 FATCAMERA/E+/GETTY IMAGES PLUS
FATCAMERA/E+/GETTY IMAGES PLUS
Strategies for the Prevention of Dental Caries
Dental hygienists are uniquely positioned to provide care and early intervention strategies to reduce dental caries.
Early childhood caries (ECC) is the presence of one or more decayed, missing, or filled (dmf) surfaces in any primary tooth of a child up to age 6. ECC continues to be the most common chronic disease in children, occurring five times to eight times more frequently than asthma.1–3
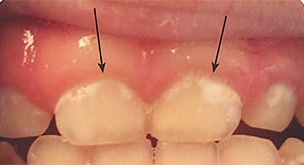
Severe ECC (S-ECC) is defined as any sign of smooth-surface caries in children younger than age 3. Additionally, in children ages 3 through 5, one or more dmf surfaces in primary maxillary anterior teeth, or a dmf score of ≥ 4 (age 3), ≥ 5 (age 4), or ≥ 6 (age 5) surfaces also constitutes S-ECC.3 The typical early sign of ECC is the crescent shaped white spot lesion at the gingival margin (Figure 1 to Figure 4).
ECC is a multifactorial disease with etiological factors being enamel hypoplasia, elevated levels of cariogenic bacteria, and the metabolism of fermentable carbohydrates, which produce acid to demineralize teeth.3 Furthermore, statistics reveal that socioeconomic status is the prevalent factor regarding ECC.4 While race, culture, ethnicity, lifestyle, diet, and oral hygiene practices play a significant role, socioeconomic status outweighs all these factors.4 In developed countries, the ECC rate is 1% to 12%, while in underdeveloped countries, the rate can be as high as 70%.4 Little knowledge on the use of fluoride, poor dietary habits, and a lack of understanding for preventive care for children by parents are correlated strongly with low socioeconomic status.5

The bacteria most often associated with ECC are mutans streptococci (MS). MS metabolize sugars to produce copious amounts of acid, lowering the pH of oral plaque. Low pH for an extended period results in a higher rate of enamel demineralization resulting in caries. A longer period of MS colonization is associated with the likelihood of caries formation. Colonization often begins with a transmission to a child from a primary caregiver, usually the mother. MS colonization is more likely to occur in a child frequently exposed to sugar or a caregiver’s saliva. Low socioeconomic status, high levels of MS in a caregiver, and frequent snacking increases the chance of MS colonization in children. MS transmission may also occur because of encounters with other family members or children in daycare centers or school.6
According to the Agency for Healthcare Research and Quality sponsored United States Medical Expenditures Panel Survey, the average dental expense in 2004 for children younger than 6 was $186 per child.7 The total cost associated with care is estimated at slightly more than $1 billion annually.7 Treating ECC often requires extensive restorative treatment or the extraction of primary teeth. In addition to the expenses of dental restorations, general anesthesia or sedation may be required if children lack the ability to cope with dental procedures. General anesthesia to facilitate dental treatment may add anywhere between $1,500 and $6,000 to the cost of dental care.8 ECC also may contribute to other health problems, such as weight loss, however, the evidence for this is inconsistent.9 Sadly, ECC continues to be the most common chronic disease in children.10

PREVENTION
Strategies continue to evolve to combat this invasive disease. Primarily, the dental hygienist is the key player in prevention. Use of motivational interviewing (MI) and collaboration with other health care providers can create a patient-centered approach to treatment. Other strategies, such as fluoride therapy, including silver diamine fluoride; proper self-care; nutritional evaluation; risk assessment; reduction of MS; and restorative interventions, if necessary; are all part of an effective ECC prevention program.
Dental hygienists are uniquely positioned to reduce the incidence of ECC via prevention. Strategies in education, including behavioral changes and nutritional counseling, position the dental hygienist perfectly in the profession’s prevention role. Furthermore, interventions, including fluoride usage, monitoring, and referral, are well within the dental hygiene scope of practice. Engaging dental hygienists in collaborative care with other health care professionals and utilizing MI while assessing and strategizing a treatment plan are important aspects of dental hygiene practice.

EDUCATION
Dental hygienists are educators at the core. In addition to preventive strategies, teaching methodologies need to be refined to produce behavioral modifications. MI is one such methodology. Colvara et al11 assessed the effectiveness of MI in prevention of ECC. Results showed MI was more effective in reducing ECC than conventional oral health education.11 MI is based on the premise that individuals make behavioral changes on their own by taking responsibility for those changes.
Educational interventions are critical to encourage behavioral change to reduce ECC. Unfortunately, high-quality interventions are lacking. A MI theory called the self-determination theory (SDT) further utilizes motivational strategies. SDT is a psychoeducational intervention, which capitalizes on meaningful, autonomous, and supportive motivation.12
When using motivation for behavioral changes, the individual will perceive the information as his or her own, thus adopting changes/strategies. Methods using MI reduced ECC by 60% compared to the control group.11 SDT methods showed an increase in knowledge and behavioral changes at P < .001.12 Treatment, nutritional counseling, and education on disease can be enhanced using MI.11
CLINICAL INTERVENTIONS
Previously, ECC approaches to treatment have been surgical and restorative, with less emphasis on prevention and management of the disease. Cost of these procedures are prohibitive, with the public sustaining the expense as many patients are covered by the Children’s Health Insurance Program/Medicaid.7 Prevention programs need to focus on stopping the disease process and pattern.
The principal approaches to prevent or reduce ECC in high-risk children include altering dietary patterns and implementing fluoride protocols. Nutritional counseling aims to help parents change their children’s dietary behaviors to favor low or noncariogenic snacks, increase use of community fluoridated water, and limit sweet foods to mealtimes. Such recommendations must be realistic and based on the dietary behaviors of the family. Evidence shows that nutritional counseling can be effective for families at high caries risk. Two landmark studies show that nutritional counseling and reinforcement resulted in reduced caries incidence.13,14 Use of water instead of juices, especially in bottles or sippy cups, and avoiding frequent consumption of fermentable carbohydrates should be encouraged. Limiting on-demand breastfeeding after the eruption of the first tooth and after dietary carbohydrates are introduced, and weaning from bottle use after 12 months are recommended.3
Additionally, oral hygiene must begin before the first tooth even appears. Training pediatricians and family physicians in ECC prevention should be highly encouraged. According to the American Academy of Pediatrics and the American Academy of Pediatric Dentistry (AAPD), the first dental visit should occur at age 1.15,16 This is a baseline screening visit for early ECC identification and to implement early intervention strategies.
A pediatrician, nurse practitioner, obstetrician, or family physician see the child and parent/caregiver much earlier than a dental professional and for many more visits. Currently, 46 states reimburse medical primary care providers through Medicaid for an oral health preventive visit.17 Boylston-Herndon et al17 studied the effects of training pediatricians and family physicians in oral health. Results showed that more oral health screenings and caries risk assessments were conducted and more patients received fluoride varnish in these practice settings. Preliminary results found a positive correlation between increased education and recognition, referral and reduction of ECC.17 Collaboration between providers in medicine and dentistry will most likely help in reducing ECC.18
FLUORIDE THERAPIES
Fluoride is the first line of defense in the prevention of ECC. The US Food and Drug Administration (FDA) recognizes fluoride as the only compound that prevents dental caries.19 In the US, community fluoridated water, toothpastes, and mouthrinses are the primary sources of fluoride.19 Other sources include office gels, varnishes, and silver diamine fluoride (SDF).
Fluoride in low levels inhibits enamel demineralization and enhances remineralization. It inhibits dental caries by changing the metabolism of the bacteria that cause caries. Higher levels of fluoride produce a temporary layer of calcium fluoride on enamel. When the pH drops below 5.5 in response to an acidogenic environment, fluoride is released and becomes available.20 Over-the-counter fluoride toothpaste used twice daily is recommended. For children at high risk, prescription fluorides are recommended.
Recently, the AAPD adjusted the recommended amount of fluoride in community water fluoridation.20 In the 1940s, fluoride in the drinking water was the only available source.20 Recommendations were set regionally because in warmer areas, children drank more water, while in colder temperatures, children drank less water. Ranges varied by climate from 0.7 ppm to 1.2 ppm.19 Today, water is just one of many sources of fluoride and children in all regions of the US consume similar amounts of water, thus the recommended dose of fluoride in drinking water was reduced to 0.7 ppm.19,20
Fluoride supplements are also effective in reducing caries and should be utilized for children deemed high risk. Fluoride supplements are recommended for those who drink fluoride-deficient water (less than 0.6 ppm) and whose diets do not contain fluoride.21 Dietary intake of fluoride can include drinking water at home or daycare/school, sodas, juices, formula and formula that requires adding water, food, and toothpastes.20 Prior to the 0.7 ppm change, there were concerns regarding increased risk of fluorosis, especially with infants consuming formula.22
While professionally applied topical gels—such as 1.23 % acidulated phosphate fluoride (APF, 12,300 ppm)—are efficacious, the popularity and widespread use of 5% sodium fluoride (NaF, 22,500 ppm ) varnishes have made them the product of choice among children in recent years. Their ease of use, reduced risk of ingestion, and no need for a completely dry field make varnish a great choice for children.
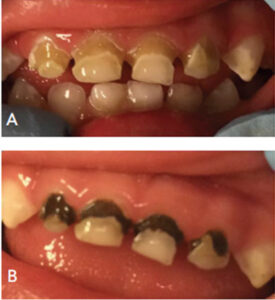
diamine fluoride. B. Arrested caries after the
application of silver diamine fluoride. FIGURE 4. COURTESY LARRY BURNETT, DDS; FIGURE 5. COURTESY NORMAN TINANOFF, DDS, MS
Although not approved for caries prevention by the FDA, the American Dental Association (ADA), has recommend fluoride varnish for caries prevention in young patients who are at moderate to high risk.19 The dental community therefore, uses fluoride varnish as “off label efficacy” because of its success in community-based programs. For example, a Kentucky program that used fluoride varnish with 6,000 elementary school students reduced caries incidence from 50% to 11% over 5 years.23 In fact, varnish is used and recommended for children younger than 6.24 Using varnish on white spot lesions— the cardinal first sign of decalcification—has been an important strategy to control ECC.
SDF (5%, 44,800 ppm) has been approved by the FDA to treat dentinal hypersensitivity. Since 2015, however, it’s been used as “off label” for caries cessation.25 A meta-analysis of existing data found that the percentage of caries arrested over 1 year using SDF was 1.66 times more effective than fluoride varnish or atraumatic restorative techniques.26
SDF is a colorless alkaline solution of silver, ammonium, and fluoride ions in a mixed heavy metal halide complex. Silver compounds and fluoride have been used extensively in caries arrest and prevention. Thus, the combination of the two provide a safe, effective caries preventive agent.27 The use of 38% SDF solution is recommended for caries arrest.25,28 Easily applied, noninvasive, affordable, and safe, SDF provides immediate arrest of the lesion. SDF is proving to be an important therapy in nonsurgical management of ECC (Figure 5).25
SELF-CARE THERAPIES
Twice-a-day toothbrushing is essential in controlling ECC, and guidelines for toothpaste use have been updated. Previously, fluoride toothpaste was not recommended for infants. However, in 2014, the recommendation changed to twice-daily brushing with fluoride toothpaste for all children in optimally-fluoridated and fluoride-deficient communities. Risk vs benefit is the key issue in preventing dental disease over mild fluorosis occurrences. The AAPD recommendation is now a smear or rice-sized amount for children younger than age 3 (0.1 mg fluoride) and a pea-sized amount for children ages 3 to 6 (0.25 mg fluoride) (Figure 6).3,29 For children at high risk of caries, prescription home-fluoride use should be recommended. Fluoride concentrations from 900 ppm to 5,000 ppm are suggested.

CONCLUSION
Early childhood caries is a complex, multifactorial disease and continues to be the most common chronic disease of childhood. Dental professionals must carefully assess the risk factors of not only the infant/child, but the parent/caregiver and create a workable treatment plan that includes the parent/ caregiver in decision making. Dental hygienists are an integral part of the health care team and are in a unique position to provide care and early intervention strategies.
REFERENCES
- Fass, EN. Is bottle-feeding of milk a factor in dental caries? J Dent Child. 1962;24:245–251.
- Tinanoff N. Introduction to the Early Childhood Caries Conference: Initial description and current understanding. Community Dent Oral Epidemiol. 1998;26 (Suppl 1):5–7.
- American Academy of Pediatric Dentistry. Policy on Early Childhood Caries: Classifications, Consequences, and Preventive Strategies, 2016. Available at: .aapd.org/media/policies_guidelines/p_eccclassifications.pdf. Accessed February 26, 2019.
- Anil S, Anand PS. Early childhood caries: prevalence, risk factors, and prevention. Front Pediatr. 2017;5:1–7.
- Wahyu AW, Retno I, Retno PR. Socioeconomic characteristics of the parents and the risk prediction of early childhood caries. Madj Persat Dokt Gigi Indone. 2017;50:23–27.
- Tinanoff, N, Kanellis, MJ, Vargas CM. Current understanding of the epidemiology, mechanisms, and prevention of dental caries in preschool children. Pediatr Dent. 2002;24:543–551.
- Manski RJ Brown E. Dental use, expenses, private dental coverage, and changes, 1996 and 2004. Available at: meps.ahrq.gov/mepsweb/data_files/publications/cb17/cb17.pdf. Accessed February 26, 2019.
- Griffin SO, Gooch BR, Beltran E, et al. Dental services, costs, and factors associated with hospitalization for Medicaid-eligible children, Louisiana 1996–1967. J Pub Health Dent. 2000;60:21–27.
- Thomas CW, Primosch RE. Changes in incremental weight and well-being of children with rampant caries following complete dental rehabilitation. Pediatr Dent. 2002;24:109–113.
- Manski MC, Tinanoff N. Intervention in early childhood caries. Dimensions of Dental Hygiene. 2010;8(5):28–34.
- Colvara BC, Faustino-Silva DD, Meyer E, Hugo FN, Hilgert JB, Celeste RK. Motivational interviewing in preventing early childhood caries in primary healthcare: a community –based randomized cluster trial. J Pediatr. 2018;201:190–195.
- Gasparoni KW, Reeve J, Ghoshe N, et al. An effective psychoeducational intervention for early childhood caries prevention: part 1. Pediatr Dent. 2012;35:241–247.
- Becks H. Rampant dental caries: Prevention and prognosis. A five-year clinical study. J Am Dent Assoc. 1944; 31:1189–1200.
- Krasse B. Approaches to prevention. microbial aspects of dental caries. In: Stiles HM, Loesche WJ, O’Brein TC, eds. Proceedings of “microbial aspects of dental caries” (abstract). Microbiol. 1976;3:867–876.
- American Academy of Pediatric Dentistry Council on Clinical Affairs. Policy on the dental home. Pediatr Dent. 2005-2006;27(7 Suppl):18–19.
- American Academy of Pediatrics. Oral health risk assessment timing and establishment of the dental home. Pediatr Dent. 2003;111(5):1113–1116.
- Boylston Herndon J, Tomar SL, Catalanatto RA. Effect of training pediatricians and family physicians in early childhood caries prevention. J Pediatr. 2015:166:1055-1061.
- Fried JL. Interprofessional collaboration: if not now, when? J Dent Hyg. 2013; 87(Suppl 1):41–44.
- Clifton CM. Focus on fluorides: update on the use of fluoride for the prevention of dental caries. J Evid Base Dent Pract. 204;14S:95–102.
- American Academy of Pediatric Dentistry. Guideline on fluoride therapy. Pediatr Dent. 2014;38:181–184.
- Rozier RG, Adair S, Graham F, et al. Evidence-based clinical recommendation on the prescription of dietary fluoride supplements for caries prevention: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2010;141:1480–1489.
- Hujoel PP, Zina LG, Moimas SAS, Cunha-Cruz J. Infant formula and enamel fluorosis. A systematic review. J Am Dent Assoc. 2009;140:841–854.
- Smith A. Ky. Voices: Clark Co. team leads way to brighter smiles, better futures for Ky kids. Available at: kentucky.com/opinion/op-ed/article44438391.html. Accessed February 26, 2019.
- Weyant RJ, Tracy SL, Anselmo T. Topical fluoride for caries prevention: Executive summary of the updated clinical recommendations and supporting systematic review. J Am Dent Assoc. 2013;144:1279–1291.
- Milgrom P, Horst JA, Ludwig S, et al. Topical silver diamine fluoride for dental caries arrest in preschool children: A randomized controlled trial and microbiological analysis of caries associated microbes and resistance gene expression. J Dent. 2018;68:72–78.
- Crystal YO, Chaffee BW. Silver diamine fluoride is effective in arresting caries lesions on primary teeth. J Evid Base Dent Pract. 2018;18:178–180.
- Zhao, IS, Gao SS, Hiraishi N, et al. Mechanisms of silver diamine fluoride on arresting caries: a literature review. Int J Dent. 2018; 68:67–76.
- Crystal YO, Marghalani AA, Ureles SD, et al. Use of silver diamine fluoride for dental caries management in children and adolescents, including those with special health care needs. Pediatr Dent. 2017;39:135–145.
- American Academy of Pediatric Dentistry. Policy on use of fluoride. Pediatr Dent. 2014;39:49–50.
From Dimensions of Dental Hygiene. March 2019;17(3):45–47.
More on filme xxl!


[…] These rebranding efforts worked to sell kids on Hawaiian Punch (formerly owned by R.J. Reynolds), Kool Aid (formerly owned by Philip Morris), and ultimately contributed to the United States’ high numbers of childhood obesity. And, as oral health professionals know, the effects of Big Soda are seen in the office every day in the form of dental caries. […]