An extensive body of research supports the use of sealants in caries prevention, but utilization is still relatively low. The rate of caries among children age 6 years to 19 years has decreased over the past 40 years since sealants first received provisional acceptance by the American Dental Association (ADA). Despite this improvement, 88% of carious lesions still occur in the pits and fissures— surfaces that most benefit from sealant application.1,2
Additional findings show that between 1988 and 1994, only 23% of 8-year-olds in the United States received sealants on their first permanent molars.3 This study also found that during the same time period, only 15% of 14-year-olds received sealants on their second permanent molars.3
To remedy these low usage rates, the US Surgeon General’s Healthy People 2010 report set a goal of increasing sealant usage by 50% for 8-year-olds and 14-year-olds.4 Despite these goals, 25.5% of children age 6 years to 9 years received sealants on their first permanent molars between 1999 and 2004, and 19.9% of teenagers age 13 years to 15 years received sealants on their second permanent molars.4 As such, the new US Surgeon General’s Healthy People 2020 report aims to increase sealant utilization to 28.1% among children age 6 years to 9 years, and 21.9% for teenagers age 13 years to 15 years.5
History of the Technique
Prevention has a long history in dentistry. In 1922, T.P. Hyatt, DDS, introduced the prophylactic odontotomy technique—a precursor to sealants—in which a restoration was placed on the occlusal surface of permanent posterior molars.6 This approach was widely practiced until 1971 when dental sealants were introduced.7,8 In 1976, the ADA recognized the efficacy of sealants,9 and in 1983, the National Institutes of Health declared sealants “a safe and highly effective means of preventing pit and fissure caries.”10
Types of Sealants
The first sealants were activated by ultraviolet light.8 Today, most sealants are photopolymerized using a curing light of which there are three types: light-emitting diode, halogen, and plasmaarc.11 The intensity of the wavelength necessary for curing is between 400 nm and 500 nm. The exposure time varies between 10 seconds and 40 seconds, depending on the light and material utilized.
The depth of cure is dependent upon sealant material selection, intensity of the curing light, and distance of the light from the material. Studies show clear sealants cure faster and pose a deeper depth of cure than opaque sealants.12
Self-cure sealants do not need activation by light. They usually require mixing two components (liquid resin monomer and a catalyst) immediately prior to placement. Once mixed, the setting time is approximately 60 seconds.
Traditionally, sealants were considered unfilled resins, compared to the resin-based composites used for restorations. Some of the sealants used today contain filler, which adds thickness or bulk to the material. Manufacturers usually add filler to allow better wear of the material. Sealants that contain filler particles typically require more time to polymerize. Filled and opaque sealants require an incremental approach to ensure a complete cure.12
Some sealants are made of glass ionomer material, which can be applied in very moist conditions and where isolation is difficult.13 Retention with glass ionomer sealants, however, is usually not as long as traditional sealants. Despite this, glass ionomer sealants are a good choice for application on partially erupted molars.13
Sealants appear clear, tinted, or opaque. One sealant product starts out pink during initial placement and then turns white upon photopolymerization.
In order to promote remineralization of enamel, some sealants contain fluoride.14 There are no long-term data to show that the addition of fluoride improves sealant effectiveness.
The presence of bisphenol A (BPA) in sealants has raised concerns about safety. BPA has been linked to adverse health effects, especially on infant development.15,16 A number of BPA-free sealants are available.15-17 Some sealants are composed of a BPA alternative, derivative bisphenol diglycidyl ether methacrylate (BisGMA). Research shows that BisGMA is stable when polymerized, and does not break down to form BPA.16
Sealant Application
The steps for basic sealant placement are as follows:
- Select the tooth or teeth for sealant application.
- Completely clean the tooth, removing plaque and debris from the enamel surface. Use pumice on a rotary brush/cup or toothbrush. Studies show there is no significant difference in sealant retention following toothbrush prophylaxis when compared to rotary brush/cup prophylaxis.18,19 While the use of fluoride- free paste is considered ideal, no significant difference in sealant retention was noted in studies that used toothpaste with and without fluoride before sealant placement.18,20
- Rinse pumice completely off tooth surfaces.
- Isolate the tooth with cotton rolls, saliva absorbents, tooth isolation system, or rubber dam. A tooth isolation system or rubber dam should be placed prior to cleaning the tooth (step two).
- Dry the tooth and apply acid etch liquid/gel or self-etch adhesive liquid per manufacturers’ recommendations.
- Rinse tooth well. Wet cotton rolls or saliva absorbents should be replaced as necessary.
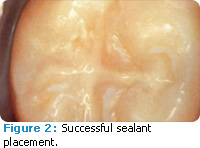
- Air dry tooth surfaces. When completely dry, the tooth structure should have a chalky, frosty-white appearance (Figure 1). If moisture or saliva contamination occurs, re-etch the tooth surface for 15 seconds and dry tooth as previously suggested. Note: some sealants require a moist tooth surface prior to application.
![]()
- Apply the sealant material in accordance with manufacturer recommendations.
- Photopolymerize the material for the recrecommended curing time or allow appropriate curing time for self-cured sealants.
- Remove all isolation materials.
- Completely rinse the area and oral cavity as necessary.
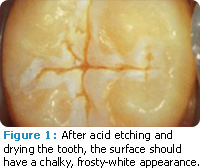
- Dry area, and check sealant integrity and patient’s occlusion with articulating paper; adjust as necessary (Figure 2).
There are variations to this sequence. For example, some manufacturers recommend the application of acid etch or self-etch adhesive prior to sealant placement.
Clinical Recommendations
The use of evidence-based data has become an integral part of clinical dentistry because it allows practitioners to make the best possible decisions for their patients.
In 2008, the ADA published “Evidence-based Clinical Recommendations for the Use of Pit and Fissure Sealants: a Report of the American Dental Association Council On Scientific Affairs.”21 After extensive review of the literature, the panel of experts’ made the following assertions:
- There is strong evidence that resin-based sealants placed on permanent molars of children and adolescents are effective in reducing caries. The use of sealants significantly reduces the incidence of caries. Data show a reduction of 86% at 1 year after sealant placement; 78.6% at 2 years; and 58.6% at 4 years among children and adolescents.21
- Pit and fissure sealants significantly reduce the percentage of noncavitated carious lesions that progress in children, adolescents, and young adults for as long as 5 years following placement. No evidence showed an increase of bacterial growth under sealants.
- Resin-based sealants are the first choice in sealant material because of their high retention rates.
- The use of air abrasion as opposed to acid etching reduces retention rates. There is some evidence that the use of self-etch bonding agents prior to sealant placement improves retention. There is limited evidence that the use of a bur prior to sealant improves retention rates among children.
Caries Risk
Caries risk assessment is key to determining a patient’s need for sealants and their efficacy. Evidence-based data show that placing a sealant over an early carious lesion can reverse the process of decay and eliminate the need for restorative care.22,23 Caries risk assessment should be routinely performed and re-evaluated in order to provide the most effective caries prevention plan.24
Caries diagnosis can be achieved with the traditional means: mirror and explorer or radiography, in addition to new technologies that incorporate light fluorescence or fiber-optic transillumination.25
Conclusion
Sealants are an invaluable component of preventive dentistry, and appropriate steps should be taken to increase their utilization. Dental professionals have all the tools and knowledge necessary to provide the highest quality care. Hopefully these tools will help us achieve or exceed the goals set for sealants by the US Surgeon General’s Healthy People 2020 report.5
REFERENCES
- Untreated Dental Caries in Children Ages 2-19, United States. Available at: www.cdc.gov/Features/dsUntreatedCavitiesKids. Accessed October 11, 2011.
- Feigal RJ. The use of pit and fissure sealants. Pediatr Dent. 2002;24:415-422.
- Beltrán-Aguilar ED, Barker LK, Canto MT, et al. Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis. MMWR Surveillance Summaries. 2005;54:1-44.
- Healthy People 2010: Oral Health. Washington, DC: US Department of Health and Human Services; 2000.
- Healthy People 2020 Summary of Objectives. Available at: www.healthypeople.gov/2020/topicsobjectives2020/pdfs/OralHealth.pdf. Accessed October 11, 2011.
- Hyatt TP. Prophylactic odontotomy: the cutting into the tooth for the prevention of disease. Dental Cosmos. 1923;65:234-241.
- Cueto EI, Buonocore MG. Sealing of pits and fissures with an adhesive resin: its use in caries prevention. J Am Dent Assoc. 1967; 75:121-128.
- Simonsen RJ. Pit and fissure sealant: review of the literature. Pediatr Dent. 2002;24:393-414.
- American Dental Association Council on Dental Materials and Devices. Pit and fissure sealants. J Am Dent Assoc. 1976;93:134.
- Dental sealants in the prevention of tooth decay. Natl Inst Health Consens Dev Conf Summ. 1984;4:9.
- Christensen GJ. The curing light dilemma. J Am Dent Assoc. 2002;133:761-763.
- Yue C, Tantbirojn D, Grothe RL, Versluis A, Hodges JS, Feigal RJ. The depth of cure of clear versus opaque sealants as influenced by curing regimens. J Am Dent Assoc. 2009;140:331-338.
- Beauchamp J, Caufield PW, Crall JJ, et al. Evidencebased clinical recommendations for the use of pitand- fissure sealants: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2008;139:257-268.
- Salar DV, GarcÃa-Godoy F, Flaitz CM, Hicks MJ. Potential inhibition of demineralization in vitro by fluoride-releasing sealants. J Am Dent Assoc. 2007;138:502-506.
- Nathanson D, Lertpitayakun P, Lamkin MS, Edalatpour M, Chou LL. In vitro elution of leachable components from dental sealants. J Am Dent Assoc. 1997;128:1517-1523.
- Fleisch AF, Sheffield PE, Chinn C, et al. Bisphenol A and related compounds in dental materials. Pediatrics. 2010;126:760-768
- Azarpazhooh A, Main PA. Is there a risk of harm or toxicity in the placement of pit and fissure sealant materials? A systematic review. J Can Dent Assoc. 2008;74:179-183.
- Gray SK, Griffin SO, Malvitz DM, Gooch BF. A comparison of the effects of toothbrushing and handpiece prophylaxis on retention of sealants. J Am Dent Assoc. 2009;140:38-46.
- Farsai PS, Uribe S, Katherine WL, Vig KWL. How to clean the tooth surface before sealant application. J Am Dent Assoc. 2010;141:696-698.
- Houpt M, Shey Z. The effectiveness of a fissure sealant after six years. Pediatr Dent. 1983;5:104-106.
- Sasa I, Donly KJ. Sealants: a review of the materials and utilization. J Calif Dent Assoc. 2010;38:730-734.
- Griffin SO, Oong E, Kohn W, et al. The effectiveness of sealants in managing carious lesions. J Dent Res. 2008;87:169-174.
- Oong EM, Griffin SO, Kohn W, Gooch BF, Caufield P. The effect of dental sealants on bacteria levels in caries lesions: a review of the evidence. J Am Dent Assoc. 2008;139:271-278.
- Sasa IS, Donly K. Sealants: a review of the materials and utilization. J Calif Dent. 2010;38:730-734.
- Zandona AF, Zero DT, Diagnostic tools for early caries detection. J Am Dent Assoc. 2006;137:1675-1684.
From Dimensions of Dental Hygiene. November 2011; 9(11): 58, 60-61.