Strategies for Selecting Ultrasonic Inserts / Tips
Improve instrumentation outcomes by using the correct insert/tip for the task at hand.
Many factors are involved in achieving successful debridement with ultrasonic technologies. Both patient- and clinician-centered ingredients are part of the formula for positive outcomes. Patient-centered factors include periodontal status, tolerance, sensitivity, comfort, and preference. Clinician-centered aspects include education, experience, motivation, and equipment choices.
Both magnetostrictive and piezoelectric inserts/tips oscillate with an elliptical pattern, and this motion depends on power setting and probe shape/design.1 Long and thin ultrasonic inserts/tips (UITs) are prone to greater elliptical motion, particularly at high power levels.1 Thus, it is not the type of generator used that is most important in optimal debridement.
One of the key factors in ultrasonic debridement is that the UIT reaches and adapts to the plaque biofilm or calculus location on the root. In addition, choosing the right UIT for the function needed, such as tenacious, burnished, or light deposit removal, is paramount. Think about UIT designs based on appearance and patterns, as with hand-activated instruments. Each end has similar characteristics, such as a contour, shank diameter (wide, thin, thinnest), and shank length (short, long, and longest).
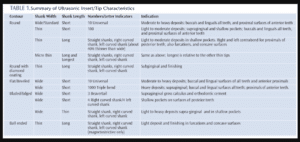
UIT contour can be round and smooth, round with diamond coating, flat, or bladed. Roundness allows easy application of all working sides and ease of insertion subgingivally. In contrast, flat profiles—adapted to the tooth on the flat surfaces—are ideal for gross calculus deposits, stain, and supragingival orthodontic cement removal. Likewise, the bladed silhouettes, most often associated with piezoelectric units, are indicated for supragingival use and subgingival endoscopic visualization, and require that the blade/edge be adapted to the deposit.
Tip diameter is categorized as wide, thin, and thinnest (micro). Wide UITs are indicated for supragingival debridement and stain removal, while thin UITs are used for subgingival applications (a thin UIT is shown in the cover photo). Also, wide tips are best for large or tenacious deposits, while thin tips are well suited for fine accumulates. There is concern regarding the influence of thin UITs on attachment loss. Casarin et al2 found that a thin UIT induced a greater immediate clinical attachment loss than a standard tip; however, this finding did not affect clinical outcomes. Patient comfort also is enhanced with thin UITs. A significant difference in patient preference was evident when a standard and thin UIT were compared.3 Reductions in plaque and bleeding indices were noted with both designs; however, the thin UITs produced significantly less patient discomfort.3
Shank length also is important. The longest shanks are intended to adapt in deep pockets. Typically, thin and long UITs are used at low to moderate power (amplitude), and wide, large ones are used on moderate to moderately high power. There are newly manufactured UITs, however, that are thin, long, and recommended for use with moderate to heavy calculus on moderately high power levels.
APPLICATIONS
Once clinicians have a full complement of UITs, the interpretation of assessment data is vital. Sulcus, shallow or deep pocket depth, taut or elastic tissue tone, and type and location of deposits should all be considered.
The most commonly used UITs are those with rounded contours, and they are available in both piezoelectric and magnetostrictive technologies. These universal round UITs with straight shanks are for gross supragingival or subgingival debridement in all intraoral locations. The shank width and length aid in determining if straight shanks are applied above or below the gingival margin. A thin shank microultrasonic rounded silhouette UIT with a straight shank is suitable for light deposit and plaque biofilm on all surfaces in anterior segments and any narrow periodontal pockets. This UIT is indicated for prophylaxis, periodontal maintenance, and initial periodontal therapy after gross deposit removal.
The addition of round and thin right and left contours is for light deposits and adaptation to proximal surfaces, root contour, and furcations. The option of a ball-ended design might assist in light debridement of furcation areas, particularly in the concave surface adjacent to the roof of the furcation entrance.
Diamond-coated UITs also have a round profile; however, they are saved for removing calculus in deep pockets and furcations. They were initially manufactured for residual deposits best identified and treated with an endoscope or direct vision during surgery. Unfortunately, endoscopic technology is not currently available to all clinicians. These UIT ends are coated with fine-diamond grit; therefore, they are very abrasive. Their adaptation and activation should be gentle and precise, with frequent evaluation of the site with direct vision or an explorer. Straight, right, and left shanks are available. The diamond surface is moved over the deposit and removal occurs from the outer to the inner layer. As such, this UIT is not most active at the terminal end as with other UITs.4 Significant root structure removal within a limited time has been demonstrated, so these UITs should be used with the utmost caution.4
Flat contours originally were designed only for heavy supragingival deposits. The standard universal flat design may include a long shank for moderate to heavy subgingival deposits. The 100 series is a universal design with a flat end and is indicated for all pocket depth and large deposits. Flat designs are intended for large deposits in supragingival or subgingival environments, but not for fine deposit and biofilm debridement. The flat UIT could be used for debridement in prophylaxis or periodontal maintenance and in the beginning stages of instrumentation for nonsurgical periodontal therapy.
Using bladed or edged profiles with piezoelectric units is reserved for heavy and/or burnished residual deposits. Anterior and posterior segments can be treated with the curved design (4 right shank/4 left shank or similar) for proximal surfaces.
The use of ultrasonic therapy for implant maintenance is increasing as more products are developed. Options include varying metal substances, plastic UITs, and soft UITs. Mann et al5 found that metal tips produced defects in titanium implants; however, the amplitude and load used affected this damage. Plastic-coated tips cause minimal damage and polish well, but leave plastic deposits on the surface. The development of less problematic materials for use on implants is needed.5
Braun et al6 found that a novel copper alloy UIT minimally influenced the titanium implant, making this a viable alternative that may provide improved durability and wear. Other researchers also concluded that copper alloy may be used in the maintenance of implant prostheses.7–9 Until these UITs are readily available, a special magnetostrictive insert with a disposable soft tip placed with a wrench device may be helpful. Many piezoelectric tip options for implants are also available.
Another concern with UIT selection is debridement of restorations. Arabaci et al10 found that applying piezoelectric tips to amalgam, porcelain, and composite restorations created roughness, scratches, and nicks. Studies show that roughness influences the establishment of plaque biofilm; therefore, achieving smoothness is important for enamel, root, and restorative surfaces.10 How much this residual roughness contributes to clinical outcomes is undetermined. In general, restorations are contraindicated for ultrasonic instrumentation; however, some UITs designed for implants may be used to debride restorations, such as the insert with a soft tip.
INAPPROPRIATE SELECTION
Improper UIT selection can have negative consequences. Incomplete debridement or burnished residual deposits are just a few of the adverse outcomes. Incomplete debridement occurs when, due to its size and contour, the UIT is unable reach the deposit location. A wide tip intended to reach a deposit located 5 mm subgingivally is not a wise choice. Likewise, a thin tip that is straight instead of curved is not a logical choice for proximal surfaces with deposits at the midline. A micro-thin UIT on low power used to remove tenacious deposits will result in burnishing. The UIT’s surface area and power are not sufficient to fracture the dense accumulation; therefore, undetected smooth, flat deposits remain.
Using the incorrect UIT can also cause discomfort or pain due to lack of adaptability or the need to increase power settings to obtain results. Also, using a wide UIT for subgingival applications vs a thin UIT could result in more root surface removal than necessary. This unintended removal could lead to post-operative sensitivity and/or interfere with long-term healing because the roughness and defects will attract further biofilm accumulation. Choosing the incorrect UIT can also encourage poor working posture when clinicians try to adapt a UIT to the anatomy. Inefficiency and compromised outcomes may also result.
PATIENT SCENARIOS
The use of more than one UIT during debridement is desirable because, in most situations, many needs are present. For example, the use of multiple UITs is necessary to remove heavy tenacious localized supragingival and generalized fine subgingival deposits. For patients with light supragingival deposits who need moderate localized subgingival removal in the posterior sextants, large supragingival designs, large subgingival types, and thin subgingival UITs of varying shapes might be incorporated. For periodontal maintenance, subgingival UITs are indicated with straight, right, and left designs. Depending on pocket depth and tissue tone, straight, right, and left UITs with thin diameter shanks are appropriate. The shank length can be short, long, or longer to reach the epithelial attachment.
Case Study 1. A patient presents with generally healthy gingiva, localized bleeding on probing, and gingival inflammation and 4 mm pocket depth on first molars. Bone loss is not detectable; therefore, gingivitis is present. Deposits are light to moderate and not dense. In addition, the maxillary laterals have been replaced with titanium implants. For prophylaxis, precision thin right, left, and straight UITs will adapt to anterior and posterior teeth, as well as meet the needs of deposit removal and shallow pocket depth. A UIT with a soft tip could be used to debride the implants. Therefore, four UITs are needed for debridement. If the patient had dense moderate to large supragingival deposits in the mandibular anteriors, a standard UIT with a bladed or flat profile would be indicated. Neither a long shank nor a thin diameter UIT is appropriate for the anterior because of the tenacious nature of the deposits.
Case Study 2. A patient presents for initial periodontal therapy with generalized marginal and diffuse inflammation, bleeding on probing, generalized 4 mm to 6 mm pocket depth with mostly normal gingival contour, Class II molar furcations with a few adjacent to recession, and moderate to heavy tenacious deposits located marginally and subgingivally. Severe and moderate bone loss is revealed on radiographs. Initial debridement could be accomplished with a standard universal UIT. A precision thin UIT could easily cause burnishing at this stage of the debridement process. Next, a thin universal UIT indicated for moderate to heavy deposits used on moderately high power, not low power, could follow. Right, left, and straight UITs indicated for heavy deposits are another option, instead of a single universal. After determining the deposits have been fractured to small, fine pieces, micro-thin, long-shank UITs are indicated. Therefore, the right, left, and straight profiles are needed to meet the generalized needs of deposit removal, as well as the root anatomy. Ball-ended UITs could be added to finish the furcation areas—particularly where recession is present. At the reevaluation visit, diamond-coated UITs could be used for flat residual deposits discovered through endoscopy.
In both cases, hand instruments should be incorporated intermittently. With the first case, a sickle could be used if calculus is located below the contact area. In the second case, periodontal files might be incorporated at the beginning of the process and/or after initial debridement to fracture deposits and prevent burnishing. Hand-activated curets would also be appropriate for definitive calculus removal in the root contours where ultrasonic instrumentation is not as effective as the use of curved, bladed instruments.
*click to view
CONCLUSION
Successful debridement with ultrasonic therapy relies on many factors; however, an initial step is proper UIT selection. With a plethora of new designs available, clinicians should examine the profile prior to selection for therapy. There are many buying options, and it is best to visit manufacturers’ websites to review availability.
Many advances have been made in nonsurgical therapy, with UIT design being one. However, only one randomized controlled trial on UIT design has been conducted.11 Efforts are being made to enhance clinical results, patient-centered outcomes, and cost-effectiveness of nonsurgical periodontal therapy.11 One facet of this mission is to develop better UITs. More randomized controlled trials are needed to study UIT design, as well as ultrasonic systems. No longer are hand instruments and a single UIT the norm. Instead, multiple UITs and hand-activated instruments should be interwoven into debridement therapy.
REFERENCES
- Lea SC, Felver B, Landini G, Walmsley AD. Three-dimensional analyses of ultrasonic scaler oscillations. J Clin Periodontol. 2009;36:44–50.
- Casarin RC, Bittencourt S, Ribeiro Edel P, et al. Influence of immediate attachment loss during instrumentation employing thin ultrasonic tips on clinical response to nonsurgical periodontal therapy. Quintessence Int. 2010;41:249–256.
- Nardi GM, Di Giorgio R, Sabatini S. Effectiveness of tips for delicate micro-ultrasonic root planing compared to tips for traditional ultrasonic root planing. Ann Stomatol (Roma). 2012;3:90–94.
- Harrel SK. From diamonds to transducers. Dimensions of Dental Hygiene. 2008;6(10):36.
- Mann M, Parmar D, Walmsley AD, Lea SC. Effect of plastic-covered ultrasonic scalers on titanium implant surfaces. Clin Oral Impl Res. 2012;23:76–82.
- Braun A, Jepsen S, Krause F. Subjective intensity of pain during ultrasonic supragingival calculus removal. J Clin Periodontol. 2007;34:668–672.
- Baek SH, Shon WJ, Bae KS, Kum KY, Lee WC, Park YS. Evaluation of the safety and efficacy of novel metallic ultrasonic scaler tip on titanium surfaces. Clin Oral Implants Res. 2012;23:1269–1274.
- Seol HW, Heo SJ, Koak JY, Kim SK, Baek SH, Lee SY. Surface alterations of several dental materials by a novel ultrasonic scaler tip. Int J Oral Maxillofac Implants. 2012;27:801–810.
- Lee AR, Chung CH, Jung GU, Pang EK. The effect of copper alloy scaler tip on the surface roughness of dental implant and restorative materials. J Korean Acad Prosthodont. 2014;52:177–185.
- Arabaci T, Cicek Y, Ozgoz, Canakci V, Canakci CF, Eltas A. The comparison of the effects of three types of piezoelectric ultrasonic tips and air polishing system on the filling materials: an in vitro study. Int J Dent Hyg. 2007;5:205–210.
- Sanz I, Alonso B, Carasol M, Herrera D, Sanz M. Nonsurgical treatment of periodontitis. J Evid Based Dent Pract. 2012:12:76–86.
From Dimensions of Dental Hygiene. October 2014;12(10):26,28,30–31.

