 ALEX-MIT/ISTOCK/THINKSTOCK
ALEX-MIT/ISTOCK/THINKSTOCK
Caring For Patients with Ehlers-Danlos Syndrome
Dental hygienists are well positioned to identify, treat, and refer patients who present with suspected or confirmed EDS signs and symptoms.
This course was published in the February 2018 issue and expires February 2021. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Describe and define Ehlers-Danlos syndrome.
- Discuss the diagnosis of EDS.
- Identify the oral health issues that may present in patients with EDS.
Due to advances in genotyping, gene mutations have been isolated in many types of EDS, supporting the theory that an inheritable factor exists in this rare disorder.3,9–13 Identification through genetic testing is not always definitive; therefore, systemic and oral manifestations are helpful in establishing an EDS diagnosis.
Patients can experience a variety of oral signs and symptoms that may be related to EDS. Different degrees of fragile mucosa, temporomandibular joint (TMJ) pain and dislocations, extensive bleeding on probing, early-onset, severe periodontitis, and premature tooth loss are some of the many oral complications.1,3–6,9,13 Dental hygienists are in a unique position to identify, treat, and refer patients who present with suspected or confirmed EDS.4,5,14 Dental hygiene treatment planning must cautiously consider and address each symptom in order to provide safe oral care. Validating patient concerns and providing dental hygiene care and referral to other health care providers may support well-being for this patient population.2
OVERVIEW OF EDS
The prevalence of EDS worldwide is estimated to be one in 5,000 people.2,4,5,7,12,15 All races and ethnicities are affected, with an equal distribution noted between men and women.1,2,4–5 While the most predominant types are classical and hypermobility, the most serious type is vascular, which can be life-threatening.11 Vascular EDS is rare with an estimated prevalence of one in 250,000 people.15
EDS alters collagen type I, III, and V formation—the primary collagen in the lamina propria—and can subsequently weaken gingival tissue.1,4,13 Cementum also contains collagen, so new cementum formation and gingival re-attachment may be delayed in periodontal diseases associated with EDS.1 In addition, collagen types I, III, and V are found in the tooth dentin and pulp, bone, mucosa, periodontal ligament, and TMJ, so any one of these structures could ultimately be affected by EDS.1,3,4
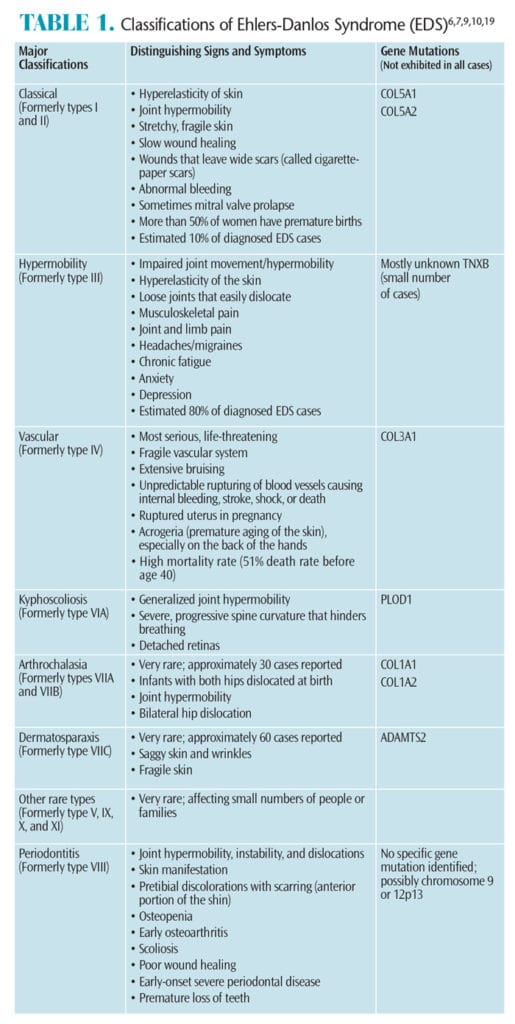
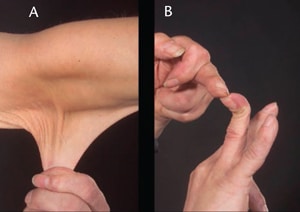
Table 1 describes the six major types of EDS.4,9,10,15,16 Vascular EDS can be fatal by causing the rupture of arterial and gastrointestinal walls.2,10,17 Additionally, complications associated with vascular EDS affect not only the vascular system—causing internal bleeding and stroke—but they can also cause the uterus to rupture during pregnancy.11,15 Joint hypermobility and skin elasticity are typical traits for most types of EDS, but they are not always present. Acute and chronic joint and/or limb pain are also common symptoms.1,5,18 Murray et al10 surveyed more than 400 adults with hypermobility-type EDS and found that the majority reported joint and limb pain, hypermobility, chronic fatigue, anxiety, and depression.
Each patient presents with a unique set of clinical indicators; thus, disability can range from mild to severe. Chronic fatigue and pain are common in EDS and can negatively impact quality of life and contribute to disability.8,18 Due to the impact on daily living, many patients with EDS experience depression and anxiety.10,19,20
MEDICAL MANAGEMENT AND DIAGNOSIS
EDS diagnosis is based primarily on clinical signs and symptoms of joint hypermobility, joint dislocations, easy bruising, joint and limb pain, chronic fatigue, and family history.7,10 Although many gene mutations have been identified for various types of EDS, not all cases within a particular type will present with the gene mutation. Genetic testing and counseling may be warranted in some cases to assist in diagnosis. The periodontitis type of EDS (formerly VIII) has been associated with a dominant inherited factor because of the strong familial patterns in multiple generations.9 When multiple family members present with rapidly progressive aggressive periodontitis, the genetic factor could be the periodontitis type of EDS.9
Individuals with EDS are likely underdiagnosed because they usually seek treatment for vague symptoms of chronic pain, and EDS is often overlooked by physicians.2,10 While there is currently no cure for EDS, treatment modalities focus primarily on patient symptoms and generally consist of pain management; use of antidepressants, muscle relaxers, and glucosamine; supplementation with vitamin C to aid wound healing; physical therapy; cognitive behavioral therapy; and lifestyle modifications.4,7,10
In addition to treating the physical symptoms, patient depression and anxiety also need to be managed though an interdisciplinary approach.10 A patient’s health care team should address each aspect of the disorder.
DENTAL HYGIENE CARE
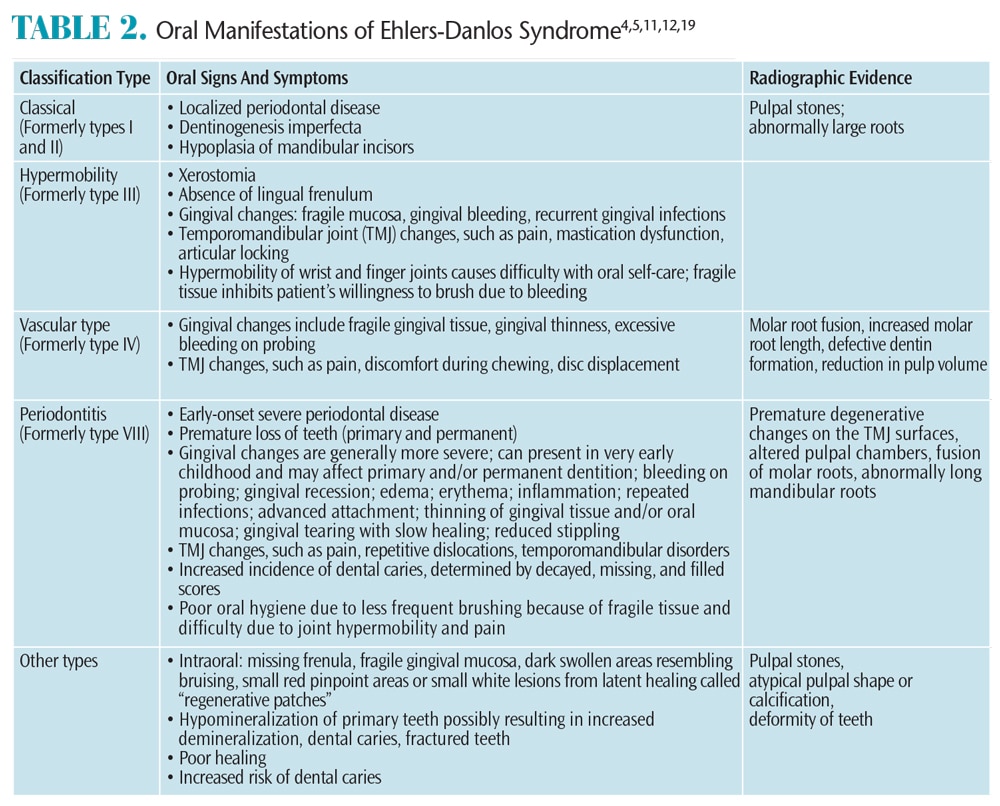
In some cases, EDS can be recognized through oral signs and symptoms (Table 2).4,5,11,12,19 For example, rapidly progressing aggressive periodontal involvement in children could indicate EDS.1 If an undiagnosed case of EDS is suspected by the dental hygienist, patient referrals might include a dermatologist, rheumatologist, cardiologist, and ophthalmologist to make a definitive diagnosis.14
Extraoral and intraoral examinations might reveal facial scars on the chin or forehead and TMJ disorder with repeated dislocations.14 Additionally, patients may exhibit thinning hair, wide nasal bridge, and palpable, movable nodules under the skin.4 In about 50% of EDS cases, patients exhibit Gorlin’s sign, or the ability to touch the tongue to the tip of the nose.14 Tulika and Kiran4 described possible extraoral features of patients with vascular type EDS as having “prominent eyes, pinched noses, small lips, hollow cheeks, and lobeless ears.” Radiographic examinations may reveal signs such as premature TMJ degeneration, decreased pulpal tissue, abnormally long roots, and molar root fusion.

Due to the prevalence and aggressiveness of periodontitis for many patients with vascular- and periodontitis-type EDS, careful and frequent oral assessment must be conducted to address relevant changes.5 Children with periodontitis-type EDS are highly susceptible to gingival recession on primary and permanent dentition, gingival bleeding after brushing, and premature tooth loss.3,9,14 Intraoral exams for vascular-type EDS may reveal gingival thinness and transparency and excessive bleeding on probing (Figure 2).21
Early diagnosis of periodontal conditions with appropriate interventions support the long-term prognosis.3 Treatment includes: nutritional counseling; education on the oral and systemic effects of EDS; demonstration of oral self-care techniques; nonsurgical periodontal therapy or prophylaxis, possibly in conjunction with systemic antibiotics; topical fluoride application; frequent recare intervals; and physician or periodontist referral.5 Additionally, providing referrals to other health care professionals, such as physical or occupational therapists to strengthen the muscles used for self-care; dietitians for nutritional support; and/or psychologists to address anxiety or depression is essential.16 Shorter dental/dental hygiene appointments may help prevent TMJ dislocations and pain.1,14 Care must be taken to avoid orthostatic hypotension.6
Anesthesia during scaling and root planing must be administered with caution, as an inferior alveolar nerve block may cause a hematoma.4,14 If significant scarring has occurred, local anesthesia might be blocked from infiltrating the tissues.4 In addition, gingival tissue can be very thin and easily torn during scaling procedures.14
Finally and most important, the need for meticulous patient oral self-care must be emphasized.3 Patients with wrist hypermobility may have difficulty with oral hygiene.1,4 If the gingival tissue is fragile, patients tend to brush less frequently, leading to high plaque scores and furthering oral disease.1,4 Ineffective brushing might increase the risk of demineralization and dental caries.12 Dental hygienists should recommend ultra-soft toothbrushes to prevent damage to the gingival margin.1
OTHER ORAL HEALTH CONSIDERATIONS
Even with periodontal treatment, patients with periodontitis type EDS can prematurely lose teeth.9 Blood tests to establish bleeding coagulation time should be performed prior to oral surgery procedures—such as extractions—due to the possibility of bleeding problems.14 During orthodontic treatment, patients must be carefully monitored because of the increased likelihood of bone resorption.3 Additionally, orthodontic treatment is likely to relapse in this population, so patients should be encouraged to wear retainers and comply with treatment.4,14
Treatment for temporomandibular disorder includes eating soft foods, avoiding wide or straining jaw movements, using ice packs to alleviate pain, and avoiding any type of occlusal adjustment to the dentition.22 If possible, noninvasive treatment is best due to the fragility of the tissue and the high risk of excessive scar tissue formation.1,22
CONCLUSION
Understanding the systemic and oral complications for EDS might save a life or extend the dentition’s longevity. The range of EDS signs and symptoms is vast and unique to each patient. Dental hygienists can identify abnormalities both extraorally and intraorally. Because of past negative medical encounters, dental professionals might be the only health care providers to identify EDS symptoms. While EDS is rare, under-diagnosis is common.2,6,7,10,19 Dental hygienists are needed not only to treat oral disease, but also to ensure patients have access to interdisciplinary specialists. The focus for EDS patients is improved oral health, as well as increased quality of life.
REFERENCES
- De Coster PJ, Martens LC, De Paepe A. Oral health in prevalent types of Ehlers-Danlos syndromes. J Oral Pathol Med. 2005;34:298–307.
- Berglund B, Anne-Cathrine M, Randers I. Dignity not fully upheld when seeking health care: Experiences expressed by individuals suffering from Ehlers-Danlos syndrome. Disability and Rehabilitation. 2010;32(1):1–7.
- Mataix J, Banuls J, Munoz C, Bermejo A, Climent JM. Periodontal Ehlers-Danlos syndrome associated with type III and I collagen deficiencies. Br J Dermatol. 2008;158:825–830.
- Tulika W, Kiran A. Ehlers-Danlos syndrome. Journal of Dental Research and Review. 2015;2(1):42–46.
- Perez LA, Al-Shammari KF, Giannobile WV, Wang H. Treatment of periodontal disease in a patient with Ehlers-Danlos syndrome. A case report and literature review. J Periodontol. 2002;73:564–570.
- Castori M, Morlino S, Ghibellini G, Celletti C, Camerota F, Grammatico P. Connective tissue, Ehlers-Danlos syndrome(s), and head and cervical pain. Am J Med Genet C Semin Med Genet. 2015;169C:84–96.
- Castori M. Ehlers-Danlos Syndrome, hypermobility type: An underdiagnosed hereditary connective tissue disorder with mucocutaneous, articular, and systemic manifestations. ISRN Dermatol. 2012;2012: 751768.
- Whitaker JK, Alexander P, Chau DY, Tint NL. Severe conjunctivochalasis in association with classic type Ehlers-Danlos syndrome. BMC Ophthalmol. 2012;12:47. Copyright ©2012 Whitaker et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License(creativecommons.org/ licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Reinstein E, DeLozier CD, Simon Z, Bannykh S, Rimoin DL, Curry CJ. Ehlers-Danlos syndrome type VIII is clinically heterogeneous disorder associated primarily with periodontal disease, and variable connective tissue features. Eur J Hum Genet. 2013;21:233–236.
- Murray B, Yashar BM, Uhlmann WR, Clauw DJ, Petty EM. Ehlers-Danlos syndrome hypermobility type: A characterization of the patients’ lived experience. Am J Med Genet A. 2013;161A:2981–2988.
- Ferré FC, Frank M, Gogly B, et al. Oral phenotype and scoring of vascular Ehlers-Danlos syndrome: a case-control study. BMJ Open. 2012;2:e000705.
- Klingberg G, Hagberg C, Noren JG, Nietzsche S. Aspects on dental hard tissues in primary teeth from patients with Ehlers-Danlos syndrome. Int J Ped Dent. 2009;19:282–290.
- Rahman N, Dunstan M, Teare MD, et al. Ehlers-Danlos syndrome with severe early-onset periodontal disease (EDS-VIII) is a distinct, heterogeneous disorder with one predisposition gene at chromosome 12p13. Am J Hum Genet. 2003;73:198–204.
- Letourneau Y, Perusse R, Buithieu H. Oral manifestations of Ehlers-Danlos syndrome. J Can Dent Assoc. 2001;67:330–334.
- Genetics Home Reference. Ehlers-Danlos Syndrome. Available at: ghr.nlm.nih.gov/condition/ehlers-danlos-syndrome. Accessed November 3, 2016.
- National Health Service United Kingdom. Ehlers-Danlos Syndrome. Available at: nhs.uk/Conditions/ ehlers-danlos-syndrome/Pages/Introduction. aspx#types. Accessed November 3, 2016.
- Pepin M, Schwarze U, Superti-Furga A, Byers P. Clinical and genetic features of Ehlers-Danlos Syndrome type IV, the vascular type. N Engl J Med. 2000;342:673–680.
- Voermans N, Knoop H, Gleijenberg G, van Engelen B. Pain in Ehlers-Danlos syndrome is common, severe, and associated with functional impairment. J Pain Symptom Manage. 2010;40:370–378.
- Knight I. The role of narrative medicine in the management of joint hypermobility syndrome/Ehlers-Danlos Syndrome, hypermobility type. Am J Med Genet C Semin Med Genet. 2015;169C:123–129.
- Sinibaldi L, Ursini G, Castori M. Psychopathological manifestations of joint hypermobility and joint hypermobility syndrome/Ehlers-Danlos syndrome, hypermobility type: The link between connective tissue and psychological distress revised. Am J Med Genet C Semin Med Genet. 2015;169C:97–106.
- Ferré FC, Frank M, Gogly B, et al. Oral phenotype and scoring of vascular Ehlers-Danlos syndrome: a case-control study. BMJ Open. 2012;2:e000705. Copyright ©2012, Published by the BMJ Publishing Group Limited. For permission to use (where not already granted under a licence) go to group.bmj.com/group/rights-licensing/permissions. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-commercial License, which permits use, distribution, and reproduction in any medium, provided the original work is properly cited, the use is non commercial and is otherwise in compliance with the license. See: creativecommons.org/licenses/by-nc/2.0/ and creativecommons.org/licenses/by-nc/2.0/legalcode.
- National Institute of Dental and Craniofacial Research. Less Is Often Best in Treating TMJ Disorders. Available at: nidcr.nih.gov/OralHealth/ Topics/TMJ/LessisBest.htm. Accessed November 3, 2016.
From Dimensions of Dental Hygiene. December 2016;14(12):40–43.