 STOCKBYTE / THINKSTOCK
STOCKBYTE / THINKSTOCK
Sedation of the Pediatric Patient
The use of sedation and general anesthesia may make the treatment of children who cannot tolerate dental care possible.
This course was published in the March 2016 issue and expires March 31, 2019. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Define the continuum of sedation and anesthesia.
- Identify the methods used to provide sedation and general anesthesia.
- Discuss the clinical guidelines for administering sedation and anesthesia.
- STOCKBYTE / THINKSTOCKList the most common agents used to achieve sedation.
Some patients, particularly children, may require sedation in order to undergo dental treatment.1 The goals of sedation include patient comfort and reduced anxiety, and it may also facilitate the provision of high-quality dental care and encourage a positive view of dental treatment.2,3 While sedation may only be administered by a specially trained dentist, nurse, or physician, dental hygienists should be prepared to help manage complications or emergencies.
The administration of sedation and general anesthesia is a continuous spectrum of nervous system depression. At one end of the spectrum is local anesthesia provided to a fully conscious patient in which sensory impulses are blocked peripherally. At the other extreme is general anesthesia. In between are varying levels of sedation, which are classified by level of consciousness, response to command, airway patency, ventilation, and cardiovascular function. For dental procedures, local anesthesia is usually combined with sedation and is often used even if general anesthesia is planned.
Minimal sedation. Patients respond normally to verbal commands during this drug-induced state. Although cognitive function and coordination may be impaired, ventilatory and cardiovascular functions are unaffected.4–6
Moderate sedation. During this drug-induced depression of consciousness, patients respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation. The medications and techniques used should carry a margin of safety wide enough to make unintended loss of consciousness unlikely. No interventions are required to maintain a patent airway, and spontaneous ventilation is adequate. Cardiovascular function is usually maintained.4–6 Purposeful response varies according to the patient’s chronological and developmental age. For example, older patients may respond to “squeeze my hand,” whereas younger children may only cry at times. What is not considered purposeful, however, is reflex withdrawal from a painful stimulus without any other reaction.5
Deep sedation. Patients cannot be easily aroused but respond purposefully following repeated or painful stimulations during this drug-induced depression of consciousness. The ability to independently maintain ventilatory function may be impaired. Patients may require assistance in maintaining a patent airway, and physiological ventilation may be inadequate. Cardiovascular function is usually normal.4–6
General anesthesia. During this drug-induced loss of consciousness, patients are not arousable, even by painful stimulation. The ability to independently maintain ventilatory functions is often impaired. Patients frequently require assistance in maintaining a patent airway, and positive pressure ventilation may be required because of depressed spontaneous ventilation or drug-induced depression of neuromuscular function. Cardiovascular function may be impaired.4–6
MODES OF SEDATION
There are numerous methods in which to administer medications to produce sedation and anesthesia, and some drugs are capable of routinely achieving and sustaining any level along the continuum. Routes of drug administration are generally categorized as enteral or parenteral. Enteral refers to administration via the gastrointestinal tract, and consists of oral and rectal routes. Parenteral routes involve the direct delivery of the drug into the systemic circulation and do not involve the gastrointestinal tract. These include injections into veins (intravenous, or IV), muscles (intramuscular, or IM), tissues between the skin and muscles (subcutaneous), intranasally, or via other routes such as into bone marrow (intraosseous). The parenteral route also comprises drugs that are absorbed into the vasculature after being inhaled. For sedation and anesthesia to occur, a medication must ultimately access the systemic circulation and eventually pass from the blood to the main site of action—the brain.
The oral route is the most common, and is often the most acceptable to patients. It is convenient, noninvasive, and economical. Medications taken orally are subject to metabolism in the gut and liver before reaching the systemic circulation. This is known as first-pass metabolism, and it means that less of the drug reaches the circulation than is consumed, and there is a lag time between administration and action. Furthermore, the amount of medication actually absorbed varies between individuals, and food and other medications can interact to either increase or decrease the availability of the drug to the systemic circulation.7 Because a drug’s influence is difficult to foresee, the lowest effective dose should be administered and adequate time allowed after dosing, so drug effects and any relevant side effects can be observed.8
The IV route is also a common pathway for drug administration. Medications given in this manner avoid first-pass hepatic metabolism, and action can be rapid. Pharmacological effects are simple to predict in terms of onset, maximum effect, and duration, which enhances the ability to titrate the drug. Titration refers to administering small doses of a drug incrementally until the desired effect is produced.7 It allows for a more individualized approach to sedation, and may also increase safety and effectiveness. However, IV medications are subject to drug interactions during metabolism that may decrease or prolong a drug’s action. The IV route is invasive, may be painful, and requires extra training on the part of the practitioner.
The IM route is frequently used in sedation and general anesthesia. In pediatric patients, the medication is generally injected into the thigh (vastus lateralis) or shoulder (deltoid) muscles. First-pass metabolism is avoided, and the drug is absorbed into the vasculature in a fairly predictable and uniform manner. Onset of action is less rapid than IV injection, and the absorption is spread out, so the duration of action tends to be longer.7 The IM route may require less technical skill on the part of the practitioner than IV cannulation. This route can be painful and locally irritating, thus, only a certain volume of medication can be injected at each site depending on the size of the musculature. It is not advisable to attempt titration via the IM route and some drugs are inappropriate for IM injection.
The inhalation mode depends on absorption of the gas into the vasculature of the respiratory system. First-pass metabolism is avoided, and onset is rapid. As gases are minimally metabolized in general, the cessation of action occurs by redistribution of the gases out of the blood and into the lungs for exhalation.9 When delivered by nasal hood or facemask, the administration of gases by inhalation can be diluted if the equipment is poorly fitting or if the patient will not tolerate it.9 During general anesthesia, gases are typically delivered more directly to the lungs via an endotracheal tube or supraglottic device.
CLINICAL GUIDELINES
As the popularity of office-based sedation and general anesthesia increases, so too do instances of tragic outcomes. Children are particularly vulnerable to sedative depressant effects on airway patency, protective reflexes, and respiratory effort.5 Respiratory distress can quickly lead to cardiac problems. The key to minimizing such risks is careful and thorough preparation—of the equipment, by the sedation team, and by the patient.
For any level of sedation, preparation begins with a complete patient evaluation, comprising age and weight, allergies, and medication usage; past medical history including surgeries/anesthesia; family medical history; baseline vital signs; physical examination focused on the heart, lungs, and airway; and appropriate consultations with primary care and specialist physicians based on the patient’s underlying medical conditions. Such evaluation will help determine whether the patient is a suitable candidate for sedation. The American Society of Anesthesiologists created a useful tool for categorizing patient risk according to physical status (Table 1).10 In the case of office-based sedation for children, patients in classes I and II are generally considered appropriate candidates. Class III patients require additional medical consultation and improvement of health prior to considering sedation.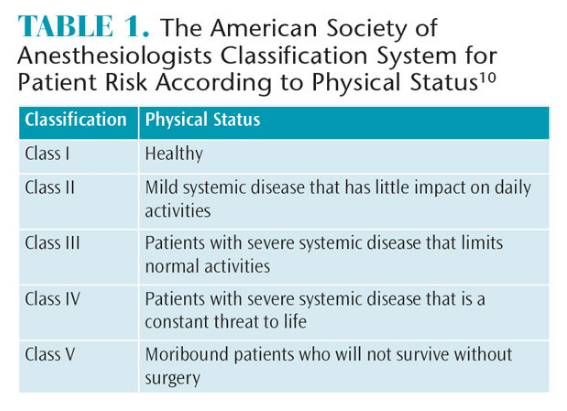
Diet is an important aspect of pre-sedation preparation. Sedative medications have the potential to impede protective airway reflexes, especially as the patient moves deeper into the anesthesia continuum. For example, if a child vomits and is unable to protect his or her airway, the vomitus can easily be aspirated into the lungs. This is a potentially serious complication that can kill or require prolonged hospitalization. To help minimize this risk, certain dietary guidelines should be followed to prevent patients from presenting for sedation with full stomachs. For healthy patients, the recommendations for minimum time before sedation are as follows: clear liquids are acceptable up to 2 hours before sedation; breast milk, 4 hours; formula and cow’s milk, 6 hours; and solid food, 8 hours.5
The dental office must be appropriately prepared for emergencies. The necessary equipment and personnel for resuscitating or maintaining an unconscious patient must be readily available. This includes size-appropriate tools for managing the airway, IV catheters and fluids, suction devices, and rescue medications. An oxygen delivery system capable of positive pressure ventilation and an automated external defibrillator must always be available.5 An emergency protocol should be in place and periodically practiced within the office. During an adverse event, the sedation team is responsible for stabilizing the patient until emergency medical help arrives.
The majority of emergencies in healthy children undergoing sedation are airway-related. When a patient is sedated, the muscles responsible for maintaining airway tone relax, and the soft tissues surrounding the airway can collapse, thereby causing airway obstruction. Children are more susceptible than are adults. Airway obstruction can often be treated by providing a chin lift or a mandible thrust while administering supplemental oxygen. If ineffectual, an airway adjunct can be promptly placed either orally or nasally to splint open the airway. In pure airway obstruction, the patient will continue to make respiratory effort but needs help opening the airways to allow airflow. In this way, airway obstruction is distinct from respiratory depression. The latter occurs as a result of medication effects on the respiratory drive. Simply opening the airway will not treat respiratory depression; rather, if a patient is not ventilating adequately, the provider must breathe for the patient. This is where positive pressure ventilation becomes especially relevant. Often, positive pressure ventilation is provided by a facemask attached to a self-inflating bag via a one-way valve connected to an oxygen source.11 The provider then squeezes the bag to produce ventilation. Obstruction and respiratory depression can occur together, so if positive pressure ventilation is required, it is wise to concurrently open the airway. If the patient still cannot be ventilated, more advanced airway management is required in the form of a supraglottic device or endotracheal tube. While changes to ventilation and airway patency rarely occur during minimal or moderate sedation, patients can easily slip into more profound levels of sedation than anticipated. Furthermore, airway obstruction can occur as the patient relaxes or if the patient’s posture changes, including the position of the mandible.8 Providers must be able to manage patients who move beyond the anticipated level of sedation.
During the sedation period, the patient’s physiological condition must constantly be observed. For example, patients under moderate sedation should have their oxygen saturation, heart rate, response to sedation, respiratory rate, and blood pressure closely monitored. During deep sedation or general anesthesia, a continuous measurement of exhaled carbon dioxide levels, heart function via electrocardiogram (EKG), and core body temperature is required.4–6 Changes in exhaled carbon dioxide can signal respiratory compromise before a pulse oximeter can. Therefore, its use is also encouraged during moderate sedation. Similarly, EKG monitoring is helpful when treating patients with cardiovascular disease. All vitals should be documented in a time-oriented sedation record, which should also include the names, routes, dosages, and administration times of all medications used, including oxygen and inhaled agents.4–6
Once the dental procedure is completed, the patient enters a period of recovery. The recovery area requires immediate access to equipment for positive pressure ventilation and suction. Blood pressure, heart rate, oxygenation, and level of consciousness should be continually monitored until the patient has met the criteria for discharge. At discharge, the patient should be awake and back to the pre-sedation level of cognition and activity. Cardiopulmonary function should be at baseline, and airway patency should be well-maintained.4–6 Post-operative pain, nausea and vomiting, and bleeding need to be controlled.6 Post-sedation or general anesthesia patients must be accompanied by a responsible third party.
COMMON SEDATIVE AGENTS
Numerous medications are available for dental sedation. The difference between the choice of drugs is generally the result of pre-treatment considerations regarding duration of drug action, potential side effects, and clinician preferences.
Sedatives may decrease fear and anxiety, but they do not diminish pain. Adequate local anesthesia is still an integral part of the dental plan when using sedation. As local anesthetics are nervous system depressants, they can potentiate the sedative and respiratory depressant actions provided by sedation medications. This can have catastrophic consequences for pediatric patients undergoing dental sedation. Thus, dosages of local anesthetics must be kept below the maximums recommended.
Chloral hydrate is a central nervous system (CNS) depressant that was historically popular for pediatric sedation. Because chloral hydrate has many adverse effects and is no longer commercially available as a prepared drug, benzodiazepines have widely supplanted it as the agents of choice for pediatric sedation. They have a high therapeutic index, meaning there is a large margin of safety between the effective dose and the toxic dose. Benzodiazepines work by potentiating the action of the inhibitory neurotransmitter, gamma-aminobutyric acid (GABA).12,13 They produce anxiolytic, hypnotic, muscle relaxant, and amnesic effects. Unfortunately, benzodiazepines occasionally cause increased activity and agitation in children when they are negatively stimulated. At doses used for moderate and deeper sedation, this class of drug can depress respiration, promote airway obstruction, and decrease blood pressure, especially when used in combination with other sedatives or opioids.12 There is also a reversal agent—flumazenil—available for benzodiazepines. Flumazenil antagonizes benzodiazepine action at the GABA receptor, and can be given in the event of an unresponsive patient. It is best administered via the IV route.
Opioids are effective analgesics, making them a useful adjunct when a dental procedure is expected to be particularly painful or stimulating. They are agonists at mu, kappa, and delta receptors in the nervous system, and are similar to substances the body naturally produces.12,14 Opioids also possess somewhat unpredictable sedative actions, and combination with other agents can produce profound sedation. Opioids depress brain respiratory centers and usually lead to a net decrease in ventilation. This respiratory depression may be synergistic when benzodiazepines and opioids are used together. Opioids are considered to be heart-safe secondary to their ability to decrease sympathetic responses; this is beneficial in patients whose cardiovascular systems cannot tolerate the stimulation produced by uncomfortable dental procedures.12 While opioids tend to reduce heart rate, overall, they are thought to produce hemodynamic stability.14 Opioids can provoke nausea and vomiting and should be avoided in patients who are prone to these conditions.15 Like benzodiazepines, there is a reversal agent for opioids. Naloxone antagonizes opioid receptors, effectively undoing opioid actions, and may be given by the IV, IM, or subcutaneous route.
Antihistamines work by antagonizing histamine and acetylcholine receptors, abolishing the excitatory impact these neurotransmitters usually have within the CNS. They are sleep-inducing and have anti-nausea actions, rendering their use helpful in combination with other medications. They are less effective than benzodiazepines when used alone, but they can potentiate the sedative effect of other agents when used in combination. Antihistamines have minimal depressant influence on the respiratory and cardiovascular systems, but they do cause anticholinergic side effects.12
Nitrous oxide is widely used in dental offices to promote relaxation and analgesia. It is a colorless, nonirritating, and mildly sweet-smelling gas. Its onset and conclusion of action are rapid, as nitrous oxide has a low blood and tissue solubility and is not metabolized.9,16 It has minimal effect on physiological parameters. When nitrous oxide is combined with other sedatives or opioids, however, respiratory and/or cardiovascular depression can be synergistically produced.9 Nitrous oxide quickly enters gas-filled spaces, and can cause dangerous increases in volume and pressure when such areas are closed or noncompliant. It is therefore contraindicated in patients with obstructions in spaces like the middle ear or the sinuses.9,16 It can also promote nausea and vomiting. Chronic exposure to nitrous oxide has been linked to reproductive issues, neurological deficits, and blood cell abnormalities. Such risk is minimized by the use of scavenging systems. Short-term use of nitrous oxide in healthy patients appears to be safe.9 Used alone, the gas typically produces minimal to moderate levels of sedation.
Sedative regimens are chosen based on a number of factors, such as age, medical history, and temperament. Surgical factors include the planned length of the procedure and amount of intraoperative and post-operative discomfort anticipated. The pharmacological profile of the various sedative agents is then matched to the patient and treatment plan. As no one medication is ideal, combinations of drugs are often used to achieve desired effects. When combinations are used, the sedative and respiratory depressant actions of each are intensified. Using combinations does, however, allow for lower doses of each individual medication, which can decrease the risk of side effects. In pediatric oral sedation, midazolam, a benzodiazepine; hydroxyzine, an antihistamine; and meperidine, an opioid, are commonly used together. If a longer duration of action is desired, diazepam may be used to replace the midazolam. If a patient is easily nauseated, the opioid may be avoided. In addition to these drugs, the level of sedation can be titrated and operative time may be extended by administering a nitrous oxide/oxygen mix.12
CONCLUSION
Patients present to the dental office with different capacities for coping and compliance, and varying levels of anxiety and medical complexity. In some patients, minimal sedation is adequate, while others may need moderate to deep sedation in order for dental care to be delivered in a secure and compassionate manner.2 Patient well-being and safety are paramount, and every member of the sedation team must be well trained and vigilant to ensure patient safety.
References
- American Academy of Pediatric Dentistry Ad HocCommittee on Sedation and Anesthesia. Policy on the use of deep sedation and general anesthesia in the pediatric dental office. Pediatr Dent.2012;37:86–87.
- American Academy of Pediatric Dentistry ClinicalAffairs Committee, Sedation and General Anesthesia Subcommittee. Guideline on use of anesthesia personnel in the administration of office-baseddeep sedation/general anesthesia to the pediatric dental patient. Pediatr Dent. 2012:37:228–231.
- American Dental Association. Policy Statement:The Use of Sedation and General Anesthesia by Dentists. Available at: ada.org/~/media/ADA/About%20the%20ADA/Files/anesthesia_policy_statement.pdf?la=en. Accessed February 19, 2016.
- American Dental Association. Guidelines for theUse of Sedation and General Anesthesia by Dentists. Available at: ada.org/~/media/ADA/About%20the%20ADA/Files/anesthesia_use_guidelines.ashx.Accessed February 19, 2016.
- American Academy of Pediatrics and theAmerican Academy of Pediatric Dentistry. Guidelines for Monitoring and Management of Pediatric Patients During and After Sedation for Diagnosticand Therapeutic Procedures. Available at: aapd.org/media/policies_guidelines/g_sedation.pdf. Accessed February 19, 2016.
- The American Society of Dentist Anesthesiologists.Parameters of Care. Available at: asdahq.org/ParametersofCare. Accessed February 19, 2016.
- Becker DE. Pharmacokinetic considerations formoderate and deep sedation. Anesth Prog. 2011;58:166–173.
- Donaldson M, Gizzarelli G, Changpong B. OralSedation: A primer on anxiolysis for the adult patient. Anesth Prog. 2007;54:118–129.
- Becker DE, Rosenberg M. Nitrous oxide and theinhalation anesthetics. Anesth Prog. 2008;55:124–131.
- Kramer K, Treasure T, Kates C, Klene C, Bennett J.History and physical evaluation. In: Bosack RC, Lieblich S, eds. Anesthesia Complications in the Dental Office. Ames, Iowa: Wiley Blackwell;2015:9–13.
- Becker DE, Rosenberg M, Phero J. Essentials ofairway management, oxygenation, and ventilation: part 1: basic equipment and devices. Anesth Prog. 2014;61:78–83.
- Becker DE. Pharmacodynamic considerationsfor moderate and deep sedation. Anesth Prog. 2012;59:28–42.
- Struyk BP, Tyler DC, Motoyama EK. Safety andoutcome in pediatric anesthesia. In: Davis PJ, Cladis FP, Motoyama EK, eds. Smith’s Anesthesia for Infants and Children. 8th ed. Philadelphia: ElsevierMosby; 2011:1273–1293.
- Robert RC. Parenteral anesthetic agents. In:Bosack RC, Lieblich S, eds. Anesthesia Complications in the Dental Office. Ames, Iowa: Wiley Blackwell;2015:135–141.
- Becker DE. Adverse drug interactions. Anesth Prog. 2011;58:31–41.
- Kates C, Anderson D, Shamo R, Bosack R.Inhalation anesthetic agents. In: Bosack RC, Lieblich S, eds. Anesthesia Complications in the Dental Office. Ames, Iowa: Wiley Blackwell;2015:143–149.
From Dimensions of Dental Hygiene. March 2016;14(03):48–51.



