maintenance and Disease Complications. Ames, Iowa: Wiley Blackwell; 2013.
- Jepsen S, Berglundh T, Genco R, et al. Primary prevention of peri-implantitis: Managing peri-implant mucositis. J Clin Periodontol. 2015;42(Suppl 16):S152–S157.
- Ward ST, Czuszak CA, Thompson AL, Downey MC, Collins MA. Assessment and maintenance of dental implants: Clinical and knowledge-seeking practice of dental hygienists. J Dent Hyg. 2012;86:104–110.
- Hasturk H, Nguyen DH, Sherzai H, et al. Comparison of the impact of scaler material composition on polished titanium implant abutment surfaces. J Dent Hyg. 2013;87:200–211.
- Birda AS, Daubert DM, Garcia LT, et al. Clinical practice guidelines for recall and maintenance of patients with tooth-borne and implant-borne dental restorations. J Prosthodont. 2016;25(Suppl 1):S32–S40.
- Geminiani A. Treatment Planning Guidelines and Prosthetic Options for the Edentulous patient. Available at: dentalacademyofce.com/courses/ 3022/PDF/1604cei_Geminiani_web.pdf. Accessed October 14, 2016.
- Selim K, Ali S, Reda A. Implant supported fixed restorations versus implant supported removable overdentures: A systematic review. Available at: id-press.eu/mjms/article/download/oamjms.2016.109/1131. Accessed October 14, 2016.
- Patzelt SB, Bahat O, Reynolds MA, Strub JR. The all-on-four treatment concept: a systematic review. Clin Implant Dent Relat Res. 2014;16:836–855.
- Dhanvarachom Cho S, Phasuk K, Levon JA. An evidence-based look at denture care. Dimensions of Dental Hygiene. 2016;14(6):20–23.
- Matsuda SA. Prevent cement-associated peri-implantitis. Dimensions of Dental Hygiene. 2014;12(11):34–37.
- Broggini N, McManus LM, Hermann JS, Medina R, Schenk RK, Buser D, Cochran DL. Peri-implant inflammation defined by the implant- abutment interface. J Dent Res. 2006;85:473–478.
- Schwarz F, Becker K, Sager M. Efficacy of professionally administered plaque removal with or without adjunctive measures for the treatment of peri-implant mucositis. A systematic review and meta-analysis. J Clin Periodontol. 2015;42 (Suppl 16):S202–S213.
- Renvert S, Polyzois I. Risk indicators for peri-implant mucositis: a systematic literature review. J Clin Periodontal. 2015;42(Suppl 16):S172–S186.
- Pattison AM, Sumi JY. Post-surgical implant care. Dimensions of Dental Hygiene. 2015;13(5):24–29.
- Hempton TJ, Bonacci FJ, Lancaster D, Pechter JE. Implant maintenance. Dimensions of Dental Hygiene. 2011:9(1):58–61.
- van Velzen FJ, Lang NP, Schulten EA, Ten Bruggenkate CM. Dental floss as a possible risk for the development of peri-implant disease: an observational study of 10 cases. Clin Oral Implants Res. 2016;27:618–621.
From Dimensions of Dental Hygiene. December 2016;14(12):36–39.